Abstract
Purpose
To explore the expression of fibroblast activation protein (FAP) in lung cancer (LC) and its correlation with tumor glucose metabolism and histopathology.
Methods
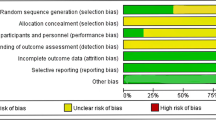
From June 2018 to November 2020, 73 patients with newly diagnosed LC were included. Immunohistochemical staining was used to quantify FAP expression in tumors. The histopathological type and tumor grade were determined via histopathological examination. The tumor glucose metabolism parameters and tumor maximal diameter were measured via [18F] F-FDG PET/CT. Univariate and multivariate analysis were performed to study the correlation of FAP expression levels with glucose metabolism variables and tumor histopathology.
Results
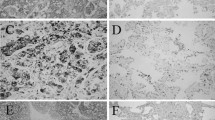
Positive FAP expression was observed in 97.3% (71/73) LC lesions, which was significantly higher than 87.7% (64/73) of [18F] F-FDG positivity observed on PET/CT (χ2 = 4.818, P = 0.028). In 12 early adenocarcinomas (ADCs), only three lesions (25%) were positive for [18F] F-FDG on PET/CT; however, 10 lesions (83.3%) were positive for FAP. When FAP expression was classified into low level (scores ≤ 3) and high level (scores > 4), high FAP level was found in 80.8% tumors and low FAP level in the other 19.2% tumors. High FAP level was identified in 100.0% of squamous cell carcinomas (SCCs), 85.7% of ADCs, 66.7% (4/6) of large cell neuroendocrine carcinomas (LCNCs), and 40.0% (4/10) of small cell lung cancers (SCLCs) (P < 0.05). In non-mucinous ADC lesions, on univariate analysis, FAP expression level showed a close relationship with tumor metabolism parameters (maximal standard uptake value (SUVmax), mean standard uptake value (SUVmean), and total lesion glycolysis (TLG)), tumor diameter, tumor grade, and lesion attenuation (P < 0.05).
Conclusion
The present study demonstrates that FAP is widely expressed in LC and shows great variation in different histopathological types. A high positive rate of FAP expression implies that FAP-targeted imaging may be a sensitive modality for diagnosing LC, especially in early ADCs. Further validation with such probes is warranted.





Similar content being viewed by others
Data availability
All data were transparent. The data used in the current study are available from the corresponding author on reasonable request.
References
Bray F, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. https://doi.org/10.3322/caac.21492.
de Sousa VML, Carvalho L. Heterogeneity in lung cancer. Pathobiology. 2018;85:96–107. https://doi.org/10.1159/000487440.
Jain D. Lung molecular cytopathology: EGFR and beyond. J Cytol. 2019;36:124–7. https://doi.org/10.4103/JOC.JOC_135_18.
Nurmik M, Ullmann P, Rodriguez F, Haan S, Letellier E. In search of definitions: cancer-associated fibroblasts and their markers. Int J Cancer. 2020;146:895–905. https://doi.org/10.1002/ijc.32193.
Yu DM, et al. The dipeptidyl peptidase IV family in cancer and cell biology. FEBS J. 2010;277:1126–44. https://doi.org/10.1111/j.1742-4658.2009.07526.x.
Chen L, Qiu X, Wang X, He J. FAP positive fibroblasts induce immune checkpoint blockade resistance in colorectal cancer via promoting immunosuppression. Biochem Biophys Res Commun. 2017;487:8–14. https://doi.org/10.1016/j.bbrc.2017.03.039.
Mankaney G, et al. Gastric cancer in FAP: a concerning rise in incidence. Fam Cancer. 2017;16:371–6. https://doi.org/10.1007/s10689-017-9971-3.
Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–7. https://doi.org/10.1038/nature03096.
Hamson EJ, Keane FM, Tholen S, Schilling O, Gorrell MD. Understanding fibroblast activation protein (FAP): substrates, activities, expression and targeting for cancer therapy. Proteomics Clin Appl. 2014;8:454–63. https://doi.org/10.1002/prca.201300095.
Giesel FL, et al. (68)Ga-FAPI PET/CT: Biodistribution and preliminary dosimetry estimate of 2 DOTA-containing FAP-targeting agents in patients with various cancers. J Nucl Med. 2019;60:386–92. https://doi.org/10.2967/jnumed.118.215913.
Kratochwil C, et al. (68)Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer. J Nucl Med. 2019;60:801–5. https://doi.org/10.2967/jnumed.119.227967.
Castello A, Rossi S, Lopci E. 18F-FDG PET/CT in restaging and evaluation of response to therapy in lung cancer: state of the art. Curr Radiopharm. 2020;13:228–37. https://doi.org/10.2174/1874471013666191230144821.
Sharma A, et al. Utility of early dynamic and delayed post-diuretic (18)F-FDG PET/CT SUVmax in predicting tumour grade and T-stage of urinary bladder carcinoma: results from a prospective single centre study. Br J Radiol. 2017;90:20160787. https://doi.org/10.1259/bjr.20160787.
Guo J, et al. VEGF-A and its isoform VEGF(1)(2)(1) mRNA expression measured by quantitative real-time RT-PCR: correlation with F-18 FDG uptake and aggressiveness of lung adenocarcinoma: preliminary study. Ann Nucl Med. 2011;25:29–36. https://doi.org/10.1007/s12149-010-0427-1.
