Abstract
Purpose
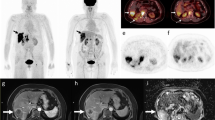
This study is to investigate the [68Ga]Ga-DOTA-FAPI PET/CT diagnosis performance in biliary tract carcinoma (BTC) and analyze the association between [68Ga]Ga-DOTA-FAPI PET/CT and clinical indexes.
Methods
A prospective study (NCT 05264688) was performed between January 2022 and July 2022. Fifty participants were scanned using [68Ga]Ga-DOTA-FAPI and [18F]FDG PET/CT and acquired pathological tissue. We employed the Wilcoxon signed-rank test to compare the uptake of [68Ga]Ga-DOTA-FAPI and [18F]FDG, and the McNemar test was used to compare the diagnostic efficacy between the two tracers. Spearman or Pearson correlation was used to assess the association between [68 Ga]Ga-DOTA-FAPI PET/CT and clinical indexes.
Results
In total, 47 participants (mean age 59.09 ± 10.98 [range 33–80 years]) were evaluated. The [68Ga]Ga-DOTA-FAPI detection rate was greater than [18F]FDG in primary tumors (97.62% vs. 85.71%), nodal metastases (90.05% vs. 87.06%), and distant metastases (100% vs. 83.67%). The uptake of [68Ga]Ga-DOTA-FAPI was higher than [18F]FDG in primary lesions (intrahepatic cholangiocarcinoma, 18.95 ± 7.47 vs. 11.86 ± 0.70, p = 0.001; extrahepatic cholangiocarcinoma, 14.57 ± 6.16 vs. 8.80 ± 4.74, p = 0.004), abdomen and pelvic cavity nodal metastases (6.91 ± 6.56 vs. 3.94 ± 2.83, p < 0.001), and distant metastases (pleural, peritoneum, omentum, and mesentery, 6.37 ± 4.21 vs. 4.50 ± 1.96, p = 0.01; bone, 12.15 ± 6.43 vs. 7.51 ± 4.54, p = 0.008). There was a significant correlation between [68Ga]Ga-DOTA-FAPI uptake and fibroblast-activation protein (FAP) expression (Spearman r = 0.432, p = 0.009), carcinoembryonic antigen (CEA) (Pearson r = 0.364, p = 0.012), and platelet (PLT) (Pearson r = 0.35, p = 0.016). Meanwhile, a significant relationship between [68Ga]Ga-DOTA-FAPI metabolic tumor volume and carbohydrate antigen199 (CA199) (Pearson r = 0.436, p = 0.002) was confirmed.
Conclusion
[68Ga]Ga-DOTA-FAPI had a higher uptake and sensitivity than [18F]FDG in the diagnosis of BTC primary and metastatic lesions. The correlation between [68Ga]Ga-DOTA-FAPI PET/CT indexes and FAP expression, CEA, PLT, and CA199 were confirmed.
Trial registration
clinicaltrials.gov: NCT 05,264,688.











Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
17 March 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00259-023-06188-2
References
Brindley PJ, Bachini M, Ilyas SI, Khan SA, Loukas A, Sirica AE, et al. Cholangiocarcinoma Nat Rev Dis Primers. 2021;7:65. https://doi.org/10.1038/s41572-021-00300-2.
Esnaola NF, Meyer JE, Karachristos A, Maranki JL, Camp ER, Denlinger CS. Evaluation and management of intrahepatic and extrahepatic cholangiocarcinoma. Cancer. 2016;122:1349–69. https://doi.org/10.1002/cncr.29692.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33. https://doi.org/10.3322/caac.21708.
Forner A, Vidili G, Rengo M, Bujanda L, Ponz-Sarvise M, Lamarca A. Clinical presentation, diagnosis and staging of cholangiocarcinoma. Liver Int. 2019;39(Suppl 1):98–107. https://doi.org/10.1111/liv.14086.
Schooler GR, Hull NC, Lee EY. Hepatobiliary MRI contrast agents: pattern recognition approach to pediatric focal hepatic lesions. AJR Am J Roentgenol. 2020;214:976–86. https://doi.org/10.2214/AJR.19.22239.
Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology. 2014;273:30–50. https://doi.org/10.1148/radiol.14132362.
Corvera CU, Blumgart LH, Akhurst T, DeMatteo RP, D’Angelica M, Fong Y, et al. 18F-fluorodeoxyglucose positron emission tomography influences management decisions in patients with biliary cancer. J Am Coll Surg. 2008;206:57–65. https://doi.org/10.1016/j.jamcollsurg.2007.07.002.
Kato T, Tsukamoto E, Kuge Y, Katoh C, Nambu T, Nobuta A, et al. Clinical role of (18)F-FDG PET for initial staging of patients with extrahepatic bile duct cancer. Eur J Nucl Med Mol Imaging. 2002;29:1047–54. https://doi.org/10.1007/s00259-002-0852-z.
Singnurkar A, Poon R, Metser U. Comparison of 18F-FDG-PET/CT and 18F-FDG-PET/MR imaging in oncology: a systematic review. Ann Nucl Med. 2017;31:366–78. https://doi.org/10.1007/s12149-017-1164-5.
Salas JR, Clark PM. Signaling pathways that drive (18)F-FDG accumulation in cancer. J Nucl Med. 2022;63:659–63. https://doi.org/10.2967/jnumed.121.262609.
Ziai P, Hayeri MR, Salei A, Salavati A, Houshmand S, Alavi A, et al. Role of optimal quantification of FDG PET imaging in the clinical practice of radiology. Radiographics. 2016;36:481–96. https://doi.org/10.1148/rg.2016150102.
Li X, Zhang Y, Zhang Y. (18)F-FDG PET/CT may be a suitable method for preoperative diagnosis and evaluation of Chinese older patients with hilar cholangiocarcinoma. BMC Geriatr. 2018;18:150. https://doi.org/10.1186/s12877-018-0846-8.
Sahai E, Astsaturov I, Cukierman E, DeNardo DG, Egeblad M, Evans RM, et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat Rev Cancer. 2020;20:174–86. https://doi.org/10.1038/s41568-019-0238-1.
Biffi G, Tuveson DA. Diversity and biology of cancer-associated fibroblasts. Physiol Rev. 2021;101:147–76. https://doi.org/10.1152/physrev.00048.2019.
Yang X, Lin Y, Shi Y, Li B, Liu W, Yin W, et al. FAP Promotes immunosuppression by cancer-associated fibroblasts in the tumor microenvironment via STAT3-CCL2 signaling. Cancer Res. 2016;76:4124–35. https://doi.org/10.1158/0008-5472.CAN-15-2973.
Fitzgerald AA, Weiner LM. The role of fibroblast activation protein in health and malignancy. Cancer Metastasis Rev. 2020;39:783–803. https://doi.org/10.1007/s10555-020-09909-3.
Giesel FL, Adeberg S, Syed M, Lindner T, Jimenez-Franco LD, Mavriopoulou E, et al. FAPI-74 PET/CT using either (18)F-AlF or cold-kit (68)Ga labeling: biodistribution, radiation dosimetry, and tumor delineation in lung cancer patients. J Nucl Med. 2021;62:201–7. https://doi.org/10.2967/jnumed.120.245084.
Koerber SA, Staudinger F, Kratochwil C, Adeberg S, Haefner MF, Ungerechts G, et al. The role of (68)Ga-FAPI PET/CT for patients with malignancies of the lower gastrointestinal tract: first clinical experience. J Nucl Med. 2020;61:1331–6. https://doi.org/10.2967/jnumed.119.237016.
Chen H, Pang Y, Wu J, Zhao L, Hao B, Wu J, et al. Comparison of [(68)Ga]Ga-DOTA-FAPI-04 and [(18)F] FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer. Eur J Nucl Med Mol Imaging. 2020;47:1820–32. https://doi.org/10.1007/s00259-020-04769-z.
Pang Y, Zhao L, Luo Z, Hao B, Wu H, Lin Q, et al. Comparison of (68)Ga-FAPI and (18)F-FDG uptake in gastric, duodenal, and colorectal cancers. Radiology. 2021;298:393–402. https://doi.org/10.1148/radiol.2020203275.
