Abstract
Purpose
Transthyretin cardiac amyloidosis (ATTR-CA) is thought to be prevalent in patients with severe aortic stenosis (AS) who are referred for transcatheter aortic valve replacement (TAVR). However, prior studies were published when TAVR was only offered to elderly, inoperable, and high-risk patients. The aim of this study was to reevaluate the prevalence of ATTR-CA in a contemporary TAVR population and identify high-risk features to guide referral for technetium-99 pyrophosphate scan (99mTc-PyP scan) screening.
Methods
Patients seen in a multidisciplinary TAVR clinic for severe AS 70 years and older were referred for a 99mTc-PyP scan to evaluate for ATTR-CA. The primary outcome was the percent with a positive scan. The discriminatory ability of high-risk features was assessed to develop a more judicious screening system.
Results
Over the study period, 380 patients underwent screening, and 20 patients (5.3%) had a positive scan, with 17 patients having confirmed ATTR-CA, 1 patient deferring confirmatory testing (combined 4.7%), 1 having light chain amyloidosis, and 1 negative on biopsy. Compared to other patient and echocardiographic measures, elevated NT-pro BNP (> 1000 ng/L) was the best discriminator on who should be referred for 99mTc-PyP scan screening, with a sensitivity of 90% and a negative predictive value of 99%.
Conclusion
The prevalence of ATTR-CA may be lower in a contemporary TAVR population due to its expanded indication for low-risk patients. NT-pro BNP is a simple test that can improve screening yield and more judiciously guide screening for ATTR-CA in this at-risk population.
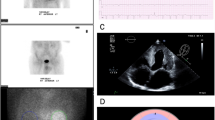
Graphical abstract
Comparison of the original versus the proposed algorithm


Similar content being viewed by others
Data Availability
Data was made available to all investigators and IRB since the data is retrospective and belongs to Cleveland Clinic.
Abbreviations
- ATTR-CA:
-
Transthyretin cardiac amyloidosis
- AS:
-
Aortic stenosis
- TAVR:
-
Transcatheter aortic valve replacement
- SAVR:
-
Surgical aortic valve replacement
- 99mTc-PyP scan:
-
Technetium-99 pyrophosphate scan
- SPECT/CT:
-
Single positron emission tomography/computed tomography
- EF:
-
Ejection fraction
- IVS:
-
Septal wall thickness
- PWT:
-
Posterior wall thickness
- LV:
-
Left ventricular
- AVA:
-
Aortic valve area
- AVAi:
-
Aortic valve area indexed to body surface area
- SVI:
-
Stroke volume index
- RAS:
-
Relative apical sparing
- SAB:
-
Septal apical to basal strain ratio
- CMR:
-
Cardiac magnetic resonance imaging
- LFLG-AS:
-
Severe low-flow, low-gradient aortic stenosis
References
Ruberg FL, Grogan M, Hanna M, Kelly JW, Maurer MS. Transthyretin amyloid cardiomyopathy: JACC state-of-the-art review, (in eng). J Am Coll Cardiol. 2019;73(22):2872–91. https://doi.org/10.1016/j.jacc.2019.04.003.
Martyn T, et al. Racial and genetic differences in presentation of transthyretin amyloid cardiomyopathy with impaired left ventricular function. JACC Heart Fail. 2022;10(9):689–691. https://doi.org/10.1016/j.jchf.2022.06.006.
Maurer MS, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379(11):1007–16. https://doi.org/10.1056/NEJMoa1805689.
Castaño A, et al. Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement, (in eng). Eur Heart J. 2017;38(38):2879–87. https://doi.org/10.1093/eurheartj/ehx350.
Cavalcante JL, et al. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis, (in eng). J Cardiovasc Magn Reson. 2017;19(1):98. https://doi.org/10.1186/s12968-017-0415-x.
Treibel TA, Fontana M, Gilbertson JA, Castelletti S, White SK, Scully PR, Roberts N, Hutt DF, Rowczenio DM, Whelan CJ, Ashworth MA, Gillmore JD, Hawkins PN, Moon JC. Occult Transthyretin cardiac amyloid in severe calcific aortic stenosis: prevalence and prognosis in patients undergoing surgical aortic valve replacement. Circ Cardiovasc Imaging. 2016;9(8):e005066. https://doi.org/10.1161/CIRCIMAGING.116.005066.
Scully PR, et al. Prevalence of cardiac amyloidosis in patients referred for transcatheter aortic valve replacement, (in eng). J Am Coll Cardiol. 2018;71(4):463–4. https://doi.org/10.1016/j.jacc.2017.11.037.
Grodin JL, Maurer MS. The truth is unfolding about transthyretin cardiac amyloidosis. Circulation. 2019;140(1):27–30. https://doi.org/10.1161/CIRCULATIONAHA.119.041015.
Gillmore JD, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis, (in eng). Circulation. 2016;133(24):2404–12. https://doi.org/10.1161/circulationaha.116.021612.
Nitsche C, et al. Light-chain and transthyretin cardiac amyloidosis in severe aortic stenosis: prevalence, screening possibilities, and outcome, (in eng). Eur J Heart Fail. 2020;22(10):1852–62. https://doi.org/10.1002/ejhf.1756.
Nitsche C, et al. Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J Am Coll Cardiol. 2021;77(2):128–39. https://doi.org/10.1016/j.jacc.2020.11.006.
van der Bijl P, Stassen J, Bax JJ. Echocardiography to identify cardiac amyloidosis in patients with calcific aortic stenosis. Eur Heart J Cardiovasc Imaging. 2022;23(10):1302–3. https://doi.org/10.1093/ehjci/jeac086.
