Abstract
Objective
Primary hepatic neuroendocrine tumor (PHNET) is an extremely rare liver neoplasm, and its clinical characteristics and imaging features are not well understood. The aim of this study was to analyze the clinical profiles and imaging features of PHNETs on contrast-enhanced ultrasound (CEUS) and computed tomography (CT)
Methods
Patients with PHNET between January 2008 and December 2015 were retrospectively identified, and their demographics, laboratory data, and imaging characteristics on CEUS and CT analyzed.
Results
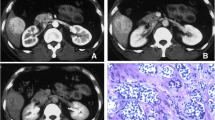
Ten consecutive patients with PHNETs were included (including one G1, seven G2, and two G3 of tumor grades).The median age of patient was 45 years (range: 27–72 years), and 60.0% of patients were male. The most common symptom was abdominal pain (60.0%), and cirrhosis was found in 40.0% of patients. Tumors were confined within the liver in 60.0% of patients, while the remaining patients had extra-hepatic metastasis. The tumors revealed hyperechoic in 60% of patients and mixed echoic in 30% of patients on conventional US, displaying intense arterial enhancement followed by washout in the portal and/or the late phases in 80.0% of patients on CEUS and 60% at CT.
Conclusions
Although PHNET is a very rare liver tumor, it should be considered as a possible differential diagnosis in the management of hepatic tumors. Most PHNETs were hyperechoic or mixed echoic on conventional US, showing similar enhancement patterns to that of hepatocellular carcinoma on CEUS.



Similar content being viewed by others
Abbreviations
- PHNET:
-
Primary hepatic neuroendocrine tumor
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- AFP:
-
α–fetoprotein
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- GGT:
-
γ-glutamyl transpeptidase
- EFSUMB:
-
European Federation of Societies for Ultrasound in medicine and Biology
References
Kloppel G, Perren A, Heitz PU (2004) The gastroenteropancreatic neuroendocrine cell system and its tumors: the WHO classification. Ann N Y Acad Sci 1014:13–27
Yao JC, Hassan M, Phan A, et al. (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26(18):3063–3072
Huang YQ, Xu F, Yang JM, et al. (2010) Primary hepatic neuroendocrine carcinoma: clinical analysis of 11 cases. Hepatobiliary Pancreat Dis Int 9(1):44–48
van der Hoef M, Crook DW, Marincek B, et al. (2004) Primary neuroendocrine tumors of the liver: MRI features in two cases. Abdom Imaging 29(1):77–81
Kong W, Qiu Y, Zhang W, et al. (2008) Diagnosis of primary hepatic carcinoid tumor: report of one case. Chin-Ger J Clin Oncol 7(11):673–675
Chen Z, Xiao HE, Ramchandra P, et al. (2014) Imaging and pathological features of primary hepatic neuroendocrine carcinoma: an analysis of nine cases and review of the literature. Oncol Lett 7(4):956–962
Claudon M, Dietrich CF, Choi BI, et al. (2013) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver–update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM FLAUS and ICUS. Ultraschall Med 34(1):11–29
Bosman FT, Carmeiro F, Hruban RH, et al. (2010) WHO classification of tumours of the digestive system. Lyon: International Agency for Research on Cancer
Claudon M, Cosgrove D, Albrecht T, et al. (2008) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update 2008. Ultraschall Med 29(1):28–44
Lin CW, Lai CH, Hsu CC, et al. (2009) Primary hepatic carcinoid tumor: a case report and review of the literature. Cases J 2(1):90
Soga J (2002) Primary hepatic endocrinomas (carcinoids and variant neoplasms). A statistical evaluation of 126 reported cases. J Exp Clin Cancer Res 21(4):457–468
Iwao M, Nakamuta M, Enjoji M, et al. (2001) Primary hepatic carcinoid tumor: case report and review of 53 cases. Med Sci Monit 7(4):746–750
Iimuro Y, Deguchi Y, Ueda Y, et al. (2002) Primary hepatic carcinoid tumor with metachronous lymph node metastasis after long-term follow up. J Gastroenterol Hepatol 17(10):1119–1124
Donadon M, Torzilli G, Palmisano A, et al. (2006) Liver resection for primary hepatic neuroendocrine tumours: report of three cases and review of the literature. Eur J Surg Oncol 32(3):325–328
de Liguori CN, Manzia TM, Tariciotti L, et al. (2009) Liver transplantation in primary hepatic carcinoid tumor: case report and literature review. Transpl Proc 41(4):1386–1389
Park CH, Chung JW, Jang SJ, et al. (2012) Clinical features and outcomes of primary hepatic neuroendocrine carcinomas. J Gastroenterol Hepatol 27(8):1306–1311
Eisenhauer EA, Therasse P, Bogaerts J, et al. (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247
Massironi S, Conte D, Sciola V, et al. (2010) Contrast-enhanced ultrasonography in evaluating hepatic metastases from neuroendocrine tumours. Dig Liver Dis 42(9):635–641
Hoeffel C, Job L, Ladam-Marcus V, et al. (2009) Detection of hepatic metastases from carcinoid tumor: prospective evaluation of contrast-enhanced ultrasonography. Dig Dis Sci 54(9):2040–2046
Mork H, Ignee A, Schuessler G, et al. (2007) Analysis of neuroendocrine tumour metastases in the liver using contrast enhanced ultrasonography. Scand J Gastroenterol 42(5):652–662
Schutte K, Bornschein J, Malfertheiner P (2009) Hepatocellular carcinoma–epidemiological trends and risk factors. Dig Dis 27(2):80–92
Boozari B, Soudah B, Rifai K, et al. (2011) Grading of hypervascular hepatocellular carcinoma using late phase of contrast enhanced sonography—a prospective study. Dig Liver Dis 43(6):484–490
Kim JE, Lee WJ, Kim SH, et al. (2011) Three-phase helical computed tomographic findings of hepatic neuroendocrine tumors: pathologic correlation with revised WHO Classification. J Comput Assist Tomogr 35:697Y702
Paulson EK, McDermott VG, Keogan MT, et al. (1998) Carcinoid metastases to the liver: role of triple-phase helical CT. Radiology 206:143Y150
Donica H, Malecha-Jedraszek A, Stroslawska E, et al. (2010) Significance of plasma chromogranin A determination in neuroendocrine tumour (NET) diagnosis. Folia Histochem Cytobiol 48(4):603–610
Authors’ contributions
RL designed, planned, and coordinated the study, interpreted the results of CEUS, drafted the manuscript and revised it. CLT collected CEUS data. DY collected CT data and clinical data. XH Z interpreted CEUS images. PC interpreted images of CT. KSM interpreted clinical data, and performed liver surgery and biopsy. DYG interpreted the pathology of PHNET tumor. SYD interpreted images of CT
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rui Li, Chun-Lin Tang, Dan Yang, Xiao-Hang Zhang, Ping Cai, Kuan-Sheng Ma, De-Yu Guo, and Shi-Yi Ding declare that they have no conflict of interest.
Ethical approval
Institutional review board approval for this study was obtained from the ethics committee of Southwest hospital
Results involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The need for informed consent of patient was waived by the ethics committee of Southwest hospital in this retrospective study.
Rights and permissions
About this article
Cite this article
Li, R., Tang, CL., Yang, D. et al. Primary hepatic neuroendocrine tumors: clinical characteristics and imaging features on contrast-enhanced ultrasound and computed tomography. Abdom Radiol 41, 1767–1775 (2016). https://doi.org/10.1007/s00261-016-0770-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0770-3