Abstract
Purpose
Diffuse large B-cell lymphoma (DLBCL) represents the most common subtype of non-Hodgkin lymphoma. Most relapses occur in the first 2 years after diagnosis. Early response assessment with 18F-fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography (PET) may facilitate early change of treatment, thereby preventing ineffective treatment and unnecessary side effects. We aimed to assess the predictive value of visually-assessed interim 18F-FDG PET on progression-free survival (PFS) or event-free survival (EFS) in DLBCL patients treated with first-line immuno-chemotherapy regimens.
Methods
For this systematic review and meta-analysis Pubmed, Embase, and the Cochrane Library were searched until July 11, 2017. Prospective and retrospective studies investigating qualitative interim PET response assessment without treatment adaptation based on the interim PET result were eligible. The primary outcome was two-year PFS or EFS. Prognostic and diagnostic measures were extracted and analysed with pooled hazard ratios and Hierarchical Summary Receiver Operator Characteristic Curves, respectively. Meta-regression was used to study covariate effects.
Results
The pooled hazard ratio for 18 studies comprising 2,255 patients was 3.13 (95%CI 2.52–3.89) with a 95% prediction interval of 1.68–5.83. In 19 studies with 2,366 patients, the negative predictive value for progression generally exceeded 80% (64–95), but sensitivity (33–87), specificity (49–94), and positive predictive values (20–74) ranged widely.
Conclusions
These findings showed that interim 18F-FDG PET has predictive value in DLBCL patients. However, (subgroup) analyses were limited by lack of information and small sample sizes. Some diagnostic test characteristics were not satisfactory, especially the positive predictive value should be improved, before a successful risk stratified treatment approach can be implemented in clinical practice.
Similar content being viewed by others
Introduction
Diffuse large B-cell lymphoma (DLBCL) represents the most common subtype of adult non-Hodgkin lymphoma (NHL) cases, and is associated with an aggressive clinical course. There are several potentially effective first-line chemotherapy regimens of which most consist of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The addition of the monoclonal antibody rituximab (R) to this regimen (R-CHOP) has significantly improved the outcome of DLBCL patients [1, 2]. However, treatment failure is still an important problem as the 3-year progression-free survival (PFS) of DLBCL patients is approximately 60–70% [3].
Commonly used prognostic indices are the International Prognostic Index (IPI) [4, 5], or the more powerful Revised-IPI (R-IPI) [6], and National Comprehensive Cancer Network IPI (NCCN-IPI) [7]. These indices can be used for risk-stratification to predict a poor outcome after R-CHOP. It is important to identify a poor outcome as soon as possible because these patients could benefit from a switch to a second-line treatment or high-dose chemotherapy (HDCT) with autologous stem cell transplantation (ASCT) as an upfront treatment [8]. 18F-fluoro-2-deoxy-D-glucose (18F-FDG) positron emission tomography (PET) after a few cycles of therapy, also known as interim 18F-FDG PET, is of increasing interest, as it may facilitate early change of treatment and prevent unnecessary side effects [9]. In recent decades several visual criteria for interpretation of 18F-FDG PET have been developed, for example, the EORTC, PERCIST, and International Harmonization Project (IHP) criteria as well as the Deauville scoring system [9,10,11,12,13]. Nowadays the latter is widely adopted for interpretation of response evaluation with 18F-FDG PET in DLBCL [9, 13].
Interim 18F-FDG PET has shown high predictive value in Hodgkin lymphoma [14]; however, according to previous reviews, the role of interim 18F-FDG PET in DLBCL is still unknown [15,16,17,18]. From these studies it can be concluded that heterogeneity in patient populations, therapy regimens, PET scanners, timing of the interim 18F-FDG PET scans, and/or differences in the visual criteria used for interpretation of the interim 18F-FDG PET scans made it hard to clarify the accuracy of interim 18F-FDG PET to predict clinical outcome in DLBCL.
Therefore, we performed a new systematic review and meta-analysis, focusing on DLBCL patients only, assessing both the hazard ratio (HR) and diagnostic parameters (sensitivity, specificity, and predictive values) of interim 18F-FDG PET on PFS or event-free survival (EFS) in patients with DLBCL treated with first-line immuno-chemotherapy regimens. The primary outcome measure was PFS (preferably) or EFS at 2 years, since DLBCL patients who are event-free after 24 months have demonstrated an overall survival (OS) comparable to an age- and sex-matched general population [19]. In order to reduce the previously described heterogeneity we performed several subgroup analyses, for example, by the type of 18F-FDG PET scanner and the type of visual criteria used for interpretation of the interim 18F-FDG PET scans. In this meticulously performed review we contacted the authors for additional information if necessary.