Mack MJ, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients, (in eng). N Engl J Med. 2019;380(18):1695–705. https://doi.org/10.1056/NEJMoa1814052.
Popma JJ, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients, (in eng). N Engl J Med. 2019;380(18):1706–15. https://doi.org/10.1056/NEJMoa1816885.
Braghiroli J, Kapoor K, Thielhelm TP, Ferreira T, Cohen MG. Transcatheter aortic valve replacement in low risk patients: a review of PARTNER 3 and Evolut Low Risk trials, (in eng). Cardiovasc Diagn Ther. 2020;10(1):59–71. https://doi.org/10.21037/cdt.2019.09.12.
Dorbala S, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: part 1 of 2-evidence base and standardized methods of imaging, (in eng). J Nucl Cardiol. 2019;26(6):2065–123. https://doi.org/10.1007/s12350-019-01760-6.
Dorbala S, et al. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: part 1 of 2—evidence base and standardized methods of imaging. Circ Cardiovasc Imaging. 2021;14(7):e000029. https://doi.org/10.1161/HCI.0000000000000029.
Phelan D, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis, (in eng). Heart. 2012;98(19):1442–8. https://doi.org/10.1136/heartjnl-2012-302353.
Liu D, et al. Effect of combined systolic and diastolic functional parameter assessment for differentiation of cardiac amyloidosis from other causes of concentric left ventricular hypertrophy, Circ Cardiovasc Imaging. 2013;6(6):1066–1072. https://doi.org/10.1161/CIRCIMAGING.113.000683.
Otto CM, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines, (in eng). J Am Coll Cardiol. 2021;77(4):450–500. https://doi.org/10.1016/j.jacc.2020.11.035.
Lang RM, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging, (in eng). J Am Soc Echocardiogr. 2015;28(1):1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003.
Smith CR, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98. https://doi.org/10.1056/NEJMoa1103510.
Leon MB, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–20. https://doi.org/10.1056/NEJMoa1514616.
Jaiswal V, et al. Echocardiographic predictors of presence of cardiac amyloidosis in aortic stenosis. Eur Heart J Cardiovasc Imaging. 2022;23(10):1290–301. https://doi.org/10.1093/ehjci/jeac146.
Hanna M, et al. Cardiac scintigraphy with technetium-99m-labeled bone-seeking tracers for suspected amyloidosis: JACC review topic of the week, (in eng). J Am Coll Cardiol. 2020;75(22):2851–62. https://doi.org/10.1016/j.jacc.2020.04.022.
Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99m)Tc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses, (in eng. Circ Cardiovasc Imaging. 2013;6(2):195–201. https://doi.org/10.1161/circimaging.112.000132.
Garcia-Pavia P, et al. Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC Working Group on Myocardial and Pericardial Diseases, (in eng). Eur Heart J. 2021;42(16):1554–68. https://doi.org/10.1093/eurheartj/ehab072.
Shah KB, et al. Transthyretin cardiac amyloidosis in Black Americans, (in eng). Circ Heart Fail. 2016;9(6):e002558. https://doi.org/10.1161/circheartfailure.115.002558.
Vergaro G, Castiglione V, Aimo A, Prontera C, Masotti S, Musetti V, Nicol M, Cohen Solal A, Logeart D, Georgiopoulos G, Chubuchny V, Giannoni A, Clerico A, Buda G, Patel KN, Razvi Y, Patel R, Wechalekar A, Lachmann H, Hawkins PN, Passino C, Gillmore J, Emdin M, Fontana M. N-terminal pro-B-type natriuretic peptide and high-sensitivity troponin T hold diagnostic value in cardiac amyloidosis. Eur J Heart Fail. 2023;25(3):335–346. https://doi.org/10.1002/ejhf.2769.
Hadziselimovic E, et al. Association of high-sensitivity troponin T with outcomes in asymptomatic non-severe aortic stenosis: a post-hoc substudy of the SEAS trial, (in eng). EClinicalMedicine 2023;58:101875. https://doi.org/10.1016/j.eclinm.2023.101875.
Akodad M, et al. Prognostic impact of pre‐transcatheter and post‐transcatheter aortic valve intervention troponin: a large cohort study. J Am Heart Assoc. 2019;8(6):e011111. https://doi.org/10.1161/JAHA.118.011111.
Funding
The Cleveland Clinic Amyloidosis Registry is supported by Dr. Hanna’s Term Chair for Amyloid Heart Disease.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Bryan Abadie MD and Adel Hajj Ali MD. Analysis was performed by Bryan Abadie MD. The first draft of the manuscript was written by Bryan Abadie MD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Consent was waived in the setting of minimal risk, as approved by the Cleveland Clinic Institutional Review Board.
Conflict of interest
Dr. Martyn receives research support from Ionis Therapeutics related to amyloidosis research, is an advisor to Recora health, and receives research support from Novartis. Dr. Hanna serves on the advisory boards of Alnylam Pharmaceuticals Inc., Eidos, Ionis Therapeutics, and Pfizer Inc. Drs. Jaber and Cremer have institutional coreLab contracts with Edwards Life Sciences, BMS, and Boston Scientific. The remaining authors have no relevant disclosures.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abadie, B., Ali, A.H., Martyn, T. et al. Prevalence of ATTR-CA and high-risk features to guide testing in patients referred for TAVR. Eur J Nucl Med Mol Imaging 50, 3910–3916 (2023). https://doi.org/10.1007/s00259-023-06374-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06374-2