Abstract
Purpose
Identifying liver metastases from neuroendocrine tumors (NETs) is a pretherapeutic challenge in patients who are candidates for liver resection. The aims of our study are to characterize and determine the frequency of different MRI characteristics of liver metastases caused by NETs in a lesion-by-lesion analysis and to determine the frequency of monomorphous and polymorphous metastases in a patient-by-patient analysis.
Methods
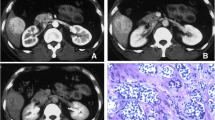
This retrospective study involved 47 patients with liver metastases arising from histologically confirmed NETs. In a lesion-by-lesion analysis, we classified these metastases according to their MRI characteristics as follows: hypervascular lesions with homogeneous or peripheral enhancement, hypovascular lesions, pure cystic lesions, and mixed solid/cystic lesions. In the patient-by-patient analysis, we distinguished patients whose metastases had the same MRI characteristics from patients with mixed lesion characteristics.
Results
A total of 376 metastases were analyzed. Of these, 84.3% (n = 317) were hypervascular, with 51.9% showing homogeneous enhancement and 32.4% (n = 122) showing peripheral enhancement. Another 7.4% (n = 28) were hypovascular, 5.3% (n = 20) were pure cystic, and 2.9% (n = 11) were mixed solid/cystic. After excluding three patients with solitary lesions, 40.9% of patients (n = 18) had mixed-type lesions, consisting of hypervascular lesions with either homogeneous or peripheral enhancement in 27.3% of cases (n = 12), while 59.1% of patients (n = 26) had identical lesions.
Conclusion
Approximately 15% of metastases have atypical MRI characteristics and are either hypovascular or cystic. Metastases with different MRI characteristics coexist in 40% of patients.







Similar content being viewed by others
References
Pape U-F, Berndt U, Müller-Nordhorn J, et al. (2008) Prognostic factors of long-term outcome in gastroenteropancreatic neuroendocrine tumours. Endocr Relat Cancer 15:1083–1097. doi:10.1677/ERC-08-0017
Lombard-Bohas C, Mitry E, O’Toole D, et al. (2009) Thirteen-month registration of patients with gastroenteropancreatic endocrine tumours in France. Neuroendocrinology 89:217–222. doi:10.1159/000151562
Steinmüller T, Kianmanesh R, Falconi M, et al. (2008) Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 87:47–62
Yao JC, Hassan M, Phan A, et al. (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26:3063–3072. doi:10.1200/JCO.2007.15.4377
Pape U-F, Jann H, Müller-Nordhorn J, et al. (2008) Prognostic relevance of a novel TNM classification system for upper gastroenteropancreatic neuroendocrine tumors. Cancer 113:256–265. doi:10.1002/cncr.23549
Dromain C, de Baere T, Lumbroso J, et al. (2005) Detection of liver metastases from endocrine tumors: a prospective comparison of somatostatin receptor scintigraphy, computed tomography, and magnetic resonance imaging. J Clin Oncol 23:70–78. doi:10.1200/JCO.2005.01.013
Dromain C, de Baere T, Baudin E, et al. (2003) MR imaging of hepatic metastases caused by neuroendocrine tumors: comparing four techniques. AJR Am J Roentgenol 180:121–128. doi:10.2214/ajr.180.1.1800121
Danet I-M, Semelka RC, Leonardou P, et al. (2003) Spectrum of MRI appearances of untreated metastases of the liver. AJR Am J Roentgenol 181:809–817. doi:10.2214/ajr.181.3.1810809
Denecke T, Baur AD, Ihm C, et al. (2013) Evaluation of radiological prognostic factors of hepatic metastases in patients with non-functional pancreatic neuroendocrine tumors. Eur J Radiol 82:e550–e555. doi:10.1016/j.ejrad.2013.06.017
Fiori S, Del Gobbo A, Gaudioso G, et al. (2013) Hepatic pseudocystic metastasis of well-differentiated ileal neuroendocrine tumor: a case report with review of the literature. Diagn Pathol 8:148. doi:10.1186/1746-1596-8-148
