Abstract
Purpose
We aimed to assess the effect of concomitant medication, age, sex, body mass index and 18-kDa translocator protein (TSPO) binding affinity status on the metabolism and plasma pharmacokinetics of [18F]DPA-714 and their influence on the plasma input function in a large cohort of 201 subjects who underwent brain and whole-body PET imaging to investigate the role of neuroinflammation in neurological diseases.
Methods
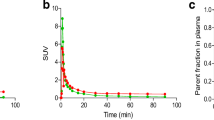
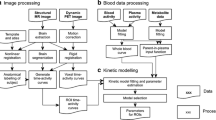
The non-metabolized fraction of [18F]DPA-714 was estimated in venous plasma of 138 patients and 63 healthy controls (HCs; including additional arterial sampling in 16 subjects) during the 90 min brain PET acquisition using a direct solid-phase extraction method. The mean fraction between 70 and 90 min post-injection ([18F]DPA-71470–90) and corresponding normalized plasma concentration (SUV70-90) were correlated with all factors using a multiple linear regression model. Differences between groups (arterial vs venous measurements; HCs vs patients; high- (HAB), mixed- (MAB) and low-affinity binders (LAB); subjects with vs without co-medications, females vs males were also assessed using the non-parametric Mann–Whitney or Kruskal–Wallis ANOVA tests. Finally, the impact of co-medications on the brain uptake of [18F]DPA-714 at equilibrium was investigated.
Results
As no significant differences were observed between arterial and venous [18F]DPA-71470–90 and SUV70-90, venous plasma was used for correlations. [18F]DPA-71470–90 was not significantly different between patients and HCS (59.7 ± 12.3% vs 60.2 ± 12.9%) despite high interindividual variability. However, 47 subjects exhibiting a huge increase or decrease of [18F]DPA-71470–90 (up to 88% or down to 23%) and SUV70-90 values (2–threefold) were found to receive co-medications identified as inhibitors or inducers of CYP3A4, known to catalyse [18F]DPA-714 metabolism. Comparison between cortex-to-plasma ratios using individual input function (VTIND) or population-based input function derived from untreated HCs (VTPBIF) indicated that non-considering the individual metabolism rate led to a bias of about 30% in VT values. Multiple linear regression model analysis of subjects free of these co-medications suggested significant correlations between [18F]DPA-71470–90 and age, BMI and sex while TSPO polymorphism did not influence the metabolism of the radiotracer. [18F]DPA-714 metabolism fell with age and BMI and was significantly faster in females than in males. Whole-body PET/CT exhibited a high uptake of the tracer in TSPO-rich organs (heart wall, spleen, kidneys…) and those involved in metabolism and excretion pathways (liver, gallbladder) in HAB and MAB with a strong decrease in LAB (-89% and -85%) resulting in tracer accumulation in plasma (4.5 and 3.3-fold increase).
Conclusion
Any co-medication that inhibits or induces CYP3A4 as well as TSPO genetic status, age, BMI and sex mostly contribute to interindividual variations of the radiotracer metabolism and/or concentration that may affect the input function of [18F]DPA-714 and consequently its human brain and peripheral uptake.
Trial registration: INFLAPARK, NCT02319382, registered December 18, 2014, retrospectively registered; IMABIO 3, NCT01775696, registered January 25, 2013, retrospectively registered; INFLASEP, NCT02305264, registered December 2, 2014, retrospectively registered; EPI-TEP, EudraCT 2017–003381-27, registered September 24, 2018.







Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SUV: :
-
Standardized uptake value
- HAB: :
-
High-affinity binders
- MAB::
-
Mixed-affinity binders
- LAB::
-
Low-affinity binders
- BMI: :
-
Body Mass Index
- TSPO: :
-
18-KDa translocator protein
- TACs:
-
Time-activity curves
- AUC:
-
Area under the curve
- VT::
-
Total volume of distribution
- PBIF::
-
Population-based input function
- IDIF::
-
Image-derived input function
- VOI::
-
Volume of interest
References
Cosenza-Nashat M, Zhao ML, Suh HS, et al. Expression of the translocator protein of 18 kDa by microglia, macrophages and astrocytes based on immunohistochemical localization in abnormal human brain. Neuropathol Appl Neurobiol. 2009. https://doi.org/10.1111/j.1365-2990.2008.01006.x.
Zhang L, Hu K, Shao T, et al. Recent developments on PET radiotracers for TSPO and their applications in neuroimaging. Acta Pharm Sin B. 2021. https://doi.org/10.1016/j.apsb.2020.08.006.
