Abstract
Purpose
PET image quality is influenced by the patient size according to the current guideline. The study aimed to propose an optimized dose regimen to yield a constant image quality independent of patient habitus to meet the clinical needs.
Methods
A first patient cohort of 78 consecutive oncological patients (59.7 ± 13.7 years) who underwent a total-body PET/CT scan were retrospectively enrolled to develop the regimen. The patients were randomly distributed in four body mass index (BMI) groups according to the World Health Organization (WHO) criteria. The liver SNR (signal-to-noise ratio, SNRL) was obtained by manually drawing regions of interest (ROIs) and normalized (SNRnorm) by the product of injected activity and acquisition time. Fits of SNRnorm against different patient-dependent parameters were performed to determine the best correlating parameter and fit method. A qualitative assessment on image quality was performed using a 5-point Likert scale to determine the acceptable threshold of SNRL. Thus, an optimized regimen was proposed and validated by a second patient cohort consisted of prospectively enrolled 38 oncological patients.
Results
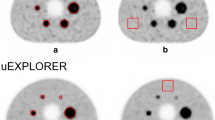
The linear fit showed SNRnorm had the strongest correlation (R2 = 0.69) with the BMI than other patient-dependent parameters and fit method. The qualitative assessment indicated a SNRL value of 14.0 as an acceptable threshold to achieve sufficient image quality. The optimized dose regimen was determined as a quadratic relation with BMI: injected activity (MBq) = 39.2 (MBq)/(− 0.03*BMI + 1.49)2. In the validation study, the SNRL no longer decreased with the increase of BMI. There was no significant difference of the image quality regarding the value of SNRL between different BMI groups (p > 0.05). In addition, the injected activity was reduced by 75.6 ± 2.9%, 72.1 ± 4.0%, 67.1 ± 4.4%, and 64.8 ± 3.5% compared with the first cohort for the four BMI groups, respectively.
Conclusion
The study proposed a quadratic relation between the 18F-FDG injected activity and the patient’s BMI for total-body 18F-FDG PET imaging. In this regimen, the image quality can maintain in a constant level independent of patient habitus and meet the clinical requirement with a reduced injected activity.







Similar content being viewed by others
References
Bosch KD, Chicklore S, Cook GJ, Davies AR, Kelly M, Gossage JA, et al. Staging FDG PET-CT changes management in patients with gastric adenocarcinoma who are eligible for radical treatment. Eur J Nucl Med Mol Imaging. 2020;47(4):759–67. https://doi.org/10.1007/s00259-019-04429-x.
Wang H, Zhao S, Li L, Tian R. Development and validation of an (18)F-FDG PET radiomic model for prognosis prediction in patients with nasal-type extranodal natural killer/T cell lymphoma. Eur Radiol. 2020;30(10):5578–87. https://doi.org/10.1007/s00330-020-06943-1.
Broccoli A, Nanni C, Cappelli A, Bacci F, Gasbarrini A, Tabacchi E, et al. Diagnostic accuracy of positron emission tomography/computed tomography-driven biopsy for the diagnosis of lymphoma. Eur J Nucl Med Mol Imaging. 2020;47(13):3058–65. https://doi.org/10.1007/s00259-020-04913-9.
Kang F, Mu W, Gong J, Wang S, Li G, Li G, et al. Integrating manual diagnosis into radiomics for reducing the false positive rate of (18)F-FDG PET/CT diagnosis in patients with suspected lung cancer. Eur J Nucl Med Mol Imaging. 2019;46(13):2770–9. https://doi.org/10.1007/s00259-019-04418-0.
Lopci E, Mascarin M, Piccardo A, Castello A, Elia C, Guerra L, et al. FDG PET in response evaluation of bulky masses in paediatric Hodgkin’s lymphoma (HL) patients enrolled in the Italian AIEOP-LH2004 trial. Eur J Nucl Med Mol Imaging. 2019;46(1):97–106. https://doi.org/10.1007/s00259-018-4155-4.
Cherry SR, Jones T, Karp JS, Qi J, Moses WW, Badawi RD. Total-Body PET: Maximizing Sensitivity to Create New Opportunities for Clinical Research and Patient Care. J Nucl Med. 2018;59(1):3–12. https://doi.org/10.2967/jnumed.116.184028.
Zhang YQ, Hu PC, Wu RZ, Gu YS, Chen SG, Yu HJ, et al. The image quality, lesion detectability, and acquisition time of 18F-FDG total-body PET/CT in oncological patients. Eur J Nucl Med Mol Imaging. 2020;47(11):2507–15. https://doi.org/10.1007/s00259-020-04823-w.
