Abstract
Purpose
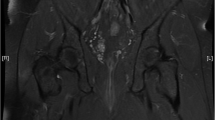
Though perianal fistulas are commonly seen in patients with Crohn’s disease, they can also be seen in patients without inflammatory bowel disease. The purpose of this study was to evaluate MR imaging differences of perianal fistulas in patients with and without Crohn’s disease.
Methods
Our retrospective search from January 2012 to December 2015 of the Radiology database for perianal fistula yielded 207 patients. Only patients with dedicated MR fistula protocol studies were included, whereas patients with previous anal surgery or anastomosis, anorectal tumors, and equivocal findings that could not be definitely assessed as a fistula were excluded. The following features were assessed: anatomic type of fistula (Parks Classification), luminal origin (hour clock position), anal verge distance, signs of acute inflammation, circumference of anus involved by inflammation, presence of rectal inflammation. and abscess.
Results
One hundred and twenty six of 207 patients met inclusion criteria. Of these, 96 (76.2%) had Crohn’s disease and 30 (23.8%) did not. The most common fistulas identified were transphincteric (38.5% of Crohn’s and 50% of non-Crohn’s) and intersphincteric (33.3% of Crohn’s and 35.4% of non-Crohn’s). An abscess was associated in 41 cases, 32 (33.3%) in the Crohn’s group and 9 (30.0%) in the non-Crohn’s group. Rectal inflammation was present in 29 patients with Crohn’s disease (29.2%) and in 2 without Crohn’s (6.7%). This finding was statistically significant (p = 0.0009).
Conclusions
Our study demonstrates that while both groups can have similar MR imaging features, accompanying rectal inflammation was more commonly seen in Crohn’s disease.




Similar content being viewed by others
References
Zanotti C, Martinez-Puente C, Pascual I, et al. (2007) An assessment of the incidence of fistula-in-ano in four countries of the European Union. Int J Colorectal Dis 22:1459–1462
Sainio P (1984) Fistula-in-ano in a defined population: incidence and epidemiological aspects. Ann Chir Gynaecol 73(4):219–224
Criado JM, del Salto LG, Rivas PF, et al. (2012) MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics 32:175–194
O’Malley RB, Al-Hawary MM, Kaza RK, et al. (2012) Rectal imaging: part 2, perianal fistula evaluation on Plevic MRI—what the radiologist needs to know. Am J Roentgenol 199:W43–W53
Beets-Tan RGH, Beets GL, van der Hoop AG, et al. (2001) Preoperative MR imaging of anal fistulas: does it really help the surgeon. Radiology 218:75–84
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of Fistula-in-ano. Br J Surg 63:1–12
Szurowska E, Wypych J, Izycka-Swieszewska E (2007) Perianal fistulas in Crohn’s disease: MRI diagnosis and surgical planning. Abdom Imaging 32:705–718
Villa C, Pompili G, Franceschelli G, et al. (2012) Role of magnetic resonance imaging in evaluation of the activity of perianal Crohn’s disease. Eur J Radiol 81:616–622
Plumb AA, Halligan S, Bhatnagar G, Taylor SA (2015) Perianal sepsis in hematologic malignancy: MR imaging appearances and distinction from cryptoglandular infection in immunocompetent patients. Radiology 276:147–155
Vanbeckevoort D, Bielen D, Vanslembrouck R, Van Assche G (2014) Magnetic resonance imaging of perianal fistulas. Magn Reson Imaging Clin N Am 22:113–123
Halligan S, Stoker J (2006) State of the art: imaging of fistula in ano. Radiology 239(1):18–33
Sneider EB, Maykel JA (2013) Anal abscess and fistula. Gastroenterol Clin N Am 42:773–784
Schwartz DA, Loftus EV Jr, Tremaine WJ, et al. (2002) The natural history of fistulizing Crohn’s disease in Olmsted County. Minnesota. Gastroenterology 122:875–880
Morris J, Spencer JA, Ambrose NS (2000) MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 20:623–635
Ong EMW, Ghazi LJ, Schwartz DA, Mortele KJ (2015) Guidelines for imaging of Crohn’s perianal fistulizing disease. Inflamm Bowel Dis 21(4):731–736
Gecse KB, Bemelman W, Kamm MA, et al. (2014) A global consensus on the classification, diagnosis and multidisciplinary treatment of perianal fistulising Crohn’s disease. Gut 63:1381–1392
Schwartz DA, Ghazi LJ, Regueiro M, et al. (2015) Guidelines for the multidisciplinary management of Crohn’s perianal fistulas: summary statement. Inflamm Bowel Dis 21(4):723–730
Rosa G, Lolli P, Piccinelli D, Mazzola F, Bonomo S (2006) Fistula-in-ano: anatomoclinical aspects, surgical therapy and results in 844 patients. Tech Coloproctol 10:215–221
Zbar AP, Horesh N, Bucholtz V, et al. (2013) Are there specific endosonographic features in Crohn’s patients with perianal fistulae? J Crohn’s Colitis 7:490–496
Lichtenstein GR, Hanauer SB, Sandborn W (2009) J and the Practice Parameters Committee of the American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol 104:465–483
Acknowledgements
Aoife Kilcoyne would like to acknowledge the support of the Mac Erlaine Scholarship, from the Academic Radiology Research Trust, St. Vincent’s Radiology Group, Dublin, Ireland. Irai S Oliveira would like to acknowledge the support of the Instituto de Ensino e Pesquisa, from Hospital Sírio-Libanês, São Paulo, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed consent
This HIPAA compliant study was approved by Institutional Review Board (IRB) and a waiver of informed consented was obtained.
Rights and permissions
About this article
Cite this article
Oliveira, I.S., Kilcoyne, A., Price, M.C. et al. MRI features of perianal fistulas: is there a difference between Crohn’s and non-Crohn’s patients?. Abdom Radiol 42, 1162–1168 (2017). https://doi.org/10.1007/s00261-016-0989-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0989-z