Abstract
Aim
To determine correlation of liver stiffness measured by MR Elastography (MRE) with biliary abnormalities on MR Cholangiopancreatography (MRCP) and MRI parenchymal features in patients with primary sclerosing cholangitis (PSC).
Methods
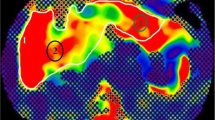
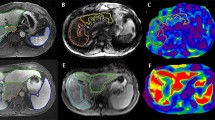
Fifty-five patients with PSC who underwent MRI of the liver with MRCP and MRE were retrospectively evaluated. Two board-certified abdominal radiologists in agreement reviewed the MRI, MRCP, and MRE images. The biliary tree was evaluated for stricture, dilatation, wall enhancement, and thickening at segmental duct, right main duct, left main duct, and common bile duct levels. Liver parenchyma features including signal intensity on T2W and DWI, and hyperenhancement in arterial, portal venous, and delayed phase were evaluated in nine Couinaud liver segments. Atrophy or hypertrophy of segments, cirrhotic morphology, varices, and splenomegaly were scored as present or absent. Regions of interest were placed in each of the nine segments on stiffness maps wherever available and liver stiffness (LS) was recorded. Mean segmental LS, right lobar (V–VIII), left lobar (I–III, and IVA, IVB), and global LS (average of all segments) were calculated. Spearman rank correlation analysis was performed for significant correlation. Features with significant correlation were then analyzed for significant differences in mean LS. Multiple regression analysis of MRI and MRCP features was performed for significant correlation with elevated LS.
Results
A total of 439/495 segments were evaluated and 56 segments not included in MRE slices were excluded for correlation analysis. Mean segmental LS correlated with the presence of strictures (r = 0.18, p < 0.001), T2W hyperintensity (r = 0.38, p < 0.001), DWI hyperintensity (r = 0.30, p < 0.001), and hyperenhancement of segment in all three phases. Mean LS of atrophic and hypertrophic segments were significantly higher than normal segments (7.07 ± 3.6 and 6.67 ± 3.26 vs. 5.1 ± 3.6 kPa, p < 0.001). In multiple regression analysis, only the presence of segmental strictures (p < 0.001), T2W hyperintensity (p = 0.01), and segmental hypertrophy (p < 0.001) were significantly associated with elevated segmental LS. Only left ductal stricture correlated with left lobe LS (r = 0.41, p = 0.018). Global LS correlated significantly with CBD stricture (r = 0.31, p = 0.02), number of segmental strictures (r = 0.28, p = 0.04), splenomegaly (r = 0.56, p < 0.001), and varices (r = 0.58, p < 0.001).
Conclusion
In PSC, there is low but positive correlation between segmental LS and segmental duct strictures. Segments with increased LS show T2 hyperintensity, DWI hyperintensity, and post-contrast hyperenhancement. Global liver stiffness shows a moderate correlation with number of segmental strictures and significantly correlates with spleen stiffness, splenomegaly, and varices.





Similar content being viewed by others
References
Olsson R, Danielsson A, Järnerot G, et al. (1991) Prevalence of primary sclerosing cholangitis in patients with ulcerative colitis. Gastroenterology 100:1319–1323
Loftus EV, Harewood GC, Loftus CG, et al. (2005) PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut 54:91–96
O’Toole A, Alakkari A, Keegan D, et al. (2012) Primary sclerosing cholangitis and disease distribution in inflammatory bowel disease. Clin Gastroenterol Hepatol 10:439–441
Broomé U, Olsson R, Lööf L, et al. (1996) Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut 38:610–615
Ponsioen CY, Chapman RW, Chazouillères O, et al. (2016) Surrogate endpoints for clinical trials in primary sclerosing cholangitis: review and results from an International PSC Study Group consensus process. Hepatology 63:1357–1367
de Vries EM, Verheij J, Hubscher SG, et al. (2015) Applicability and prognostic value of histologic scoring systems in primary sclerosing cholangitis. J Hepatol 63:1212–1219
De Vries EMG, Beuers U, Ponsioen CY (2015) Biomarkers for disease progression of primary sclerosing cholangitis. Curr Opin Gastroenterol 31:239–246