Materials and methods
Search strategy
For this systematic review and meta-analysis we searched in collaboration with a medical librarian Pubmed/MEDLINE, Embase, and the Cochrane Library databases from onset until July 11, 2017 with a language restriction to English, French, Dutch, or German. Our search strategy contained a combination of various indexed terms and free text words for “positron emission tomography” and “non-Hodgkin lymphoma” (full search strategy Supplemental Table 1). We included full-text publications of original prospective and retrospective studies. Excluded were conference abstracts, letters, comments, editorials, review articles, animal studies, and case reports. Reference lists of included articles were checked to identify additional eligible studies.
Study selection: Eligibility criteria
Patients
Adult patients treated with first-line immuno-chemotherapy regimens for stage I-IV DLBCL were considered as our target population. We excluded studies that investigated HIV-related lymphoma, central nervous system (CNS) lymphoma involvement, or post-transplant lymphoproliferative disease (PTLD). Studies containing less than 80% of DLBCL subtype were excluded, unless subgroup data for DLBCL were presented or if the remaining 20% had PMBCL or FL grade 3B [20]. Studies including ten patients or less were classified as case series and therefore also excluded.
Treatment procedures
Studies in which a change of treatment was based on the interim 18F-FDG PET result and prospective PET-adapted trials were not included. However, we allowed a change of therapy in patients with clinical evidence of progressive disease during first-line treatment [9].
We included all R-CHOP-like treatments as first-line treatment strategies [1, 2, 21,22,23], but we excluded studies if ≤50% of patients received rituximab. Therapies using other (new generation) monoclonal antibodies were excluded.
Studies with autologous stem cell transplantation (ASCT) were eligible if this strategy was part of the preplanned first-line treatment. Radiotherapy was accepted if the decision to give radiotherapy was preplanned or used for consolidation of PET positive sites at the end of first-line treatment, but not affected by interim 18F-FDG PET results. If studies did not report on the use of ASCT or radiotherapy, we assumed that no ASCT or radiotherapy was given based on interim 18F-FDG PET result.
Interim 18F-FDG PET procedures
An interim 18F-FDG PET scan should have been performed after the first, second, third, or fourth treatment cycle. PET only as well as PET/CT systems were considered eligible. Use of other radiopharmaceuticals than 18F-FDG were not accepted.
We focused on visual interpretation criteria only, as nowadays, semi-quantitative PET strategies are used for research purposes only and are not standard in the current guidelines yet [13]. PET response criteria were grouped into three categories: Deauville score (DS) on a 5-point scale [9, 13], International Harmonization Project (IHP) [12], and custom visual criteria (i.e. not based on consensus guidelines).
Outcome measures
The primary outcome measure was defined as PFS (preferably) or EFS at 2 years. We included studies with a minimum median follow-up period of 24 months in surviving patients (or for the entire study population), because most patients experience relapse or progression of their disease in the first 2 years after their diagnosis [24, 25].
Data extraction and quality assessment
After removing duplicates, two authors independently screened titles and abstracts of the search results for eligibility (CNB and NH, AdJ, or HCWdV). The decision to include studies in the review was based on the full-text articles (CNB and AdJ or HCWdV). Extensive data extraction forms (available upon request) were developed which included the criteria from the methodological checklists for diagnostic accuracy studies (QUADAS-2) [26] and for prognostic studies (QUIPS) [27]. The forms were tested in a few articles and used independently by two review authors (CNB, AdJ). Consensus meetings (with three experts in nuclear medicine, hematology, and methodology, respectively) were organized to solve disagreements and to decide on eligibility of the final study selection. Besides general information about study design, patients, treatment, interim 18F-FDG PET performance, and outcome measures (used for qualitative study descriptions and determination of eligibility) we extracted outcomes on two types of predictive parameters.
For the first predictive meta-analysis we extracted univariate hazard ratios (HRs) and their corresponding 95% confidence intervals. If this data was not reported and not provided after contacting the authors, we used the methods of Tierney et al. [28] to deduce these from reported parameters or from the Kaplan-Meier (KM) curves, using numbers at risk when available.
For the second predictive meta-analysis we used a diagnostic approach and constructed 2 × 2 contingency tables to calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of interim 18F-FDG PET for prediction of two-year PFS and - EFS. If no two-year survival percentages were reported we estimated the percentages from the KM curves at this time-point. If information was missing or unclear authors were contacted. A maximum of three reminders were sent. In case of no reply we used the information that was available from the original publication. Individual patient data was not requested for this meta-analysis.