Salamone L, McCarthy S, Salem RR (2010) Atypical cystic carcinoid tumors of the liver. J Clin Gastroenterol 44:e256–e259. doi:10.1097/MCG.0b013e3181da7714
Soyer P, Boudiaf M, Placé B, et al. (2011) Preoperative detection of hepatic metastases: comparison of diffusion-weighted, T2-weighted fast spin echo and gadolinium-enhanced MR imaging using surgical and histopathologic findings as standard of reference. Eur J Radiol 80:245–252. doi:10.1016/j.ejrad.2010.06.027
Hardie AD, Naik M, Hecht EM, et al. (2010) Diagnosis of liver metastases: value of diffusion-weighted MRI compared with gadolinium-enhanced MRI. Eur Radiol 20:1431–1441. doi:10.1007/s00330-009-1695-9
d’Assignies G, Fina P, Bruno O, et al. (2013) High sensitivity of diffusion-weighted MR imaging for the detection of liver metastases from neuroendocrine tumors: comparison with T2-weighted and dynamic gadolinium-enhanced MR imaging. Radiology 268:390–399. doi:10.1148/radiol.13121628
Soyer P, Gueye C, Somveille E, Laissy JP, Scherrer A (1995) MR diagnosis of hepatic metastases from neuroendocrine tumors versus hemangiomas: relative merits of dynamic gadolinium chelate-enhanced gradient-recalled echo and unenhanced spin-echo images. AJR Am J Roentgenol 165:1407–1413. doi:10.2214/ajr.165.6.7484575
Paulson EK, McDermott VG, Keogan MT, et al. (1998) Carcinoid metastases to the liver: role of triple-phase helical CT. Radiology 206:143–150. doi:10.1148/radiology.206.1.9423664
Bader TR, Semelka RC, Chiu VC, Armao DM, Woosley JT (2001) MRI of carcinoid tumors: spectrum of appearances in the gastrointestinal tract and liver. J Magn Reson Imaging 14:261–269. doi:10.1002/jmri.1182
Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S (2010) The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas 39:707–712. doi:10.1097/MPA.0b013e3181ec124e
Elias D, Lefevre JH, Duvillard P, et al. (2010) Hepatic metastases from neuroendocrine tumors with a “thin slice” pathological examination: they are many more than you think. Ann Surg 251:307–310. doi:10.1097/SLA.0b013e3181bdf8cf
Hentic O, Couvelard A, Rebours V, et al. (2011) Ki-67 index, tumor differentiation, and extent of liver involvement are independent prognostic factors in patients with liver metastases of digestive endocrine carcinomas. Endocr Relat Cancer 18:51–59. doi:10.1677/ERC-09-0319
Guyennon A, Mihaila M, Palma J, et al. (2010) Perfusion characterization of liver metastases from endocrine tumors: computed tomography perfusion. World J Radiol 2:449–454. doi:10.4329/wjr.v2.i11.449
Lawrence B, Gustafsson BI, Chan A, et al. (2011) The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 40:1–18. doi:10.1016/j.ecl.2010.12.005
Wijesuriya S, Siriwardana R, Deen K (2010) Hepatobiliary and pancreatic: carcinoid tumor with cystic liver metastases. J Gastroenterol Hepatol 25:647–647. doi:10.1111/j.1440-1746.2010.06290.x
Sugawara Y, Yamamoto J, Yamasaki S, et al. (2000) Cystic liver metastases from colorectal cancer. J Surg Oncol 74:148–152.10.1002/1096-9098(200006)74:2<148::AID-JSO13>3.0.CO;2-N
Pavel M, Baudin E, Couvelard A, et al. (2012) ENETS consensus guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 95:157–176. doi:10.1159/000335597
Frilling A, Modlin IM, Kidd M, et al. (2014) Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol 15:e8–21. doi:10.1016/S1470-2045(13)70362-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Informed consent
The Institutional Review Board approved the study and did not require additional informed consent for reviewing the patients’ medical records and images.
Rights and permissions
About this article
Cite this article
Milin, S., Brunaud, L., Orry, X. et al. Prevalence of hepatic lesion types defined by T2-weighted and dynamic gadolinium-enhanced MR imaging in patients with metastasized neuroendocrine tumors. Abdom Radiol 41, 2132–2141 (2016). https://doi.org/10.1007/s00261-016-0814-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0814-8