Abstract
Purpose
To evaluate preoperative CT features that predict the development of postoperative inguinal hernia after robot-assisted laparoscopic radical prostatectomy (RALRP).
Methods
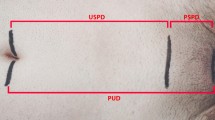
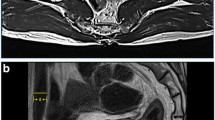
We enrolled 160 men who underwent CT, subsequent RALRP, and at least three years of follow-up. CT was retrospectively reviewed in consensus by two radiologists for the presence of asymmetric spermatic cord fat and scrotal fluid collection. The diagnostic power of each CT feature for the development of postoperative inguinal hernia was calculated. Multiple logistic regression was performed to evaluate the association between CT features, clinical variables, and postoperative inguinal hernia.
Results
Surgically confirmed postoperative inguinal hernia developed in 17 patients. Asymmetric spermatic cord fat was demonstrated in 13 patients, and scrotal fluid collection was seen in 59 patients. The diagnostic values of asymmetric spermatic cord fat and scrotal fluid collection for postoperative inguinal hernia were 58.8% and 88.2% sensitivity, 97.9% and 69.2% specificity, 76.9% and 25.4% positive predictive value, 95.2% and 98.0% negative predictive value, and 93.8% and 71.3% accuracy, respectively. On multiple logistic regression analysis, asymmetric spermatic cord fat, scrotal fluid collection, and low BMI were significant predictive factors for the development of postoperative inguinal hernia (odds ratios: 135.8, 31.6, and 0.7, respectively).
Conclusion
The presence of asymmetric spermatic cord fat or scrotal fluid collection was significantly associated with the development of postoperative inguinal hernia.


Similar content being viewed by others
References
Heidenreich A, Bellmunt J, Bolla M, et al. (2011) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 59:61–71
Zhu S, Zhang H, Xie L, et al. (2013) Risk factors and prevention of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol 189:884–890
Lee DH, Jung HB, Chung MS, et al. (2013) Patent processus vaginalis in adults who underwent robot-assisted laparoscopic radical prostatectomy: Predictive signs of postoperative inguinal hernia in the internal inguinal floor. Int J Urol 20:177–182
Stranne J, Lodding P (2011) Inguinal hernia after radical retropubic prostatectomy: risk factors and prevention. Nat Rev Urol 8:267–273
Arai Y, Egawa S, Tobisu K, et al. (2000) Radical retropubic prostatectomy: time trends, morbidity and mortality in Japan. BJU Int 85:287–294
Twu C-M, Ou Y-C, Yang C-R, et al. (2005) Predicting risk factors for inguinal hernia after radical retropubic prostatectomy. Urology 66:814–818
Regan TC, Mordkin RM, Constantinople NL, et al. (1996) Incidence of inguinal hernias following radical retropubic prostatectomy. Urology 47:536–537
Rosemar A, Angerås U, Rosengren A (2008) Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg 247:1064–1068
Lee DH, Koo KC, Lee SH, et al. (2014) A simple procedure to prevent postoperative inguinal hernia after robot-assisted laparoscopic radical prostatectomy: a plugging method of the internal inguinal floor for patients with patent processus vaginalis. J Urol 191:468–472
Fukuta F, Hisasue S, Yanase M, et al. (2006) Preoperative computed tomography finding predicts for postoperative inguinal hernia: new perspective for radical prostatectomy-related inguinal hernia. Urology 68:267–271
Stranne J, Hugosson J, Lodding P (2007) Inguinal hernia is a common complication in lower midline incision surgery. Hernia 11:247–252
Ichioka K, Yoshimura K, Utsunomiya N, et al. (2004) High incidence of inguinal hernia after radical retropubic prostatectomy. Urology 63:278–281
Holcomb GW, Brock JW, Morgan WM (1994) Laparoscopic evaluation for a contralateral patent processus vaginalis. J Pediatr Surg 29:970–974
Nomura T, Mimata H, Kitamura H, et al. (2005) Lower incidence of inguinal hernia: minilaparotomy radical retropubic prostatectomy compared with conventional technique. A preliminary report. Urol Int 74:32–37
Stranne J, Johansson E, Nilsson A, et al. (2010) Inguinal hernia after radical prostatectomy for prostate cancer: results from a randomized setting and a nonrandomized setting. Eur Urol 58:719–726
McDonald D, Huggins C (1949) Simultaneous prostatectomy and inguinal herniorrhaphy. Surg Gynecol Obstet 89:621
Fujii Y, Yamamoto S, Yonese J, et al. (2014) The processus vaginalis transection method to prevent postradical prostatectomy inguinal hernia: long-term results. Urology 83:247–252
van Veen RN, van Wessem KJ, Halm JA, et al. (2007) Patent processus vaginalis in the adult as a risk factor for the occurrence of indirect inguinal hernia. Surg Endosc 21:202–205
Wechsler RJ, Kurtz AB, Needleman L, et al. (1989) Cross-sectional imaging of abdominal wall hernias. AJR Am J Roentgenol 153:517–521
Valentino M, Bertolotto M, Ruggirello M, et al. (2011) Cystic lesions and scrotal fluid collections in adults: Ultrasound findings. J Ultrasound 14:208–215
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study received no funding support.
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was waived by the institutional review board.
Rights and permissions
About this article
Cite this article
Sim, K.C., Sung, D.J., Han, N.Y. et al. Preoperative CT findings of subclinical hernia can predict for postoperative inguinal hernia following robot-assisted laparoscopic radical prostatectomy. Abdom Radiol 43, 1231–1236 (2018). https://doi.org/10.1007/s00261-017-1270-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1270-9