Statistical analyses
Two approaches of meta-analysis
For the meta-analyses of the HRs, individual log hazard ratios (HRs) and standard errors (SE) were pooled using a random-effects model (REML, restricted maximum likelihood). Together with the individual study results, the pooled effect estimate—expressed as HR and 95% confidence interval—was visualized in a Forest plot. Between-study heterogeneity was assessed by using Cochran’s Q and I2 statistics [29]. A 95% prediction interval around the HR was calculated to predict the expected range of the HR of a new (future) study [30]. A funnel plot was presented to visually assess if publication bias was likely [31].
For the diagnostic meta-analysis, the pooled sensitivity and specificity was obtained by Hierarchical Summary ROC curve (HSROC) models and ROC curves constructed in RevMan [32] using the input parameters of the HSROC models.
Influence of covariates
Several prespecified subgroup analyses—which included both clinical and methodological issues—were performed using univariate meta-regression models for the HRs and as covariate interaction term in the HSROC models. The following subgroup analyses were performed: study design (retrospective or prospective studies; blinded review or not reported; PFS or EFS), characteristics of patients (100% DLBCL or between 80 and 100%), treatments (ASCT upfront or not, preplanned or consolidative radiotherapy used or unknown), properties of scans (PET/CT or a combination of PET/CT and PET standalone systems, availability of a baseline PET or CT), and scoring issues (DS -, IHP -, or custom criteria, central review or local review).
Software
Statistical analysis was performed in R (version 3.2.5) [33] using the Metafor package and SAS Proc Nlmixed was used for the HSROC models. A P value of less than 0.05 was considered statistically significant.
Results
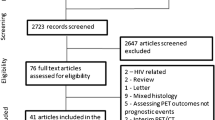
The search yielded 9,960 records after removing duplicates; 290 concerned studies on NHL and interim FDG-PET, the other 9,670 records were excluded because they did not report on NHL or I-PET. 85/290 were potentially eligible and full-text articles were retrieved. After checking detailed inclusion and exclusion criteria we included 20 eligible studies in the qualitative systematic review; 19 out of 20 were eligible for the HRs evaluations and 18 out of 20 for the HSROC analyses (Fig. 1).
PRISMA flow diagram. *Records refer to the title and abstract screening of the search results. †Full-text articles refer to the full-text assessment of the selected articles from the title and abstract screening phase. Abbreviations: I-PET = interim 18F-FDG positron emission tomography, FLT = Fluorothymidine, DLBCL = diffuse large B-cell lymphoma, EoT-PET = end-of-treatment 18F-FDG positron emission tomography, HR = hazard ratio, HSROC = hierarchical summary receiver operating curve
A total of 2,411 newly diagnosed DLBCL patients from 20 studies were assessed for this analysis. Table 1 shows the main study-, patient-, and treatment characteristics of the included studies. The number of included patients per study ranged from 32 to 327 (median 112, interquartile range 70–142). Seven studies had a prospective study design. The median age of the patients ranged from 54 to 65 years, with the exception of one study with a median age of 46 [40], and 45–67% of the patients were of male gender. Most studies included patients with Ann Arbor stage I/II as well as stage III/IV; in two studies less than 50% of the patients had stage III or IV [37, 45] and one study included patients with stage III and IV only [51]. First-line treatment regimens varied between and within the studies, but R-CHOP was the basic principle in all studies. Radiotherapy was given in most of the studies to selected patients (preplanned, e.g. in case of bulky disease or as a consolidation for residual lymphoma sites after treatment). Autologous stem cell transplantation had been planned upfront in three studies [44, 48, 50].
In Table 2 details of PET procedures, interpretation, and timing of interim PET between cycles are shown. Most studies performed an interim PET scan after two cycles of chemotherapy in all patients, one study made interim PET scans after only one course in all patients [43]; the remaining studies combined patient groups who had their interim assessment after a variable number of treatment cycles. The number of days after the previous treatment course at which the interim PET was acquired also varied between studies, mostly just before the next chemotherapy cycle, but the number of days after previous treatment was not reported by all studies. Twelve studies applied the Deauville scoring system and four the International Harmonization Project system [40, 46, 48, 51]. The remaining studies used a custom scoring system [42, 50, 52, 53].
The outcome measures of the included studies are shown in Table 3: 16 studies presented PFS and the other four studies reported EFS. The definitions of PFS and EFS for the different studies are presented in Supplemental Table 2. Percentages of positive interim PET scans ranged from 18.1 to 56.3%. Five original publications had reported univariate HRs, and four authors provided a (re)calculated HR upon our request. Two authors provided information about the number of events and P-values in order to use the method from Tierney et al. [28]. For one study we extracted the HR from the KM curves with numbers at risk provided by the authors and for six studies we used the KM curves without numbers at risk. For two studies we could not extract the HRs, as there was insufficient data and no Kaplan-Meier curve [36, 48].
