Abstract
Purpose
To compare liver lesion volume measurement on multiple 3D software platforms using a liver phantom.
Methods
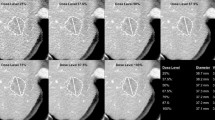
An anthropomorphic phantom constructed with ten liver lesions of varying size, attenuation, and shape with known volume and long axis measurement was scanned (120 kVp, 80–440 smart mA, NI 12). DICOM data were uploaded to five commercially available 3D visualization systems and manual tumor volume was obtained by three-independent readers. Accuracy and reproducibility of linear and volume measurements were compared. The two most promising systems were then compared with an additional prototype system by two readers using both manual and semi-automated measurement with similar comparison between linear and volume measures. Measurements were performed on 5- and 1.25-mm data sets. Inter- and intra-observer variability was also assessed.
Results
Overall mean % volume error on the five commercially available software systems (averaging all ten liver lesions among all three readers) was 8.0% ± 7.5%, 13.7% ± 11.2%, 14.2% ± 15.2%, 16.4% ± 14.8 %, and 16.9% ± 13.8%, varying almost twofold across vendor. Moderate inter-observer variability was present. Volume measurement was slightly more accurate than linear measurement, but linear measurement was more reproducible across readers and systems. On the two “best” systems, the manual measurement method was more accurate than the automated method (p = 0.001). The prototype system demonstrated superior semi-automated assessment, with a mean % volume error of 5.3% ± 4.1% (vs. 17.8% ± 11.1% and 31.5% ± 19.7%, p < 0.001), with improved inter- and intra-observer variability.
Conclusions
Accuracy and reproducibility of volume assessment of liver lesions varies significantly by vendor, which has important implications for clinical use.





Similar content being viewed by others
References
Paesmans M, Sculier JP, Libert P, et al. (1997) Response to chemotherapy has predictive value for further survival of patients with advanced non-small cell lung cancer: 10 years experience of the European Lung Cancer Working Party. Eur J Cancer 33:2326–2332
Buyse M, Thirion P, Carlson RW, et al. (2000) Relation between tumour response to first-line chemotherapy and survival in advanced colorectal cancer: a meta-analysis. Meta-Analysis Group in Cancer. Lancet 356:373–378
Goffin J, Baral S, Tu D, Nomikos D, Seymour L (2005) Objective responses in patients with malignant melanoma or renal cell cancer in early clinical studies do not predict regulatory approval. Clin Cancer Res 11:5928–5934
El-Maraghi RH, Eisenhauer EA (2008) Review of phase II trial designs used in studies of molecular targeted agents: outcomes and predictors of success in phase III. J Clin Oncol 26:1346–1354
Therasse P, Arbuck SG, Eisenhauer EA, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Eisenhauer EA, Therasse P, Bogaerts J, et al. (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Arimoto T (1993) Significance of computed tomography-measured volume in the prognosis of cervical carcinoma. Cancer 72:2383–2388
Chen SW, Yang SN, Liang JA, Lin FJ, Tsai MH (2009) Prognostic impact of tumor volume in patients with stage III–IVA hypopharyngeal cancer without bulky lymph nodes treated with definitive concurrent chemoradiotherapy. Head Neck 31:709–716
Yeo SG, Kim DY, Park JW, et al. (2011) Tumor volume reduction rate after preoperative chemoradiotherapy as a prognostic factor in locally advanced rectal cancer. Int J Radiat Oncol Biol Phys 18(13):3686–3693. doi:10.1245/s10434-011-1822-0
Kim YC, Lim JS, Keum KC, et al. (2011) Comparison of diffusion-weighted MRI and MR volumetry in the evaluation of early treatment outcomes after preoperative chemoradiotherapy for locally advanced rectal cancer. J Mag Reson Imaging: JMRI 34(3):570–576. doi:10.1002/jmri.22696
Hopper KD, Kasales CJ, Eggli KD, et al. (1996) The impact of 2D versus 3D quantitation of tumor bulk determination on current methods of assessing response to treatment. J Comput Assist Tomogr 20:930–937
Pickhardt PJ, Lehman VT, Winter TC, Taylor AJ (2006) Polyp volume versus linear size measurements at CT colonography: implications for noninvasive surveillance of unresected colorectal lesions. AJR Am J Roentgenol 186:1605–1610
Prasad SR, Jhaveri KS, Saini S, et al. (2002) CT tumor measurement for therapeutic response assessment: comparison of unidimensional, bidimensional, and volumetric techniques initial observations. Radiology 225:416–419
Sargent DJ, Rubinstein L, Schwartz L, et al. (2009) Validation of novel imaging methodologies for use as cancer clinical trial end-points. Eur J Cancer 45:290–299
