Abstract
Aim
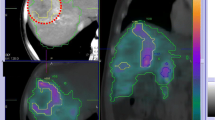
Transarterial radioembolization (TARE) is, by all standards, a radiation therapy. As such, according to Euratom Directive 2013/59, it should be optimized by a thorough treatment plan based on the distinct evaluation of absorbed dose to the lesions and to the non-tumoural liver (two-compartment dosimetry). Since the dosimetric prediction with 99mTc albumin macro-aggregates (MAA) of non-tumoural liver is much more accurate than the same prediction on lesions, treatment planning should focus on non-tumoural liver rather than on lesion dosimetry. The aim of this study was to determine a safety limit through the analysis of pre-treatment dosimetry with 99mTc-MAA single photon emission computed tomography (SPECT/CT), in order to deliver the maximum tolerable absorbed dose to non-tumoural liver.
Methods
Data from intermediate/advanced hepato-cellular carcinoma (HCC) patients treated with 90Y glass microspheres were collected in this single-arm retrospective study. Injection was always lobar, even in case of bilobar disease, to avoid treating the whole liver in a single session. A three-level definition of liver decompensation (LD) was introduced, considering toxicity only in cases of liver decompensation requiring medical action (LD type C, LDC). We report LDC rates, receiver operating characteristic (ROC) analysis between LDC and NO LDC absorbed dose distributions, normal tissue complication probability (NTCP) curves and uni- and multivariate analysis of risk factors associated with toxicity.
Results
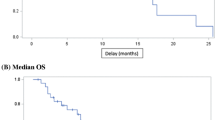
A 6-month timeline was defined as necessary to capture all treatment-related toxicity events. Previous transarterial chemoembolization (TACE), presence or extension of portal vein tumoural thrombosis (PVTT) and tumour pattern (nodular versus infiltrative) were not associated with tolerance to TARE. On the contrary, at the multivariate analysis, the absorbed dose averaged over the whole non-tumoural liver (including the non-injected lobe) was a prognostic indicator correlated with liver decompensation (odds ratio = 4.24). Basal bilirubin > 1.1 mg/dL was a second even more significant risk factor (odds ratio = 6.35). NTCP analysis stratified with this bilirubin cut-off determined a 15% liver decompensation risk at 50 Gy/90 Gy for bilirubin >/< 1.1 mg/dL. These results are valid for a 90Y glass microsphere administration 4 days after the reference time.
Conclusion
Given the low predictive accuracy of 99mTc-MAA on lesion absorbed dose reported by several authors, an optimized TARE with 90Y glass microspheres with lobar injection 4 days after reference time should aim at an absorbed dose averaged over the whole non-tumoural liver of 50 Gy/90 Gy for basal bilirubin higher/lower than 1.1 mg/dL, respectively.







Similar content being viewed by others
References
Cremonesi M, Chiesa C, Strigari L, Ferrari M, Botta F, Guerriero F, et al. Radioembolization of hepatic lesions from a radiobiology and dosimetric perspective. Front Oncol. 2014;19:4–210. https://doi.org/10.3389/fonc.2014.00210.
Sposito C, Mazzaferro V. The SIRveNIB and SARAH trials, radioembolization vs. sorafenib in advanced HCC patients: reasons for a failure, and perspectives for the future. Hepatobiliary Surg Nutr. 2018;7(6):487–9.
Bastiaannet R, Kappadath SC, Kunnen B, Braat AJAT, Lam MGEH, de Jong HWAM. The Physics of Radioembolization. Eur J Nucl Med Mol Im Physics. 2018;5(1):22.
Gnesin S, Canetti L, Adib S, Cherbuin N, Silva Monteiro M, Bize P, et al. Partition Model-Based 99mTc-MAA SPECT/CT Predictive Dosimetry Compared with 90Y TOF PET/CT Posttreatment Dosimetry in Radioembolization of Hepatocellular Carcinoma: A Quantitative Agreement Comparison. J Nucl Med. 2016;57(11):1672–8.
Jadoul A, Bernard C, Lovinfosse P, Gérard L, Lilet H, Cornet O, et al. Comparative dosimetry between 99mTc-MAA SPECT/CT and 90Y PET/CT in primary and metastatic liver tumours. Eur J Nucl Med Mol Imaging. 2020;47(4):828–37.
Haste P, Tann M, Persohn S, LaRoche T, Aaron V, Mauxion T, et al. Correlation of Technetium-99 m Macroaggregated Albumin and Yttrium-90 Glass Microsphere Biodistribution in Hepatocellular Carcinoma: A Retrospective Review of Pretreatment Single Photon Emission CT and Posttreatment Positron Emission Tomography/CT. J Vasc Interv Radiol. 2017;28:722–30.