In Fig. 2 the Forest plot with the 18 univariate HRs is shown. The pooled effect estimate was 3.13 (95% CI 2.52–3.89). The Cochran’s Q test for heterogeneity was not statistically significant (P = 0.087) and between study heterogeneity was low (I2 = 35.14%). The 95% prediction interval was 1.68–5.83, with one outlier [37].
Forest plot of univariate hazard ratios for interim PET scans in diffuse large B-cell lymphoma. This plot shows the univariate hazard ratios (black squares, size based on study size), and 95% CI’s (horizontal lines) of the individual studies sorted by publication year for PFS/EFS of the interim PET positive and negative patients. The estimated pooled effect estimation is shown with a diamond. For each study a 2 × 2 contingency table at 2 years follow-up is shown
The methodological quality was assessed based on the QUADAS-2 and QUIPS checklists. Subgroup analyses were performed on study design characteristics that were potential sources of bias.
Meta-regression showed that the outcomes did not differ between retrospective and prospective studies, studies with blinded review and studies that did not report whether they blinded the PET/CT assessment, or studies that used PFS or EFS as outcome measure. A statistically significant higher HR was found for studies with a combination of integrated PET/CT- and PET standalone systems compared to studies with integrated PET/CT systems only (HR 4.39 vs 2.85, P = 0.0332) and a trend towards a higher HR in studies with 80–99% DLBCL compared to studies with 100% DLBCL (P = 0.0577). Prespecified subgroups for different types of treatments and FDG-PET scoring systems showed no statistically significant differences (Supplemental Table 3). For the subgroups “availability of baseline PET or CT” and “central or local review procedure”, insufficient information was reported to perform these analyses. Risk of publication bias as assessed with a Funnel plot was low (Supplemental Fig. 1).
Nineteen studies had data available for the calculation of PPV, NPV, sensitivity, and specificity of interim PET for prediction of two-year-PFS or -EFS. For one study we could not extract or calculate the diagnostic measures [48]. PPV and NPV ranged from 20 to 74% and 64 to 95%, respectively. Sensitivity and specificity ranged from 33 to 87% and 49 to 94%, respectively (Table 3, Supplemental Fig. 2).
In Fig. 3 the ROC curves of the different visual criteria are shown. The studies that were classified as “custom”, did not have comparable scan positivity definitions and therefore no summary curve for this group was presented. We found no statistically significant differences between the curves for Deauville and IHP. There was a trend (P = 0.0503) towards a higher accuracy for studies with DLBCL 80–99% versus studies with 100% DLBCL patients.
Summary receiver operating curves (sROC) for different visual interim PET criteria. Studies that assessed interim PET scans according to the Deauville’s criteria are indicated with blue circles, studies that used the international harmonization project (IHP) criteria are indicated with red diamonds and studies that used custom visual criteria are indicated with green squares. The size of the circles, diamonds, and squares are based on the inverse standard error
Discussion
This systematic review and meta-analysis included 20 studies comprising a total of 2,411 DLBCL patients who underwent interim 18F-FDG PET. Eighteen studies were eligible for the HR and 19 for the HSROC meta-analyses. We found a pooled estimated HR of 3.13 (95% CI 2.52–3.89) for interim PET in the prediction of PFS or EFS. The prediction interval ranged from 1.68 to 5.83, suggesting that a new study investigating the prognostic value of interim PET on PFS or EFS will find a HR in this range with 95% confidence. These results confirm the predictive value of interim PET in DLBCL patients for PFS and EFS. Our pooled estimated HR was lower than reported in a previous meta-analysis (2013) [16] which reported a pooled estimated HR of 4.4 (95% CI 3.34–5.81) from nine studies investigating the prediction of PFS by interim PET. They used a similar approach to extract HRs; however, they had less strict inclusion criteria with regard to the NHL types and follow-up period, both visual and semi-quantitatively assessed PET scans were included, and no subgroup analyses were performed. Despite these differences, their HR result is within the range of our calculated 95% prediction interval and the amount of statistical heterogeneity (I2 = 39%) amongst studies was comparable. Other meta-analyses did not compare the HRs between studies [15, 17, 18].
We have no explanation for the statistically significant higher HR for studies (n = 5) that used both PET/CT- and PET standalone systems compared to studies that used an integrated PET/CT system.
The trend towards a higher HR for the studies with both DLBCL and PMBCL patients compared to studies with only DLBCL patients could not directly be explained by the inclusion of both lymphoma subtypes. The fact that two out of three studies with both DLBCL and PMBCL patients [52, 53] used custom criteria for the interpretation of the interim PET could possibly explain this. These meta-regression results should be interpreted with caution, as the number of studies per subgroup were relatively low (Supplemental Table 3) which precludes multivariate meta-regression analysis.