Ruilong Z, et al. Diagnostic value of 18F-FDG-PET/CT for the evaluation of solitary pulmonary nodules: a systematic review and meta-analysis. Nucl Med Commun. 2017;38:67–75. https://doi.org/10.1097/MNM.0000000000000605.
Badawi RD, et al. First human imaging studies with the EXPLORER total-body PET scanner. J Nucl Med. 2019;60:299–303. https://doi.org/10.2967/jnumed.119.226498.
Ren YY, et al. Whole-body (18)F-FDG PET/CT for M staging in the patient with newly diagnosed nasopharyngeal carcinoma: Who needs? Eur J Radiol. 2017;89:200–7. https://doi.org/10.1016/j.ejrad.2017.02.002.
Travis WD, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244–85. https://doi.org/10.1097/JTO.0b013e318206a221.
Nakamura H, et al. Close association of IASLC/ATS/ERS lung adenocarcinoma subtypes with glucose-uptake in positron emission tomography. Lung Cancer. 2015;87:28–33. https://doi.org/10.1016/j.lungcan.2014.11.010.
Liao Y, Ni Y, He R, Liu W, Du J. Clinical implications of fibroblast activation protein-alpha in non-small cell lung cancer after curative resection: a new predictor for prognosis. J Cancer Res Clin Oncol. 2013;139:1523–8. https://doi.org/10.1007/s00432-013-1471-8.
Koustoulidou S, et al. Cancer-associated fibroblasts as players in cancer development and progression and their role in targeted radionuclide imaging and therapy. Cancers (Basel). 2021;13:1100. https://doi.org/10.3390/cancers13051100.
Fischer E, et al. Radioimmunotherapy of fibroblast activation protein positive tumors by rapidly internalizing antibodies. Clin Cancer Res. 2012;18:6208–18. https://doi.org/10.1158/1078-0432.CCR-12-0644.
Loktev A, et al. A tumor-imaging method targeting cancer-associated fibroblasts. J Nucl Med. 2018;59:1423–9. https://doi.org/10.2967/jnumed.118.210435.
Giesel FL, et al. FAPI-74 PET/CT using either (18)F-AlF or cold-kit (68)Ga labeling: biodistribution, radiation dosimetry, and tumor delineation in lung cancer patients. J Nucl Med. 2021;62:201–7. https://doi.org/10.2967/jnumed.120.245084.
Hao B, Wu J, Pang Y, Sun L, Chen H. 68Ga-FAPI PET/CT in assessment of leptomeningeal metastases in a patient with lung adenocarcinoma. Clin Nucl Med. 2020;45:784–6. https://doi.org/10.1097/RLU.0000000000003231.
Loutfi S, Khankan A, Al Ghanim S. Guidelines for multimodality radiological staging of lung cancer. J Infect Public Health. 2012;5(Suppl 1):S14-21. https://doi.org/10.1016/j.jiph.2012.09.009.
Wood DE, et al. Lung Cancer Screening, Version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16:412–41. https://doi.org/10.6004/jnccn.2018.0020.
Nomori H, et al. Evaluation of F-18 fluorodeoxyglucose (FDG) PET scanning for pulmonary nodules less than 3 cm in diameter, with special reference to the CT images. Lung Cancer. 2004;45:19–27. https://doi.org/10.1016/j.lungcan.2004.01.009.
Chen H, Pang Y, Meng T, Yu X, Sun L. 18F-FDG and 68Ga-FAPI PET/CT in the evaluation of ground-glass opacity nodule. Clin Nucl Med. 2021;46:424–6. https://doi.org/10.1097/RLU.0000000000003600.
Wei Y, et al. [(18)F]AlF-NOTA-FAPI-04 PET/CT uptake in metastatic lesions on PET/CT imaging might distinguish different pathological types of lung cancer. Eur J Nucl Med Mol Imaging. 2021. https://doi.org/10.1007/s00259-021-05638-z.
Moreno-Ruiz P, et al. Stromal FAP is an independent poor prognosis marker in non-small cell lung adenocarcinoma and associated with p53 mutation. Lung Cancer. 2021;155:10–9. https://doi.org/10.1016/j.lungcan.2021.02.028.
Acknowledgements
We are grateful to Prof Deng Yongjian, a pathologist, and his team in Nanfang Hospital, for providing direction in pathologic diagnoses and immunohistochemical staining and scores.
Funding
This work was supported financially by the National Science Foundation of China under grants 81873905.
Author information
Authors and Affiliations
Contributions
Conceptualization: Hubing Wu
Formal analysis and investigation: Xiaohui Chen, Xinran Liu, Lijuan Wang, Wenlan Zhou, Yin Zhang, Ying Tian, Jianer Tan, Ye Dong, Lilan Fu, Hubing Wu
Writing-original draft preparation: Xiaohui Chen, Xinran Liu, Lijuan Wang
Writing-review and editing: Hubing Wu
Funding acquisition: Hubing Wu
Supervision: Hubing Wu
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of Southern Medical University in view of the retrospective nature of the study.
Consent to participate
Due to the retrospective nature of the study, informed consent was not obtained in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - Chest
Rights and permissions
About this article
Cite this article
Chen, X., Liu, X., Wang, L. et al. Expression of fibroblast activation protein in lung cancer and its correlation with tumor glucose metabolism and histopathology. Eur J Nucl Med Mol Imaging 49, 2938–2948 (2022). https://doi.org/10.1007/s00259-022-05754-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05754-4