Abstract
Purpose
This study aimed to explore the clinical staging performance of [68 Ga]Ga-DOTA-FAPI-04 PET/CT compared with that of 2-[18F]FDG PET/CT in non-small cell lung cancer (NSCLC) patients lesion by lesion.
Methods
A total of 134 diagnosed or suspected NSCLC patients were enrolled in the prospective study (ChiCTR2000038080); they received paired 2-[18F]FDG PET/CT and [68 Ga]Ga-DOTA-FAPI-04 PET/CT. Of these patients, the retrospective analysis of 74 NSCLC patients with pathological results was conducted from primary tumor (T) diagnosis, lymph node (N), and metastatic lesion (M) staging. The imaging characteristics of the lung nodules and suspected metastases were obtained and analyzed, and the staging performance of 2-[18F]FDG PET/CT and [68 Ga]Ga-DOTA-FAPI-04 PET/CT was compared.
Results
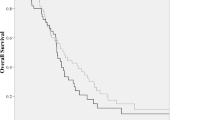
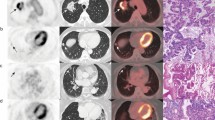
For T diagnosis, [68 Ga]Ga-DOTA-FAPI-04 showed better diagnostic performance than 2-[18F]FDG in 79 lung nodules of 72 patients, especially for nonsolid and small-dimension adenocarcinoma nodules. For N staging, 98 lymph nodes (LNs) with pathological results in 37 patients were analyzed. The SUVmax of [68 Ga]Ga-DOTA-FAPI-04 in the nonmetastatic LNs was significantly lower than that in the metastatic LNs. Regarding metastatic LN identification, the calculated optimum cut-off value of [68 Ga]Ga-DOTA-FAPI-04 SUVmax was 5.5, and the diagnostic accuracy using [68 Ga]Ga-DOTA-FAPI-04 and 2-[18F]FDG criteria was 94% and 30%, respectively (P < 0.001). For M staging, [68 Ga]Ga-DOTA-FAPI-04 identified more lesions than 2-[18F]FDG (257 vs. 139 lesions) in 14 patients with multiple metastases. Overall, the staging accuracy of [68 Ga]Ga-DOTA-FAPI-04 was better than that of 2-[18F]FDG in 52 patients with different pathological stages [43/52 (82.7%) vs. 27/52 (51.9%), P = 0.001].
Conclusion
Compared with 2-[18F]FDG PET/CT, [68 Ga]Ga-DOTA-FAPI-04 PET/CT demonstrated better staging performance in NSCLC patients with different pathological stages, especially those with localized disease.





Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or uploaded as supplementary information.
Code availability
Not applicable.
References
Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16:582–98. https://doi.org/10.1038/nrc.2016.73.
Santi A, Kugeratski FG, Zanivan S. Cancer associated fibroblasts: the architects of stroma remodeling. Proteomics. 2018;18. https://doi.org/10.1002/pmic.201700167.
Liao Z, Tan ZW, Zhu P, Tan NS. Cancer-associated fibroblasts in tumor microenvironment - accomplices in tumor malignancy. Cell Immunol. 2019;343:103729. https://doi.org/10.1016/j.cellimm.2017.12.003.
McCarthy JB, El-Ashry D, Turley EA. Hyaluronan, cancer-associated fibroblasts and the tumor microenvironment in malignant progression. Front Cell Dev Biol. 2018;6:48. https://doi.org/10.3389/fcell.2018.00048.
Han Y, Zhang Y, Jia T, Sun Y. Molecular mechanism underlying the tumor-promoting functions of carcinoma-associated fibroblasts. Tumour Biol. 2015;36:1385–94. https://doi.org/10.1007/s13277-015-3230-8.
Koczorowska MM, Tholen S, Bucher F, Lutz L, Kizhakkedathu JN, De Wever O, et al. Fibroblast activation protein-alpha, a stromal cell surface protease, shapes key features of cancer associated fibroblasts through proteome and degradome alterations. Mol Oncol. 2016;10:40–58. https://doi.org/10.1016/j.molonc.2015.08.001.
Garin-Chesa P, Old LJ, Rettig WJ. Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc Natl Acad Sci U S A. 1990;87:7235–9. https://doi.org/10.1073/pnas.87.18.7235.
Lai D, Ma L, Wang F. Fibroblast activation protein regulates tumor-associated fibroblasts and epithelial ovarian cancer cells. Int J Oncol. 2012;41:541–50. https://doi.org/10.3892/ijo.2012.1475.
Loktev A, Lindner T, Mier W, Debus J, Altmann A, Jager D, et al. A tumor-imaging method targeting cancer-associated fibroblasts. J Nucl Med. 2018;59:1423–9. https://doi.org/10.2967/jnumed.118.210435.
Lindner T, Loktev A, Altmann A, Giesel F, Kratochwil C, Debus J, et al. Development of quinoline-based theranostic ligands for the targeting of fibroblast activation protein. J Nucl Med. 2018;59:1415–22. https://doi.org/10.2967/jnumed.118.210443.
Giesel FL, Kratochwil C, Lindner T, Marschalek MM, Loktev A, Lehnert W, et al. (68)Ga-FAPI PET/CT: biodistribution and preliminary dosimetry estimate of 2 DOTA-containing FAP-targeting agents in patients with various cancers. J Nucl Med. 2019;60:386–92. https://doi.org/10.2967/jnumed.118.215913.
Kratochwil C, Flechsig P, Lindner T, Abderrahim L, Altmann A, Mier W, et al. (68)Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer. J Nucl Med. 2019;60:801–5. https://doi.org/10.2967/jnumed.119.227967.