Diagnostic 2 × 2 contingency tables of interim PET showed wide ranges between studies for sensitivity, specificity, and positive predictive values at 2 years. The ranges reported in other systematic reviews and meta-analyses were hard to compare as they used the complete follow-up period for their calculations, included studies with follow-up periods less than 24 months, and used other statistical methods [15, 17, 18]. We decided to truncate at 2 years, as most clinically relevant events occur during this period. Moreover, the widely ranging complete follow-up periods of individual studies might introduce bias.
Negative predictive values for 2-year progression-free status were generally above 80%, except in four studies [34, 35, 39, 53]. In Mamot et al. [39], the somewhat lower negative predictive value could possibly be explained because radiotherapy (administered regardless of PET results) was counted as an event and resulted in a lower EFS rate compared to other clinical trials. Zhao et al. [53] had a low percentage of negative interim PET scans and a high number of events, which explains the lower NPV.
The higher sensitivity values seen in ROC analysis for both IHP and custom criteria vs. the Deauville system may be explained by the lower threshold of test positivity with IHP vs. Deauville (using liver and blood pool activity as the reference tissue, respectively). None of the studies using custom criteria defined a threshold comparable to or higher than hepatic uptake. We found widely ranging positivity rates between studies, which are mainly in agreement with the timing of interim PET between cycles and the criteria used. In an exploratory analysis on five studies [34, 37,38,39, 47] that performed interim PET strictly after 2 cycles of therapy and applied the Deauville scoring system we found a pooled estimated HR of 3.48 (95% CI 2.46–4.93) with a corresponding 95% prediction interval of 1.58–7.67 (Supplemental Fig. 3). The positivity rates for these studies ranged between 18 and 46%, PPV from 37 to 74% and NPV from 76 to 91%, comparable to the analysis including all studies.
We chose to present the methodological characteristics along the other characteristics of the study population and treatments (Table 1) and along characteristics (including timing between cycles) of the index test (Table 2).
QUADAS-2 and QUIPS criteria were applied to assess the quality of the studies from the perspective of risk of bias and applicability. In this review, the strict inclusion and exclusion criteria with regard to patient population (>80% DLBCL), index test (interim PET between one and five treatment cycles), and reference standard (PFS and EFS) guaranteed the applicability of the results to the review question. In the subgroup analyses we examined whether bias could have occurred because of methodological shortcomings. It appeared that none of these affected the results. Only characteristics of the population (< 100% DLBCL) and a combination of integrated and standalone systems seemed to have impact on the predictive value of interim PET.
We used a comprehensive search strategy and applied strict inclusion and exclusion criteria. We focused on DLBCL patients, and 2-year PFS. Moreover, we examined the influence of different design characteristics (retrospective and prospective, blinded review or not reported; PFS or EFS), characteristics of patients (100% DLBCL or between 80 and 100%), treatments (ASCT upfront or not, preplanned or consolidative radiotherapy used or unknown), availability of a baseline PET or CT, properties of scans (PET/CT or a combination of PET/CT and PET standalone systems), and scoring issues (DS -, IHP -, or custom criteria, central review or local review). Only the patient characteristics and properties of scans affected the results. It appeared that the HR estimates of the included studies were quite homogeneous (I2 = 35%).
By contacting the authors we were able to include most of the eligible studies in our meta-analysis and deducting data that was not presented by the authors directly. Some data though were hard to obtain from the studies.
First of all, the definition of the start of the progression-free survival and event-free survival differed amongst studies. Some studies started their follow-up period at the time from diagnosis and others from initiation of first-line treatment. Recently some data has shown that patients who have a more aggressive disease tend to be treated earlier, so there could be selection bias between studies that have a shorter period between time of diagnosis and initiation of treatment versus studies with a longer period [54]. For future studies it seems important to have a comparable start of the follow-up period and authors should report the interval between diagnosis and start of the treatment to prevent or adjust for this risk of bias.
Another issue is that timing of the interim PET scans between cycles was different between studies; not only did the timing after which cycle the scan is performed differ, but also the number of days between the previous treatment course and interim PET. Unfortunately, not all authors report on this, although it is recommended to perform the scan at least 10 days after the previous course of chemotherapy, because of possible effects on tumor metabolism and systemic effects by, for example, growth factors [55].