Hamelin L, Lagarde J, Dorothée G, et al. Distinct dynamic profiles of microglial activation are associated with progression of Alzheimer’s disease. Brain. 2018. https://doi.org/10.1093/brain/awy079.
Bodini B, Poirion E, Tonietto M, et al. Individual Mapping of Innate Immune Cell Activation Is a Candidate Marker of Patient-Specific Trajectories of Worsening Disability in Multiple Sclerosis. J Nucl Med. 2020. https://doi.org/10.2967/jnumed.119.231340.
Lavisse S, Goutal S, Wimberley C, et al. Increased microglial activation in patients with Parkinson disease using [18F]-DPA714 TSPO PET imaging. Parkinsonism Relat Disord. 2021. https://doi.org/10.1016/j.parkreldis.2020.11.011.
Hashimoto K, Inoue O, Suzuki K, et al. Synthesis and evaluation of 11C-PK11195 for in vivo study of peripheral-type benzodiazepine receptors using positron emission tomography. Ann Nucl Med. 1989. https://doi.org/10.1007/bf03164587.
Chauveau F, Van Camp N, Dollé F, et al. Comparative evaluation of the translocator protein radioligands 11C-DPA-713, 18F-DPA-714, and 11C-PK11195 in a rat model of acute neuroinflammation. J Nucl Med. 2009. https://doi.org/10.2967/jnumed.108.058669.
James ML, Fulton RR, Vercoullie J, et al. DPA-714, a new translocator protein-specific ligand: synthesis, radiofluorination, and pharmacologic characterization. J Nucl Med. 2008. https://doi.org/10.2967/jnumed.107.046151.
Lavisse S, Inoue K, Jan C, et al. [18F]DPA-714 PET imaging of translocator protein TSPO (18 kDa) in the normal and excitotoxically-lesioned nonhuman primate brain. Eur J Nucl Med Mol Imaging. 2015. https://doi.org/10.1007/s00259-014-2962-9.
Arlicot N, Vercouillie J, Ribeiro MJ, et al. Initial evaluation in healthy humans of [18F]DPA-714, a potential PET biomarker for neuroinflammation. Nucl Med Biol. 2012. https://doi.org/10.1016/j.nucmedbio.2011.10.012.
Lavisse S, García-Lorenzo D, Peyronneau MA et al. Optimized Quantification of Translocator Protein Radioligand 18F-DPA-714 Uptake in the Brain of Genotyped Healthy controls. J. Nucl. Med. 2015; https://doi.org/10.2967/jnumed.115.156083.
Hamelin L, Lagarde J, Dorothée G et al. Clinical IMABio3 team. Early and protective microglial activation in Alzheimer's disease: a prospective study using 18F-DPA-714 PET imaging. Brain. 2016; https://doi.org/10.1093/brain/aww017.
Yrondi A, Aouizerate B, El-Hage W, et al. Assessment of Translocator Protein Density, as Marker of Neuroinflammation, in Major Depressive Disorder: A Pilot, Multicenter, Comparative, Controlled, Brain PET Study (INFLADEP Study). Front Psychiatry. 2018. https://doi.org/10.3389/fpsyt.2018.00326.
Backhaus P, Roll W, Beuker C, et al. Initial experience with [18F]DPA-714 TSPO-PET to image inflammation in primary angiitis of the central nervous system. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-019-04662-4.
Owen DR, Yeo AJ, Gunn RN, et al. An 18-kDa translocator protein (TSPO) polymorphism explains differences in binding affinity of the PET radioligand PBR28. J Cereb Blood Flow Metab. 2012. https://doi.org/10.1038/jcbfm.2011.147.
Peyronneau MA, Saba W, Goutal S, et al. Metabolism and quantification of [(18)F]DPA-714, a new TSPO positron emission tomography radioligand. Drug Metab Dispos. 2013. https://doi.org/10.1124/dmd.112.046342.
Guengerich FP. Cytochrome P450 research and The Journal of Biological Chemistry. J Biol Chem. 2019. https://doi.org/10.1074/jbc.tm118.004144.
Vicente-Rodríguez M, Singh N, Turkheimer F, et al. Resolving the cellular specificity of TSPO imaging in a rat model of peripherally-induced neuroinflammation. Brain Behav Immun. 2021;96:154–67. https://doi.org/10.1016/j.bbi.2021.05.025.
Guilarte TR, Alexander N, Rodichkin AN, et al. Imaging neuroinflammation with TSPO: A new perspective on the cellular sources and subcellular localization. Pharmacology & Therapeutics. 2022;234:108048. https://doi.org/10.1016/j.pharmthera.2021.108048.