Chiesa C, Maccauro M. 166Ho microsphere scout dose for more accurate radioembolization treatment planning. Eur J Nucl Med Mol Imaging. 2020;47(4):744–7.
Chiesa C, Maccauro M, Romito R, Spreafico C, Pellizzari S, Negri A, et al. Need, feasibility and convenience of dosimetric treatment planning in liver selective internal radiation therapy with 90Y microspheres: the experience of the National Cancer Institute of Milan. Q J Nucl Med Mol Im. 2011;55:168–97.
Mazzaferro V, Sposito C, Bhoori S, Romito R, Chiesa C, Morosi C, et al. Yttrium90 radioembolization for intermediate-advanced hepatocarcinoma: a phase II study. Hepatology. 2013;57(5):1826–37.
Chiesa C, Mira M, Maccauro M, Spreafico C, Romito R, Morosi C, et al. Radioembolization of Hepatocarcinoma with 90-Y Glass Microspheres: Development of an Individualized Treatment Planning Strategy based on Dosimetry and Radiobiology. Eur J Nucl Med Mol Im. 2015;42:1718–38.
Spreafico C, Sposito C, Vaiani M, Cascella T, Bhoori S, Morosi C, et al. Development of a prognostic score to predict response to yttrium-90 radioembolization for hepatocellular carcinoma with portal vein invasion. J Hep. 2018;68:724–32.
Botta F, Ferrari M, Chiesa C, Vitali S, Guerriero F, Nile MC, et al. Impact of missing attenuation and scatter corrections on 99m Tc-MAA SPECT 3D dosimetry for liver radioembolization using the patient relative calibration methodology: A retrospective investigation on clinical images. Med Phys. 2018;45(4):1684–98.
Garin E, Rolland Y, Laffont S, Edeline J. Clinical impact of 99mTc-MAA SPECT/CT-based dosimetry in the radioembolization of liver malignancies with 90Y-loaded Microspheres. Eur J Nucl Med Mol Imaging. 2016;43:559–75.
Goin JE, Salem R, Carr BI, Dancey JE, Soulen MC, Geschwind JFH, et al. Treatment of unresecable hepatocellular carcinoma with intrahepatic yttrium-90 microspheres: factors associated with liver toxicities. J Vasc Interv Radiology. 2005;16:205–13.
Braat MNGJA, van Erpecum KJ, Zonnenberg BA, van den Bosch MAJ, Lam MGEH. Radioembolization-induced liver disease: a systematic review. Eur J Gastroenterol Hepatol. 2016;29:144–52.
Srinivas SM, Natarajan N, Kuroiwa J, et al. Determination of radiation absorbed dose to primary liver tumours and normal liver tissue using post-radioembolization 90Y PET. Front Oncol. 2014;4:255.
Hilgard P, Hamami M, El Fouly A, Scherag A, Müller S, Ertle et al. Radioembolization with yttrium-90 glass microspheres in hepatocellular carcinoma: European Experience on Safety and Long-Term Survival. Hepatology 2010;52:1741–1749
Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, et al. Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010;138(1):52–64.
Andrews JC, Walker SC, Ackermann RJ, et al. Hepatic Radioembolization with Yttrium-90 Containing Glass Microspheres: Preliminary Results and Clinical Follow-Up. J Nucl Med. 1994;35:1637–44.
Strigari L, Sciuto R, Rea S, Carpanese L, Pizzi G, Soriani A, et al. Efficacy and toxicity related to treatment of hepatocellular carcinoma with 90Y SIR spheres: radiobiological considerations. J Nucl Med. 2010;51:1377–85.
Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21(1):109–22.
Burman C, Kutcher GJ, Emami B, Goitein M. Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys. 1991;21(1):123–35.
Dawson LA, Ten Haken RK. Partial volume tolerance of the liver to radiation. Sem in rad onc. 2005;15:279–83.
Salem R, Padia SA, Lam M, Bell J, Chiesa C, Fowers K, et al. Clinical and dosimetric considerations for Y90: recommendations from an international multidisciplinary working group. Eur J Nucl Med Mol Imaging. 2019;46(8):1695–704.
Spreafico C, Maccauro M, Mazzaferro V, Chiesa C. The dosimetric importance of the number of 90Y microspheres in liver transarterial radioembolization (TARE). Eur J Nucl Med Mol Imaging. 2014;41:634–8.
Walrand S, Hesse M, Chiesa C, Lhommel R, Jamar F. The low hepatic toxicity per Gy of 90Y glass microspheres is linked to their transport in the arterial tree favouring a non-uniform trapping as observed in posttherapy PET imaging. J Nucl Med. 2014;55:135–40.