In systematic reviews, investigators need to make choices. We chose to use the univariate data. This choice was made because univariate data were available in most studies and because of the large heterogeneity in factors for which the HR was adjusted in the primary articles. The adjusted factors were limited by the low number of events in most studies and partially based on available information such as quantitative PET analyses, immunohistochemistry and collection of specific clinical data (e.g. bone marrow involvement). Fourteen of the 20 studies performed a multivariate analysis. Most articles adjusted for the IPI score [34,35,36,37,38,39, 41,42,43, 46] or age-adjusted IPI [44, 48, 49], some dichotomized the score and others used the individual components. Results were varying widely; in some studies both interim PET and (aa)IPI showed an independent association with PFS or EFS [42, 48], others only for interim PET [34, 37, 39, 41, 44, 53], or (aa)IPI [43, 49] or no independent associations were found for both interim PET or (aa)IPI [35, 36, 38, 46]. One could argue that reporting univariate HRs instead of multivariate HRs could result in an overestimation of the predictive value of interim PET. Three studies reported both uni- and multivariate HRs and differences between univariate and multivariate HRs were −0.99 [41], 0.0 [39],and + 0.2 [42], respectively.
We further decided to choose the DS threshold for the interim response criteria which is most commonly described (DS < = 3 versus DS > = 4), because presenting all thresholds would increase heterogeneity, influence effect sizes, and finally use the same patients data multiple times in the analyses. Four studies presented multiple scores. Mylam et al. [43] published data about positivity for Deauville scores 4 and 5 as well as for Deauville score 5 and for IHP. Kim et al. [35] and Itti et al. [47] presented data about different positivity cutoff values for Deauville scores. Fuertes et al. [45] published a regular Deauville score as well as a 3 point-scale. In this review, we focused on visual response assessment criteria, and the potential added value of quantitative PET metrics is currently being investigated. Recently, a large phase III PET-adapted trial showed in a post-hoc analysis that a SUVmax reduction strategy [56] seems to discriminate better between good and poor outcome compared to the Deauville scoring system [57]. Finally, it should be mentioned that the studies from Safar et al. [50] and Itti et al. [47] had a small overlap in patient inclusion (n = 7); however, this will presumably not bias our results due to the small number.
Conclusion
This systematic review and meta-analysis shows that interim PET in DLBCL patients has predictive value (HR 3.13). However, some diagnostic test characteristics are still too low, especially the positive predictive value should be improved, before a risk stratified treatment approach can be implemented in clinical practice.
References
Pfreundschuh M, Trümper L, Osterborg A, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera international trial (MInT) group. Lancet Oncol. 2006;7:379–91.
Pfreundschuh M, Schubert J, Ziepert M, et al. Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B-cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol. 2008;9:105–16.
Vitolo U, Trněný M, Belada D, et al. Obinutuzumab or rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in previously untreated diffuse large B-cell lymphoma. J Clin Oncol. 2017;35:3529–37.
International Non-Hodgkin's Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med. 1993;329:987–94.
Ziepert M, Hasenclever D, Kuhnt E, et al. Standard international prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28:2373–80. Erratum in: J Clin Oncol. 2011; 29: 779
Sehn LH, Berry B, Chhanabhai M, et al. The revised international prognostic index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109:1857–61.
Zhou Z, Sehn LH, Rademaker AW, et al. An enhanced international prognostic index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123:837–42.
Stiff PJ, Unger JM, Cook JR, et al. Autologous transplantation as consolidation for aggressive non-Hodgkin's lymphoma. N Engl J Med. 2013;369:1681–90.
Barrington SF, Mikhaeel NG, Kostakoglu L, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the international conference on malignant lymphomas imaging working group. J Clin Oncol. 2014;32:3048–58. Erratum in: J Clin Oncol. 2016; 34: 2562
Young H, Baum R, Cremerius U, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET study group. Eur J Cancer. 1999;35:1773–82.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122S–50S.
Juweid ME, Stroobants S, Hoekstra OS, et al. Imaging Subcommittee of International Harmonization Project in lymphoma. Use of positron emission tomography for response assessment of lymphoma: consensus of the imaging Subcommittee of International Harmonization Project in lymphoma. J Clin Oncol. 2007;25:571–8.
Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32:3059–68.
André MPE, Girinsky T, Federico M, et al. Early positron emission tomography response-adapted treatment in stage I and II Hodgkin lymphoma: final results of the randomized EORTC/LYSA/FIL H10 trial. J Clin Oncol. 2017;35:1786–94.
Terasawa T, Lau J, Bardet S, et al. Fluorine-18-fluorodeoxyglucose positron emission tomography for interim response assessment of advanced-stage Hodgkin's lymphoma and diffuse large B-cell lymphoma: a systematic review. J Clin Oncol. 2009;27:1906–14.