Hillman SL, An MW, O’Connell MJ, et al. (2009) Evaluation of the optimal number of lesions needed for tumor evaluation using the response evaluation criteria in solid tumors: a north central cancer treatment group investigation. J Clin Oncol 27:3205–3210
Bolte H, Riedel C, Muller-Hulsbeck S, et al. (2007) Precision of computer-aided volumetry of artificial small solid pulmonary nodules in ex vivo porcine lungs. Br J Radiol 80:414–421
Buckler AJ, Mozley PD, Schwartz L, et al. (2010) Volumetric CT in lung cancer: an example for the qualification of imaging as a biomarker. Acad Radiol 17:107–115
Erasmus JJ, Gladish GW, Broemeling L, et al. (2003) Interobserver and intraobserver variability in measurement of non-small-cell carcinoma lung lesions: implications for assessment of tumor response. J Clin Oncol 21:2574–2582
Hein PA, Romano VC, Rogalla P, et al. (2009) Linear and volume measurements of pulmonary nodules at different CT dose levels: intrascan and interscan analysis. RoFo 181:24–31
Marchiano A, Calabro E, Civelli E, et al. (2009) Pulmonary nodules: volume repeatability at multidetector CT lung cancer screening. Radiology 251:919–925
Marten K, Engelke C (2007) Computer-aided detection and automated CT volumetry of pulmonary nodules. Eur Radiol 17:888–901
Mozley PD, Schwartz LH, Bendtsen C, et al. (2010) Change in lung tumor volume as a biomarker of treatment response: a critical review of the evidence. Ann Oncol 21:1751–1755
Wormanns D, Kohl G, Klotz E, et al. (2004) Volumetric measurements of pulmonary nodules at multi-row detector CT: in vivo reproducibility. Eur Radiol 14:86–92
Costello P, Duszlak EJ, Lokich J, Matelski H, Clouse ME (1983) Assessment of tumor response by computed tomography liver volumetry. J Comput Tomogr 7:323–326
De Vriendt G, Rigauts H, Meeus L (1998) A semi-automated program for volume measurement in focal hepatic lesions: a first clinical experience. J Belg Radiol 81:181–183
Fabel M, Bolte H, von Tengg-Kobligk H, et al. (2011) Semi-automated volumetric analysis of lymph node metastases during follow-up: initial results. Eur Radiol 21:683–692
Fabel M, von Tengg-Kobligk H, Giesel FL, et al. (2008) Semi-automated volumetric analysis of lymph node metastases in patients with malignant melanoma stage III/IV: a feasibility study. Eur Radiol 18:1114–1122
Keil S, Behrendt FF, Stanzel S, et al. (2008) Semi-automated measurement of hyperdense, hypodense and heterogeneous hepatic metastasis on standard MDCT slices. Comparison of semi-automated and manual measurement of RECIST and WHO criteria. Eur Radiol 18:2456–2465
Keil S, Bruners P, Ohnsorge L, et al. (2010) Semiautomated versus manual evaluation of liver metastases treated by radiofrequency ablation. J Vascular Interv Radiol: JVIR 21:245–251
Keil S, Plumhans C, Behrendt FF, et al. (2009) Semi-automated quantification of hepatic lesions in a phantom. Invest Radiol 44:82–88
Keil S, Plumhans C, Behrendt FF, et al. (2009) Automated measurement of lymph nodes: a phantom study. Eur Radiol 19:1079–1086
Keil S, Plumhans C, Nagy IA, et al. (2010) Dose reduction for semi-automated volumetry of hepatic metastasis in MDCT studies. Investig Radiol 45:77–81
Zhou JY, Wong DW, Ding F, et al. (2010) Liver tumour segmentation using contrast-enhanced multi-detector CT data: performance benchmarking of three semiautomated methods. Eur Radiol 20:1738–1748
Dubus L, Gayet M, Zappa M, et al. (2011) Comparison of semi-automated and manual methods to measure the volume of liver tumours on MDCT images. Eur Radiol 21:996–1003
Keil S, Bruners P, Schiffl K, et al. (2010) Radiofrequency ablation of liver metastases-software-assisted evaluation of the ablation zone in MDCT: tumor-free follow-up versus local recurrent disease. Cardiovasc Interv Radiol 33:297–306
Kudo K, Christensen S, Sasaki M, et al. (2013) Accuracy and reliability assessment of CT and MR perfusion analysis software using a digital phantom. Radiology 267:201–211
Heye T, Davenport MS, Horvath JJ, et al. (2013) Reproducibility of dynamic contrast-enhanced MR imaging. Part I. Perfusion characteristics in the female pelvis by using multiple computer-aided diagnosis perfusion analysis solutions. Radiology 266:801–811
RDCT (2009) R: A language and environment for statistical computing. In: R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org
Mazzaferro V, Regalia E, Doci R, et al. (1996) Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 334:693–699
Funding
AUR-GE Radiology Research Academic Fellowship (GERRAF).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubner, M.G., Dustin Pooler, B., del Rio, A.M. et al. Volumetric evaluation of hepatic tumors: multi-vendor, multi-reader liver phantom study. Abdom Imaging 39, 488–496 (2014). https://doi.org/10.1007/s00261-014-0079-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0079-z