Garin E, Lenoir L, Edeline J, Laffont S, Mesbah H, Porée P, et al. Boosted selective internal radiation therapy with 90Y-loaded glass microspheres (B-SIRT) for hepatocellular carcinoma patients: a new personalized promising concept. Eur J Nucl Med Mol Imaging. 2013;40:1057–68.
Garin E, Rolland Y, Pracht M, Le Sourd S, Laffont S, Mesbah H, et al. High impact of macroaggregated albumin-based tumour dose on response and overall survival in hepatocellular carcinoma patients treated with 90Y-loaded glass microsphere radioembolization. Liver International. 2017;37:101–10.
Young JY, Rhee TK, Atassi B, Gates VL, Kulik L, Mulcahni MF, et al. Radiation dose limits and liver toxicities resulting from multiple yttrium-90 radioembolization treatments for hepatocellular carcinoma. J Vasc Interv Radiol. 2007;18:1375–82.
Sangro B, Gil-Alzugaray B, Rodriguez J, Sola I, Martinez-Cuesta A, Viudez A, et al. Liver disease induced by radioembolization of liver tumours: description and possible risk factors. Cancer. 2008;112:1538–46.
Gil-Alzugaray B, Chopitea A, Inarrairaegui M, Bilbao JI, Rodriguez-Fraile M, Rodriguez J, et al. Prognostic Factors and Prevention of Radioembolization-Induced Liver Disease Hepatology. 2013;57:1078–87.
Pacilio M, Ferrari M, Chiesa C, Lorenzon L, Mira M, Botta F, et al. 3D dosimetry treatment planning with 99mTc-macroaggregated albumin SPECT in radioembolization with 90Y microspheres: a Monte Carlo study of the impact on absorbed dose distributions of attenuation and scatter corrections using the patient relative calibration methodology. Medical Physics. 2016;43:4053–64.
Acknowledgements
We thank Dr. Kirk Fowers of BTG Biocompatibles L.t.d. for useful discussions and suggestions. We acknowledge nuclear medicine technicians Monica Testoni, Dehborah Mansi, Sergio Bavusi, Consuelo Zanette, Rossana Pavesi and Marco Magistretti and CT technicians Roberto Gallo, Pietro Basile and Vanni Tirella for retrieving patient scans. We also acknowledge the head of nurses Rita Sicari for patient management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Carlo Chiesa received honoraria for consultancies from BTG Biocompatibles and Terumo. He also received a research grant from BTG Biocompatibles for this Investigator Initiated Study.
Marta Mira received a 15-month research grant from BTG Biocompatibles in order to perform this study.
Marco Maccauro, Carlo Spreafico, Sherrie Bhoori and Vincenzo Mazzaferro received honoraria as consultant and speakers from BTG Biocompatibles.
All the other authors have nothing to disclose.
Research on humans
The present Investigator Initiated Study (SPETc-DOSE-1) and the grant from BTG Biocompatibles were approved by the Ethics Committee and by the legal office of our Institution Fondazione IRCCS Istituto Nazionale Tumori (Committee for Trials on New Diagnostic and Therapeutic Methods—Comitato per la Sperimentazione dei Nuovi Metodi Diagnostici e Terapeutici, protocol number INT/99/17 Q/17/063). Our research has been performed in accordance with the ethical standards as cited in the 1964 Declaration of Helsinki.
Informed consent, for Cohort 3 thoroughly explaining the dosimetric optimization of treatment, was obtained from all patients before the 99mTc-MAA angioscintigraphic session (simulation). For Cohort 1, informed consent for the whole radioembolization procedure according to TheraSphere indication was obtained from all patients within the prospective phase II study [9].
Consent to retrospective clinical data collection was conducted according to the Italian legislation valid during the study. The corresponding author and P.I. of the study, Carlo Chiesa, signed a declaration stating that patients were not reachable at the time of the study since they died before the beginning of data collection.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The medical physicist Marta Mira was temporarily supported for the present Investigator Initiated Study with a research grant received from BTG Biocompatibles L.t.d.
This article is part of the Topical Collection on Dosimetry.
Electronic supplementary material
ESM 1
(DOCX 60 kb)
Rights and permissions
About this article
Cite this article
Chiesa, C., Mira, M., Bhoori, S. et al. Radioembolization of hepatocarcinoma with 90Y glass microspheres: treatment optimization using the dose-toxicity relationship. Eur J Nucl Med Mol Imaging 47, 3018–3032 (2020). https://doi.org/10.1007/s00259-020-04845-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04845-4