Rohrich M, Loktev A, Wefers AK, Altmann A, Paech D, Adeberg S, et al. IDH-wildtype glioblastomas and grade III/IV IDH-mutant gliomas show elevated tracer uptake in fibroblast activation protein-specific PET/CT. Eur J Nucl Med Mol Imaging. 2019;46:2569–80. https://doi.org/10.1007/s00259-019-04444-y.
Koerber SA, Staudinger F, Kratochwil C, Adeberg S, Haefner MF, Ungerechts G, et al. The role of (68)Ga-FAPI PET/CT for patients with malignancies of the lower gastrointestinal tract: first clinical experience. J Nucl Med. 2020;61:1331–6. https://doi.org/10.2967/jnumed.119.237016.
Shi X, Xing H, Yang X, Li F, Yao S, Zhang H, et al. Fibroblast imaging of hepatic carcinoma with (68)Ga-FAPI-04 PET/CT: a pilot study in patients with suspected hepatic nodules. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-020-04882-z.
Wei Y, Cheng K, Fu Z, Zheng J, Mu Z, Zhao C, et al. [18F]AlF-NOTA-FAPI-04 PET/CT uptake in metastatic lesions on PET/CT imaging might distinguish different pathological types of lung cancer. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-021-05638-z.
Wang L, Tang G, Hu K, Liu X, Zhou W, Li H, et al. Comparison of (68)Ga-FAPI and (18)F-FDG PET/CT in the evaluation of advanced lung cancer. Radiology. 2022:211424. https://doi.org/10.1148/radiol.211424.
Chen H, Pang Y, Wu J, Zhao L, Hao B, Wu J, et al. Comparison of [(68)Ga]Ga-DOTA-FAPI-04 and [(18)F] FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer. Eur J Nucl Med Mol Imaging. 2020;47:1820–32. https://doi.org/10.1007/s00259-020-04769-z.
Detterbeck FC, Boffa DJ, Kim AW, Tanoue LT. The eighth edition lung cancer stage classification. Chest. 2017;151:193–203. https://doi.org/10.1016/j.chest.2016.10.010.
Kakinuma R, Noguchi M, Ashizawa K, Kuriyama K, Maeshima AM, Koizumi N, et al. Natural history of pulmonary subsolid nodules: a prospective multicenter study. J Thorac Oncol. 2016;11:1012–28. https://doi.org/10.1016/j.jtho.2016.04.006.
Mattes MD, Weber WA, Foster A, Moshchinsky AB, Ahsanuddin S, Zhang Z, et al. A predictive model for lymph node involvement with malignancy on PET/CT in non-small-cell lung cancer. J Thorac Oncol. 2015;10:1207–12. https://doi.org/10.1097/jto.0000000000000601.
Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005;236:1011–9. https://doi.org/10.1148/radiol.2363041310.
Giesel FL, Heussel CP, Lindner T, Röhrich M, Rathke H, Kauczor H-U, et al. FAPI-PET/CT improves staging in a lung cancer patient with cerebral metastasis. Eur J Nucl Med Mol Imaging. 2019;46:1754–5. https://doi.org/10.1007/s00259-019-04346-z.
Maiga AW, Deppen SA, Mercaldo SF, Blume JD, Montgomery C, Vaszar LT, et al. Assessment of fluorodeoxyglucose F18-labeled positron emission tomography for diagnosis of high-risk lung nodules. JAMA Surg. 2018;153:329–34. https://doi.org/10.1001/jamasurg.2017.4495.
Röhrich M, Leitz D, Glatting FM, Wefers AK, Weinheimer O, Flechsig P, et al. Fibroblast activation protein specific PET/CT imaging in fibrotic interstitial lung diseases and lung cancer: a translational exploratory study. J Nucl Med. 2021. https://doi.org/10.2967/jnumed.121.261925.
Konishi J, Yamazaki K, Tsukamoto E, Tamaki N, Onodera Y, Otake T, et al. Mediastinal lymph node staging by FDG-PET in patients with non-small cell lung cancer: analysis of false-positive FDG-PET findings. Respiration. 2003;70:500–6. https://doi.org/10.1159/000074207.
Al-Sarraf N, Gately K, Lucey J, Wilson L, McGovern E, Young V. Lymph node staging by means of positron emission tomography is less accurate in non-small cell lung cancer patients with enlarged lymph nodes: analysis of 1,145 lymph nodes. Lung Cancer. 2008;60:62–8. https://doi.org/10.1016/j.lungcan.2007.08.036.
De Leyn P, Lardinois D, Van Schil P, Rami-Porta R, Passlick B, Zielinski M, et al. European trends in preoperative and intraoperative nodal staging: ESTS guidelines. J Thorac Oncol. 2007;2:357–61. https://doi.org/10.1097/01.JTO.0000263722.22686.1c.
Serfling S, Zhi Y, Schirbel A, Lindner T, Meyer T, Gerhard-Hartmann E, et al. Improved cancer detection in Waldeyer’s tonsillar ring by (68)Ga-FAPI PET/CT imaging. Eur J Nucl Med Mol Imaging. 2021;48:1178–87. https://doi.org/10.1007/s00259-020-05055-8.
Funding
The current research was financially supported by the Natural Science Foundation of Beijing project 7202027; National Natural Science Foundation of China 81871387, 81671733, 81871386, and 82001857; and Science Foundation of Peking University Cancer Hospital-2021–18.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Peking University Cancer Hospital (2019 KT95); oral and written informed consent was obtained from all participants.
Consent for publication
Not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology—Chest
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, X., Wang, S., Xu, X. et al. Higher accuracy of [68 Ga]Ga-DOTA-FAPI-04 PET/CT comparing with 2-[18F]FDG PET/CT in clinical staging of NSCLC. Eur J Nucl Med Mol Imaging 49, 2983–2993 (2022). https://doi.org/10.1007/s00259-022-05818-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05818-5