Hicks RJ, Roselt PJ, Kallur KG, Tothill RW, Mileshkin L. FAPI PET/CT: Will It End the Hegemony of (18)F-FDG in Oncology? J Nucl Med. 2021;62:296–302. https://doi.org/10.2967/jnumed.120.256271.
Lan L, Zhang S, Xu T, Liu H, Wang W, Feng Y, et al. Prospective comparison of (68)Ga-FAPI versus (18)F-FDG PET/CT for tumor staging in biliary tract cancers. Radiology. 2022;304:648–57. https://doi.org/10.1148/radiol.213118.
Dendl K, Koerber SA, Kratochwil C, Cardinale J, Finck R, Dabir M, et al. 2021 FAP and FAPI-PET/CT in malignant and non-malignant diseases: a perfect symbiosis? Cancers (Basel). 13 https://doi.org/10.3390/cancers13194946.
Altmann A, Haberkorn U, Siveke J. The latest developments in imaging of fibroblast activation protein. J Nucl Med. 2021;62:160–7. https://doi.org/10.2967/jnumed.120.244806.
Wang H, Zhu W, Ren S, Kong Y, Huang Q, Zhao J, et al. (68)Ga-FAPI-04 versus (18)F-FDG PET/CT in the detection of hepatocellular carcinoma. Front Oncol. 2021;11:693640. https://doi.org/10.3389/fonc.2021.693640.
Guo W, Pang Y, Yao L, Zhao L, Fan C, Ke J, et al. Imaging fibroblast activation protein in liver cancer: a single-center post hoc retrospective analysis to compare [(68)Ga]Ga-FAPI-04 PET/CT versus MRI and [(18)F]-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2021;48:1604–17. https://doi.org/10.1007/s00259-020-05095-0.
Tao DL, Tassi Yunga S, Williams CD, McCarty OJT. Aspirin and antiplatelet treatments in cancer. Blood. 2021;137:3201–11. https://doi.org/10.1182/blood.2019003977.
Haemmerle M, Stone RL, Menter DG, Afshar-Kharghan V, Sood AK. The platelet lifeline to cancer: challenges and opportunities. Cancer Cell. 2018;33:965–83. https://doi.org/10.1016/j.ccell.2018.03.002.
Sirica AE, Gores GJ, Groopman JD, Selaru FM, Strazzabosco M, Wei Wang X, et al. Intrahepatic cholangiocarcinoma: continuing challenges and translational advances. Hepatology. 2019;69:1803–15. https://doi.org/10.1002/hep.30289.
Cadamuro M, Nardo G, Indraccolo S, Dall’olmo L, Sambado L, Moserle L, et al. Platelet-derived growth factor-D and Rho GTPases regulate recruitment of cancer-associated fibroblasts in cholangiocarcinoma. Hepatology. 2013;58:1042–53. https://doi.org/10.1002/hep.26384.
Acknowledgements
The authors gratefully acknowledge all participants.
Funding
This work was supported by grants from the Key Research and Development Program of Hubei Province (2021BCA114), Research Fund of the Health Commission of Hubei Province (WJ2021M255), and Cancer Research and Translational Platform Project of Zhongnan Hospital of Wuhan University (ZLYNXM202004).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Yuan Yufeng, He Yong, and Zhang Zhonglin designed the clinical research. Jiang Yaqun and Xia Xigang conducted the literature search. Liao Bo, Zhu Qian, Wang Haitao, Wu Dongde, Jiang Ping, Tang Shengli, Yang Zhiyong, and He Yueming recruited the patients. Li Jinghua, Xu Kui, Guo Deliang, and Jiang Yaqun conducted the study and collected and analyzed data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in all figures.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The authors regret to inform that there is an error in their original article. The following article note is missing in the original article: Li Jinghua, Xu Kui, and Guo Deliang contributed equally to the work.
The original article has been corrected.
This article is part of the Topical Collection on Oncology - General.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jinghua, L., Kui, X., Deliang, G. et al. Clinical prospective study of Gallium 68 (68Ga)–labeled fibroblast-activation protein inhibitor PET/CT in the diagnosis of biliary tract carcinoma. Eur J Nucl Med Mol Imaging 50, 2152–2166 (2023). https://doi.org/10.1007/s00259-023-06137-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06137-z