Zhu Y, Lu J, Wei X, Song S, Huang G. The predictive value of interim and final [18F] fluorodeoxyglucose positron emission tomography after rituximab-chemotherapy in the treatment of non-Hodgkin's lymphoma: a meta-analysis. Biomed Res Int. 2013;275805 https://doi.org/10.1155/2013/275805.
Sun N, Zhao J, Qiao W, Wang T. Predictive value of interim PET/CT in DLBCL treated with R-CHOP: meta-analysis. Biomed Res Int. 2015;648572 https://doi.org/10.1155/2015/648572.
Adams HJ, Kwee TC. Prognostic value of interim FDG-PET in R-CHOP-treated diffuse large B-cell lymphoma: systematic review and meta-analysis. Crit Rev Oncol Hematol. 2016;106:55–63.
Maurer MJ, Ghesquières H, Jais JP, et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J Clin Oncol. 2014;32:1066–73.
Zimmermann M, Oehler C, Mey U, Ghadjar P, Zwahlen DR. Radiotherapy for non-Hodgkin's lymphoma: still standard practice and not an outdated treatment option. Radiat Oncol. 2016;11:110. https://doi.org/10.1186/s13014-016-0690-y.
Delarue R, Tilly H, Mounier N, et al. Dose-dense rituximab-CHOP compared with standard rituximab-CHOP in elderly patients with diffuse large B-cell lymphoma (the LNH03-6B study): a randomised phase 3 trial. Lancet Oncol. 2013;14:525–33.
Cunningham D, Hawkes EA, Jack A, et al. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet. 2013;381:1817–26.
Casasnovas RO, Ysebaert L, Thieblemont C, et al. FDG-PET-driven consolidation strategy in diffuse large B-cell lymphoma: final results of a randomized phase 2 study. Blood. 2017;130:1315–26.
Coiffier B, Thieblemont C, Van Den Neste E, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d'Etudes des Lymphomes de l'Adulte. Blood. 2010;116:2040–5.
Gisselbrecht C, Glass B, Mounier N, et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28:4184–90. Erratum in: J Clin Oncol. 2012; 30: 1896
Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158:280–6.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. https://doi.org/10.1136/bmj.d549.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
R Core Team (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org.
Fan Y, Zhang Y, Yang Z, et al. Evaluating early interim fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography with the SUV(max-liver)-based interpretation for predicting the outcome in diffuse large B-cell lymphoma. Leuk Lymphoma. 2017;58:1–9.
Kim J, Song YS, Lee JS, Lee WW, Kim SE. Risk stratification of diffuse large B-cell lymphoma with interim PET-CT based on different cutoff Deauville scores. Leuk Lymphoma. 2018;59:340–7.
de Oliveira Costa R, Hallack Neto A, Siqueira S, et al. Interim fluorine-18 fluorodeoxyglucose PET-computed tomography and cell of origin by immunohistochemistry predicts progression-free and overall survival in diffuse large B-cell lymphoma patients in the rituximab era. Nucl Med Commun. 2016;37:1095–101.
Kong Y, Qu L, Li Y, Liu D, Lv X, Han J. Predictive significance of a new prognostic score for patients with diffuse large B-cell lymphoma in the interim-positron emission tomography findings. Medicine (Baltimore). 2016;95:e2808. https://doi.org/10.1097/MD.0000000000002808.
Mikhaeel NG, Smith D, Dunn JT, et al. Combination of baseline metabolic tumour volume and early response on PET/CT improves progression-free survival prediction in DLBCL. Eur J Nucl Med Mol Imaging. 2016;43:1209–19.
Mamot C, Klingbiel D, Hitz F, et al. Final results of a prospective evaluation of the predictive value of interim positron emission tomography in patients with diffuse large B-cell lymphoma treated with R-CHOP-14 (SAKK 38/07). J Clin Oncol. 2015;33:2523–9. Erratum in: J Clin Oncol. 2015; 33: 3074
Zhang X, Fan W, Xia ZJ, et al. Use of subsequent PET/CT in diffuse large B-cell lymphoma patients in complete remission following primary therapy. Chin J Cancer. 2015;34:70–8.
Carr R, Fanti S, Paez D, et al. IAEA lymphoma study group. Prospective international cohort study demonstrates inability of interim PET to predict treatment failure in diffuse large B-cell lymphoma. J Nucl Med. 2014;55:1936–44.
Dabaja BS, Hess K, Shihadeh F, et al. Positron emission tomography/computed tomography findings during therapy predict outcome in patients with diffuse large B-cell lymphoma treated with chemotherapy alone but not in those who receive consolidation radiation. Int J Radiat Oncol Biol Phys. 2014;89:384–91.
