Abstract
Purpose
To retrospectively review revised pre-procedural coagulation guidelines for percutaneous liver biopsy to determine whether their implementation is associated with increased hemorrhagic complications on a departmental scale. Secondary endpoints were to determine the effect of this change on pre-procedural blood product (FFP and platelet) utilization, to evaluate the impact of administered blood products on hemorrhagic complications, and to determine whether bleeding complications were related to INR and platelet levels.
Materials and methods
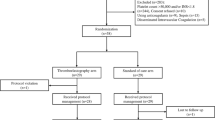
This IRB-approved, HIPAA-compliant, retrospective study reviewed 1846 percutaneous liver biopsies in 1740 patients, comparing biopsies performed, while SIR consensus pre-procedural coagulation guidelines were in place (INR ≤ 1.5, platelets ≥50,000 µL) to those performed after departmental implementation of revised, less stringent guidelines (INR ≤ 2.0, platelets ≥25,000 µL).
Results
On a departmental scale, there were significantly fewer hemorrhagic complications in the population of patients treated after adoption of less stringent guidelines as compared to those treated under the SIR guidelines (1.6% vs. 3.4%, p = 0.0192) despite a significant decrease in pre-procedural FFP (0.8% vs. 3.9%, p < 0.001) and platelet transfusions (0.3% vs. 1.2%, p = 0.021). Individual patient hemorrhagic complication rates significantly increased as INR increased (p = 0.006) and platelet counts decreased (p = 0.004), but pre-procedural FFP (p = 0.64) and/or platelet transfusion (p = 0.5) did not have a significant impact on hemorrhagic complication rates.
Conclusion
Implementation of less stringent pre-procedural coagulation parameter guidelines for percutaneous liver biopsy (INR ≤ 2.0, platelets ≥25,000 µL) did not result in an increase in departmental hemorrhagic complication rates but did significantly decrease pre-procedural FFP/platelet administration. An individual patient’s bleeding risk does increase as INR increases and platelets decrease, but pre-procedural FFP and/or platelet transfusion did not mitigate that increased risk.


Similar content being viewed by others
References
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD (2009) American Association for the Study of Liver D. Liver Biopsy Hepatol 49(3):1017–1044
Gilmore IT, Burroughs A, Murray-Lyon IM, et al. (1995) Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London. Gut 36(3):437–441
McGill DB, Rakela J, Zinsmeister AR, Ott BJ (1990) A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology 99(5):1396–1400
Piccinino F, Sagnelli E, Pasquale G, Giusti G (1986) Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 2(2):165–173
Minuk GY, Sutherland LR, Wiseman DA, MacDonald FR, Ding DL (1987) Prospective study of the incidence of ultrasound-detected intrahepatic and subcapsular hematomas in patients randomized to 6 or 24 hours of bed rest after percutaneous liver biopsy. Gastroenterology 92(2):290–293
Caldwell SH (2001) Controlling pain in liver biopsy, or “we will probably need to repeat the biopsy in a year or two to assess the response”. Am J Gastroenterol 96(5):1327–1329
Patel IJ, Davidson JC, Nikolic B, et al. (2012) Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol 23(6):727–736
Dillon JF, Simpson KJ, Hayes PC (1994) Liver biopsy bleeding time: an unpredictable event. J Gastroenterol Hepatol 9(3):269–271
Gazelle GS, Haaga JR, Rowland DY (1992) Effect of needle gauge, level of anticoagulation, and target organ on bleeding associated with aspiration biopsy. Work in progress. Radiology 183(2):509–513
Ewe K (1981) Bleeding after liver biopsy does not correlate with indices of peripheral coagulation. Dig Dis Sci 26(5):388–393
Terjung B, Lemnitzer I, Dumoulin FL, et al. (2003) Bleeding complications after percutaneous liver biopsy. An analysis of risk factors. Digestion 67(3):138–145
Segal JB, Dzik WH, Transfusion Medicine/Hemostasis Clinical Trials N (2005) Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion 45(9):1413–1425
Mahal AS, Knauer CM, Gregory PB (1981) Bleeding after liver biopsy. West J Med 134(1):11–14
Holland L, Sarode R (2006) Should plasma be transfused prophylactically before invasive procedures? Curr Opin Hematol 13(6):447–451
Gajic O, Dzik WH, Toy P (2006) Fresh frozen plasma and platelet transfusion for nonbleeding patients in the intensive care unit: benefit or harm? Crit Care Med 34(5 Suppl):S170–S173
Yang L, Stanworth S, Hopewell S, Doree C, Murphy M (2012) Is fresh-frozen plasma clinically effective? An update of a systematic review of randomized controlled trials. Transfusion 52(8):1673–1686 (quiz)
Stanworth SJ, Brunskill SJ, Hyde CJ, McClelland DB, Murphy MF (2004) Is fresh frozen plasma clinically effective? A systematic review of randomized controlled trials. Br J Haematol 126(1):139–152
O’Connor SD, Taylor AJ, Williams EC, Winter TC (2009) Coagulation concepts update. AJR Am J Roentgenol 193(6):1656–1664
Institute NC (2009) Common Terminology Criteria for Adverse Events v4.0.
R Development Core Team (2013) R: a language and environment for statistical computing. R Foundation for Statistical Computing V, Austria. ISBN 3-900051-07-0. http://www.R-project.org.
McInnes MD, Kielar AZ, Macdonald DB (2011) Percutaneous image-guided biopsy of the spleen: systematic review and meta-analysis of the complication rate and diagnostic accuracy. Radiology 260(3):699–708
Domen RE, Hoeltge GA (2003) Allergic transfusion reactions: an evaluation of 273 consecutive reactions. Arch Pathol Lab Med 127(3):316–320
Kleinman S, Caulfield T, Chan P, et al. (2004) Toward an understanding of transfusion-related acute lung injury: statement of a consensus panel. Transfusion 44(12):1774–1789
Popovsky MA, Moore SB (1985) Diagnostic and pathogenetic considerations in transfusion-related acute lung injury. Transfusion 25(6):573–577
FDA (2010) Fatalities reported to FDA following blood collection and transfusion
Narick C, Triulzi DJ, Yazer MH (2012) Transfusion-associated circulatory overload after plasma transfusion. Transfusion 52(1):160–165
Görlinger K, Saner F (2015) Prophylactic plasma and platelet transfusion in the critically Ill patient: just useless and expensive or even harmful? BMC Anesthesiol 15:86
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. Louis Hinshaw: Shareholder and Consultant for NeuWave Medical, a company which manufactures microwave ablation technology. Shareholder, Novleos, a company which manufactures tumor radiopharmaceuticals. All others—none.
Rights and permissions
About this article
Cite this article
Kitchin, D.R., del Rio, A.M., Woods, M. et al. Percutaneous liver biopsy and revised coagulation guidelines: a 9-year experience. Abdom Radiol 43, 1494–1501 (2018). https://doi.org/10.1007/s00261-017-1319-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1319-9