de Vries EM, de Krijger M, Färkkilä M, et al. (2017) Validation of the prognostic value of histologic scoring systems in primary sclerosing cholangitis: an international cohort study. Hepatology 65:907–919
Karlsen TH, Vesterhus M, Boberg KM (2014) Review article: controversies in the management of primary biliary cirrhosis and primary sclerosing cholangitis. Aliment Pharmacol Ther 39:282–301
Majoie CB, Reeders JW, Sanders JB, et al. (1991) Primary sclerosing cholangitis: a modified classification of cholangiographic findings. AJR Am J Roentgenol 157:495–497
Craig DA, MacCarty RL, Wiesner RH, et al. (1991) Primary sclerosing cholangitis: value of cholangiography in determining the prognosis. AJR Am J Roentgenol 157:959–964
Rajaram R, Ponsioen CY, Majoie CB, et al. (2001) Evaluation of a modified cholangiographic classification system for primary sclerosing cholangitis. Abdom Imaging 26:43–47
Bader TR, Beavers KL, Semelka RC (2003) MR imaging features of primary sclerosing cholangitis: patterns of cirrhosis in relationship to clinical severity of disease. Radiology 226:675–685
Ruiz A, Lemoinne S, Carrat F, et al. (2014) Radiologic course of primary sclerosing cholangitis: assessment by three-dimensional magnetic resonance cholangiography and predictive features of progression. Hepatology 59:242–250
Singh S, Venkatesh SK, Wang Z, et al. (2015) Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol 13:440–451
Eaton JE, Dzyubak B, Venkatesh SK, et al. (2016) Performance of magnetic resonance elastography in primary sclerosing cholangitis. J Gastroenterol Hepatol 31:1184–1190
Venkatesh SK, Wang G, Lim SG, et al. (2014) Magnetic resonance elastography for the detection and staging of liver fibrosis in chronic hepatitis B. Eur Radiol 24:70–78
Venkatesh SK, Yin M, Takahashi N, et al. (2015) Non-invasive detection of liver fibrosis: MR imaging features vs. MR elastography. Abdom Imaging 40:766–775
Revelon G, Rashid A, Kawamoto S, et al. (1999) Primary sclerosing cholangitis: MR imaging findings with pathologic correlation. AJR Am J Roentgenol 173:1037–1042
Kim WR, Therneau TM, Wiesner RH, et al. (2000) A revised natural history model for primary sclerosing cholangitis. Mayo Clin Proc 75:688–694
Corpechot C, Gaouar F, El Naggar A, et al. Baseline values and changes in liver stiffness measured by transient elastography are associated with severity of fibrosis and outcomes of patients with primary sclerosing cholangitis. Gastroenterology 2014;146:970–979; quiz e15–6.
Petrovic BD, Nikolaidis P, Hammond NA, et al. (2007) Correlation between findings on MRCP and gadolinium-enhanced MR of the liver and a survival model for primary sclerosing cholangitis. Dig Dis Sci 52:3499–3506
Ni Mhuircheartaigh JM, Lee KS, Curry MP, et al. (2017) Early peribiliary hyperenhancement on MRI in patients with primary sclerosing cholangitis: significance and association with the Mayo risk score. Abdom Radiol (NY) 42:152–158
Venkatesh SK, Wells ML, Miller FH, et al. (2017) Magnetic resonance elastography: beyond liver fibrosis-a case-based pictorial review. Abdom Radiol. https://doi.org/10.1007/s00261-017-1383-1
Acknowledgement
We would like to thank Miranda K. Chamley for her help in data collection, Brent Warndahl for his help with MRI protocol and Dr. Rickey Carter for his advice on statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Richard L. Ehman acknowledges the support of the National Institutes of Health grant (EB001981).
Conflict of Interest
RLE and the Mayo Clinic have a financial interest in MRE technology and hold equity in Resoundant, Inc. All other authors declare that they have no conflict of interest for the above work.
Ethical approval
This is a retrospective study and an Institutional Review Board approval was obtained for review of patient data.
Rights and permissions
About this article
Cite this article
Bookwalter, C.A., Venkatesh, S.K., Eaton, J.E. et al. MR elastography in primary sclerosing cholangitis: correlating liver stiffness with bile duct strictures and parenchymal changes. Abdom Radiol 43, 3260–3270 (2018). https://doi.org/10.1007/s00261-018-1590-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1590-4