Abstract
Purpose
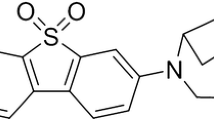
We report findings from the first-in-human study of [11C]MDTC, a radiotracer developed to image the cannabinoid receptor type 2 (CB2R) with positron emission tomography (PET).
Methods
Ten healthy adults were imaged according to a 90-min dynamic PET protocol after bolus intravenous injection of [11C]MDTC. Five participants also completed a second [11C]MDTC PET scan to assess test-retest reproducibility of receptor-binding outcomes. The kinetic behavior of [11C]MDTC in human brain was evaluated using tissue compartmental modeling. Four additional healthy adults completed whole-body [11C]MDTC PET/CT to calculate organ doses and the whole-body effective dose.
Results
[11C]MDTC brain PET and [11C]MDTC whole-body PET/CT was well-tolerated. A murine study found evidence of brain-penetrant radiometabolites. The model of choice for fitting the time activity curves (TACs) across brain regions of interest was a three-tissue compartment model that includes a separate input function and compartment for the brain-penetrant metabolites. Regional distribution volume (VT) values were low, indicating low CB2R expression in the brain. Test-retest reliability of VT demonstrated a mean absolute variability of 9.91%. The measured effective dose of [11C]MDTC was 5.29 μSv/MBq.
Conclusion
These data demonstrate the safety and pharmacokinetic behavior of [11C]MDTC with PET in healthy human brain. Future studies identifying radiometabolites of [11C]MDTC are recommended before applying [11C]MDTC PET to assess the high expression of the CB2R by activated microglia in human brain.




Similar content being viewed by others
Data availability
The datasets generated and analyzed in this study are available from the corresponding author on reasonable request.
References
Xin Q, et al. The impact of cannabinoid type 2 receptors (CB2Rs) in neuroprotection against neurological disorders. Acta Pharmacol Sin. 2020;41(12):1507–18.
Basavarajappa BS, et al. Endocannabinoid system in neurodegenerative disorders. J Neurochem. 2017;142(5):624–48.
Solas M, et al. CB2 receptor and amyloid pathology in frontal cortex of Alzheimer's disease patients. Neurobiol Aging. 2013;34(3):805–8.
Gómez-Gálvez Y, et al. Potential of the cannabinoid CB(2) receptor as a pharmacological target against inflammation in Parkinson's disease. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:200–8.
García MC, et al. Identification of CB2 receptors in human nigral neurons that degenerate in Parkinson's disease. Neurosci Lett. 2015;587:1–4.
Cristino L, Bisogno T, Di Marzo V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat Rev Neurol. 2020;16(1):9–29.
Horti AG, et al. Synthesis and biodistribution of [11C]A-836339, a new potential radioligand for PET imaging of cannabinoid type 2 receptors (CB2). Bioorg Med Chem. 2010;18(14):5202–7.
Yao BB, et al. Characterization of a cannabinoid CB2 receptor-selective agonist, A-836339 [2,2,3,3-tetramethyl-cyclopropanecarboxylic acid [3-(2-methoxy-ethyl)-4,5-dimethyl-3H-thiazol-(2Z)-ylidene]-amide], using in vitro pharmacological assays, in vivo pain models, and pharmacological magnetic resonance imaging. J Pharmacol Exp Ther. 2009;328(1):141–51.
Rahmim A, et al. Statistical dynamic image reconstruction in state-of-the-art high-resolution PET. Phys Med Biol. 2005;50(20):4887–912.
Hilton J, et al. Column-switching HPLC for the analysis of plasma in PET imaging studies. Nucl Med Biol. 2000;27(6):627–30.
Coughlin JM, et al. The distribution of the alpha7 nicotinic acetylcholine receptor in healthy aging: an in vivo positron emission tomography study with [(18)F]ASEM. Neuroimage. 2018;165:118–24.
Innis RB, et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab. 2007;27(9):1533–9.
Carson RE. Parameter estimation in positron emission tomography. In: Principles And Applications For The Brain And Heart. New York, N Y, USA: Raven Press; 1986. p. Xiii+690. Illus 347-390.
Fujita M, et al. Kinetic and equilibrium analyses of [(123)I]epidepride binding to striatal and extrastriatal dopamine D(2) receptors. Synapse. 1999;34(4):290–304.
Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46(6):1023–7.
Glatting G, et al. Choosing the optimal fit function: comparison of the Akaike information criterion and the F-test. Med Phys. 2007;34(11):4285–92.
Scheinin NM, et al. Biodistribution and radiation dosimetry of the amyloid imaging agent 11C-PIB in humans. J Nucl Med. 2007;48(1):128–33.
van der Aart J, et al. Radiation dose estimates for carbon-11-labelled PET tracers. Nucl Med Biol. 2012;39(2):305–14.
Dishino DD, et al. Relationship between lipophilicity and brain extraction of C-11-labeled radiopharmaceuticals. J Nucl Med. 1983;24(11):1030–8.
Kao CH, et al. Evaluation of [76Br]FBAU 3',5'-dibenzoate as a lipophilic prodrug for brain imaging. Nucl Med Biol. 2002;29(5):527–35.
Kubinyi H. The quantitative analysis of structure-activity relationships. In: Abraham DJ, editor. Burger’s Medicinal Chemistry and Drug Discovery, in Burger’s Medicinal Chemistry and Drug Discovery. New York: Wiley; 1995. p. 497–571.
Welch MJ, et al. Biodistribution of N-alkyl and N-fluoroalkyl derivatives of spiroperidol; radiopharmaceuticals for PET studies of dopamine receptors. Int J Rad Appl Instrum B. 1986;13(5):523–6.
Evens N, et al. Synthesis and biological evaluation of carbon-11- and fluorine-18-labeled 2-oxoquinoline derivatives for type 2 cannabinoid receptor positron emission tomography imaging. Nucl Med Biol. 2009;36(4):455–65.
Katoch-Rouse R, et al. Synthesis, structure-activity relationship, and evaluation of SR141716 analogues: development of central cannabinoid receptor ligands with lower lipophilicity. J Med Chem. 2003;46(4):642–5.
Liu QR, et al. Species differences in cannabinoid receptor 2 (CNR2 gene): identification of novel human and rodent CB2 isoforms, differential tissue expression and regulation by cannabinoid receptor ligands. Genes Brain Behav. 2009;8(5):519–30.
Ahmad R, et al. Decreased in vivo availability of the cannabinoid type 2 receptor in Alzheimer's disease. Eur J Nucl Med Mol Imaging. 2016;43(12):2219–27.
Acknowledgements
This publication was supported by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number UL1 TR 001079 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS, or NIH. We also acknowledge EB024495 for support.
Funding
This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number UL1 TR 001079 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS, or NIH. We also acknowledge EB024495 for support.
Author information
Authors and Affiliations
Contributions
YD, JC, ML, AH, and MP contributed to the study conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by YD and JC, and each author read, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Johns Hopkins Institutional Review Board and was conducted under a FDA-approved US investigational new drug application (IND 131367). All experimental animal protocols were performed in accordance with relevant federal and state laws and institutional guidelines and approved by the Animal Care and Use Committee of the Johns Hopkins Medical Institutions.
Consent to participate
Written, informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurology
Supplementary information
ESM 1
(DOCX 271 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, Y., Coughlin, J.M., Brosnan, M.K. et al. First-in-human imaging using [11C]MDTC: a radiotracer targeting the cannabinoid receptor type 2. Eur J Nucl Med Mol Imaging 50, 2386–2393 (2023). https://doi.org/10.1007/s00259-023-06170-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06170-y