Fang YHD, McConathy JE, Yacoubian TA, et al. Image Quantification for TSPO PET with a Novel Image-Derived Input Function Method. Diagnostics. 2022;12:1161. https://doi.org/10.3390/diagnostics12051161.
Wimberley C, Lavisse S, Hillmer A, et al. Kinetic modeling and parameter estimation of TSPO PET imaging in the human brain. Eur J Nucl Med Mol Imaging. 2021;49:246–56. https://doi.org/10.1007/s00259-021-05248-9.
Kuhnast B, Damont A, Hinnen F, et al. [18F]DPA-714, [18F]PBR111 and [18F]FEDAA1106-selective radioligands for imaging TSPO 18 kDa with PET: automated radiosynthesis on a TRACERLAb FX-FN synthesizer and quality controls. Appl Radiat Isot. 2012. https://doi.org/10.1016/j.apradiso.2011.10.015.
Ma B, Prueksaritanont T, Lin JH. Drug interactions with calcium channel blockers: possible involvement of metabolite-intermediate complexation with CYP3A. Drug Metab Dispos. 2000;28(2):125–30.
Guay DR. Extended-release alfuzosin hydrochloride: a new alpha-adrenergic receptor antagonist for symptomatic benign prostatic hyperplasia. Am J Geriatr Pharmacother. 2004. https://doi.org/10.1016/s1543-5946(04)90003-7.
Denisov IG, Baylon JL, Grinkova YV, et al. Drug-Drug Interactions between Atorvastatin and Dronedarone Mediated by Monomeric CYP3A4. Biochemistry. 2018. https://doi.org/10.1021/acs.biochem.7b01012.
Sönnerstam E, Sjölander M, Lövheim H, et al. Clinically relevant drug-drug interactions among elderly people with dementia. Eur J Clin Pharmacol. 2018. https://doi.org/10.1007/s00228-018-2514-5.
Choi YH, Lee MG. Pharmacokinetic and pharmacodynamic interaction between nifedipine and metformin in rats: competitive inhibition for metabolism of nifedipine and metformin by each other via CYP isozymes. Xenobiotica. 2012. https://doi.org/10.3109/00498254.2011.633177.
Nakamura K, Ariyoshi N, Iwatsubo T, et al. Inhibitory effects of nicardipine to cytochrome P450 (CYP) in human liver microsomes. Biol Pharm Bull. 2005. https://doi.org/10.1248/bpb.28.882.
Jann MW, Shirley KL, Small GW. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin Pharmacokinet. 2002. https://doi.org/10.2165/00003088-200241100-00003.
Taavitsainen P, Kiukaanniemi K, Pelkonen O. In vitro inhibition screening of human hepatic P450 enzymes by five angiotensin-II receptor antagonists. Eur J Clin Pharmacol. 2000. https://doi.org/10.1007/s002280050731.
Subrahmanyam V, Renwick AB, Walters DG, et al. Identification of cytochrome P450 isoforms responsible for cis-tramadol metabolism in human liver microsomes. Drug Metab Dispos. 2001;29(8):1146–55.
Caccia S. Metabolism of the newer antidepressants An overview of the pharmacological and pharmacokinetic implications. Clin Pharmacokinet. 1998;34(4):281–302. https://doi.org/10.2165/00003088-199834040-00002.
Martin P, Gillen M, Millson D, et al. Effects of CYP3A4 Inhibitors Ketoconazole and Verapamil and the CYP3A4 Inducer Rifampicin on the Pharmacokinetic Parameters of Fostamatinib: Results from In Vitro and Phase I Clinical Studies. Drugs R D. 2016. https://doi.org/10.1007/s40268-015-0118-4.
Armijo JA, Vega-Gil N, Shushtarian M, et al. 10-Hydroxycarbazepine serum concentration-to-oxcarbazepine dose ratio: influence of age and concomitant antiepileptic drugs. Ther Drug Monit. 2005. https://doi.org/10.1097/01.ftd.0000155342.93489.fd.
Kam WW, Meikle SR, Zhou H, et al. The 18 kDa translocator protein (peripheral benzodiazepine receptor) expression in the bone of normal, osteoprotegerin or low calcium diet treated mice. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0030623.
Rizzo G, Veronese M, Tonietto M, et al. Generalization of endothelial modelling of TSPO PET imaging: Considerations on tracer affinities. J Cereb Blood Flow Metab. 2019. https://doi.org/10.1177/0271678X17742004.
Wolbold R, Klein K, Burk O, et al. Sex is a major determinant of CYP3A4 expression in human liver. Hepatology. 2003. https://doi.org/10.1053/jhep.2003.50393.