Mylam KJ, Kostakoglu L, Hutchings M, et al. (18)F-fluorodeoxyglucose-positron emission tomography/computed tomography after one cycle of chemotherapy in patients with diffuse large B-cell lymphoma: results of a Nordic/US intergroup study. Leuk Lymphoma. 2015;56:2005–12.
Nols N, Mounier N, Bouazza S, et al. Quantitative and qualitative analysis of metabolic response at interim positron emission tomography scan combined with international prognostic index is highly predictive of outcome in diffuse large B-cell lymphoma. Leuk Lymphoma. 2014;55:773–80.
Fuertes S, Setoain X, Lopez-Guillermo A, et al. Interim FDG PET/CT as a prognostic factor in diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2013;40:496–504.
González-Barca E, Canales M, Cortés M, et al. GELTAMO (Grupo Español de Linfoma y Trasplante de Médula Ósea). Predictive value of interim 18F-FDG-PET/CT for event-free survival in patients with diffuse large B-cell lymphoma homogenously treated in a phase II trial with six cycles of R-CHOP-14 plus pegfilgrastim as first-line treatment. Nucl Med Commun. 2013;34:946–52.
Itti E, Meignan M, Berriolo-Riedinger A, et al. An international confirmatory study of the prognostic value of early PET/CT in diffuse large B-cell lymphoma: comparison between Deauville criteria and ΔSUVmax. Eur J Nucl Med Mol Imaging. 2013;40:1312–20.
Lanic H, Mareschal S, Mechken F, et al. Interim positron emission tomography scan associated with international prognostic index and germinal center B cell-like signature as prognostic index in diffuse large B-cell lymphoma. Leuk Lymphoma. 2012;53:34–42.
Pregno P, Chiappella A, Bellò M, et al. Interim 18-FDG-PET/CT failed to predict the outcome in diffuse large B-cell lymphoma patients treated at the diagnosis with rituximab-CHOP. Blood. 2012;119:2066–73.
Safar V, Dupuis J, Itti E, et al. Interim [18F]fluorodeoxyglucose positron emission tomography scan in diffuse large B-cell lymphoma treated with anthracycline-based chemotherapy plus rituximab. J Clin Oncol. 2012;30:184–90.
Cashen AF, Dehdashti F, Luo J, Homb A, Siegel BA, Bartlett NL. 18F-FDG PET/CT for early response assessment in diffuse large B-cell lymphoma: poor predictive value of international harmonization project interpretation. J Nucl Med. 2011;52:386–92.
Zinzani PL, Gandolfi L, Broccoli A, et al. Midtreatment 18F-fluorodeoxyglucose positron-emission tomography in aggressive non-Hodgkin lymphoma. Cancer. 2011;117:1010–8.
Zhao J, Qiao W, Wang C, Wang T, Xing Y. Therapeutic evaluation and prognostic value of interim hybrid PET/CT with (18)F-FDG after three to four cycles of chemotherapy in non-Hodgkin's lymphoma. Hematology. 2007;12:423–30.
Maurer MJ, Ghesquières H, Link BK, et al. Diagnosis-to-Treatment Interval Is an Important Clinical Factor in Newly Diagnosed Diffuse Large B-Cell Lymphoma and Has Implication for Bias in Clinical Trials. J Clin Oncol. 2018;36:1603–10.
Boellaard R, Delgado-Bolton R, Oyen WJ, et al. European Association of Nuclear Medicine (EANM). FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Lin C, Itti E, Haioun C, et al. Early 18F-FDG PET for prediction of prognosis in patients with diffuse large B-cell lymphoma: SUV-based assessment versus visual analysis. J Nucl Med. 2007;48:1626–32.
Dührsen U, Müller S, Hertenstein B, et al. PETAL Trial Investigators. Positron Emission Tomography-Guided Therapy of Aggressive Non-Hodgkin Lymphomas (PETAL): a multicenter, randomized phase III trial. J Clin Oncol. 2018, May 11. https://doi.org/10.1200/JCO.2017.76.8093.
Acknowledgements
This work was financially supported by an Alpe d’Huzes/KWF fund provided by the Dutch Cancer Society (# VU 2012-5848).
The authors would like to thank the authors of the primary studies that replied to the requests and kindly provided additional information or analyses.
Funding
This work was financially supported by an Alpe d’Huzes/KWF fund provided by the Dutch Cancer Society (# VU 2012–5848).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Burggraaff, C.N., de Jong, A., Hoekstra, O.S. et al. Predictive value of interim positron emission tomography in diffuse large B-cell lymphoma: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 46, 65–79 (2019). https://doi.org/10.1007/s00259-018-4103-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4103-3