Tan H, Sui X, Yin H, Yu H, Gu Y, Chen S, et al. Total-body PET/CT using half-dose FDG and compared with conventional PET/CT using full-dose FDG in lung cancer. Eur J Nucl Med Mol Imaging. 2021;48(6):1966–75. https://doi.org/10.1007/s00259-020-05091-4.
Liu G, Hu P, Yu H, Tan H, Zhang Y, Yin H, et al. Ultra-low-activity total-body dynamic PET imaging allows equal performance to full-activity PET imaging for investigating kinetic metrics of 18F-FDG in healthy volunteers. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-020-05173-3
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54. https://doi.org/10.1007/s00259-014-2961-x.
Tahari AK, Chien D, Azadi JR, Wahl RL. Optimum lean body formulation for correction of standardized uptake value in PET imaging. J Nucl Med. 2014;55(9):1481–4. https://doi.org/10.2967/jnumed.113.136986.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1–253
Janmahasatian S, Duffull SB, Ash S, Ward LC, Byrne NM, Green B. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44(10):1051–65. https://doi.org/10.2165/00003088-200544100-00004.
Cox CPW, Segbers M, Graven LH, Brabander T, van Assema DME. Standardized image quality for 68Ga-DOTA-TATE PET/CT. EJNMMI Res. 2020;10(1):27. https://doi.org/10.1186/s13550-020-0601-y.
de Groot EH, Post N, Boellaard R, Wagenaar NR, Willemsen AT, van Dalen JA. Optimized dose regimen for whole-body FDG-PET imaging. EJNMMI Res. 2013;3(1):63. https://doi.org/10.1186/2191-219X-3-63.
Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, et al. Procedure guideline for tumor imaging with 18F-FDG PET/CT 1.0. J Nucl Med. 2006;47(5):885–95.
Mizuta T, Senda M, Okamura T, Kitamura K, Inaoka Y, Takahashi M, et al. NEC density and liver ROI S/N ratio for image quality control of whole-body FDG-PET scans: comparison with visual assessment. Mol Imaging Biol. 2009;11(6):480–6. https://doi.org/10.1007/s11307-009-0214-3.
Büsing KA, Schönberg SO, Brade J, Wasser K. Impact of blood glucose, diabetes, insulin, and obesity on standardized uptake values in tumors and healthy organs on 18F-FDG PET/CT. Nucl Med Biol. 2013;40(2):206–13. https://doi.org/10.1016/j.nucmedbio.2012.10.014.
Laffon E, Adhoute X, de Clermont H, Marthan R. Is liver SUV stable over time in 18F-FDG PET imaging? J Nucl Med Technol. 2011;39(4):258–63. https://doi.org/10.2967/jnmt.111.090027.
Funding
This study is supported by the Three-year Action Plan of Clinical Skills and Innovation of Shanghai Hospital Development Center (grant number: SHDC2020CR3079B), and Science and Technology Committee of Shanghai Municipality (20DZ2201800), Special Fund for Clinical Research, Young Program of Zhongshan Hospital of Fudan University (2018ZSQN38, 2019ZSYQ28, 2020ZSLC63) young program of Zhongshan Hospital and Shanghai "Rising Stars of Medical Talent"-Youth Development Program (HWJRS2019-720), the Shanghai Municipal Key Clinical Specialty Project (Grant number: SHSLCZDZK03401).
Author information
Authors and Affiliations
Contributions
Jie Xiao was involved in the statistical analysis and manuscript writing. Haojun Yu contributed to data acquisition and reconstructions. Xiuli Sui and Yan Hu contributed to data analyses and image interpretation. Guobing Liu and Yanyan Cao helped with data processing. Yiqiu Zhang and Pengcheng Hu supervised the study. Ying Wang and Chenwei Li were with editing English grammar. Hongcheng Shi and Baixuan Xu designed the study and contributed to editing and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Ying Wang and Chenwei Li are employees of United Imaging Healthcare. The other authors who are working in Zhongshan Hospital or Chinese PLA General Hospital have full control of the data and declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Technology
Supplementary Information
ESM 1
(DOCX 102 kb)
Rights and permissions
About this article
Cite this article
Xiao, J., Yu, H., Sui, X. et al. Can the BMI-based dose regimen be used to reduce injection activity and to obtain a constant image quality in oncological patients by 18F-FDG total-body PET/CT imaging?. Eur J Nucl Med Mol Imaging 49, 269–278 (2021). https://doi.org/10.1007/s00259-021-05462-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05462-5