Cotreau, M.M, von Moltke, L.L & Greenblatt, D.J. The Influence of Age and Sex on the Clearance of Cytochrome P450 3A Substrates. Clin Pharmacokinet. 2005; https://doi.org/10.2165/00003088-200544010-00002.
Wang P, Shao X, Bao Y, et al. Impact of obese levels on the hepatic expression of nuclear receptors and drug-metabolizing enzymes in adult and offspring mice. Acta Pharm Sin B. 2020. https://doi.org/10.1016/j.apsb.2019.10.009.
Tuisku J, Plavén-Sigray P, Gaiser EC, et al. Effects of age, BMI and sex on the glial cell marker TSPO - a multicentre [11C]PBR28 HRRT PET study. Eur J Nucl Med Mol Imaging. 2019. https://doi.org/10.1007/s00259-019-04403-7.
Hirvonen J, Roivainen A, Virta J, et al. Human biodistribution and radiation dosimetry of 11C-(R)-PK11195, the prototypic PET ligand to image inflammation. Eur J Nucl Med Mol Imaging. 2010. https://doi.org/10.1007/s00259-009-1298-3.
Foss CA, Plyku D, Ordonez AA, et al. Biodistribution and Radiation Dosimetry of 124I-DPA-713, a PET Radiotracer for Macrophage-Associated Inflammation. J Nucl Med. 2018. https://doi.org/10.2967/jnumed.117.207431.
Sakata M, Ishibashi K, Imai M, et al. Assessment of safety, efficacy, and dosimetry of a novel 18-kDa translocator protein ligand, [11C]CB184, in healthy human volunteers. Eur J Nucl Med Mol Imaging Res. 2017. https://doi.org/10.1186/s13550-017-0271-6.
Brown AK, Fujita M, Fujimura Y, et al. Radiation dosimetry and biodistribution in monkey and man of 11C-PBR28: a PET radioligand to image inflammation. J Nucl Med. 2007. https://doi.org/10.2967/jnumed.107.044842.
Fujimura Y, Kimura Y, Siméon FG, et al. Biodistribution and radiation dosimetry in humans of a new PET ligand, (18)F-PBR06, to image translocator protein (18 kDa). J Nucl Med. 2010. https://doi.org/10.2967/jnumed.109.068064.
Brody AL, Okita K, Shieh J, et al. Radiation dosimetry and biodistribution of the translocator protein radiotracer [(11)C]DAA1106 determined with PET/CT in healthy human volunteers. Nucl Med Biol. 2014. https://doi.org/10.1016/j.nucmedbio.2014.07.004.
Kreisl WC, Fujita M, Fujimura Y, et al. Comparison of [(11)C]-(R)-PK 11195 and [(11)C]PBR28, two radioligands for translocator protein (18 kDa) in human and monkey: Implications for positron emission tomographic imaging of this inflammation biomarker. Neuroimage. 2010. https://doi.org/10.1016/j.neuroimage.2009.11.056.
Acknowledgements
We would like to thank all study participants and the staff at the SHFJ PET for their assistance : Claude Comtat, Vincent Brulon, Christine Baron, Christine Coulon, Stéphane Demphel, Maud Goislard, Françoise Hinnen, Thierry Lekieffre, Christine Manciot.
Funding
PET imaging studies: Imabio3: French Health Ministry (PHRC- 0054-N 2010) and Institut Roche de Recherche et Medecine Translationelle, European Union’s Seventh Framework Programme (FP7/2007–2013), grant agreement HEALTH-F2-2011–278850 (INMiND); Inflapark: France Parkinson (GAO 2008) and Neuratris; Inflasep: ANR grant MNP2008-007125; Epitep: French Federation for Epilepsy Research.
Author information
Authors and Affiliations
Contributions
This manuscript has been seen and approved by all authors, and each author has contributed significantly to this work. Subject recruitment and/or supervision and design the PET study: MB, MS, BS, SL, PR, VB, CL. Supervision and design of the metabolism and pharmacokinetic study: MAP. Statistical analysis: MAP, MB, CL; [18F]DPA-714 PK data: BJ, MAP; Radiochemistry/radiopharmacy: BK, FC, PG; WB PET images analysis: DLN, SG; MB; Brain PET images analysis: CL, MB; Manuscript draft: MAP, MB.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peyronneau, M., Kuhnast, B., Nguyen, DL. et al. [18F]DPA-714: Effect of co-medications, age, sex, BMI and TSPO polymorphism on the human plasma input function. Eur J Nucl Med Mol Imaging 50, 3251–3264 (2023). https://doi.org/10.1007/s00259-023-06286-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06286-1