Abstract
Purpose
Although the mechanisms by which the central noradrenaline (NA) system influences appetite and controls energy balance are quite well understood, its relationship to changes in body weight remains largely unknown. The main goal of this study was to further clarify whether the brain NA system is a stable trait or whether it can be altered by dietary intervention.
Methods
We aimed to compare central NA transporter (NAT) availability in ten obese, otherwise healthy individuals with a body mass index (BMI) of 42.4 ± 3.7 kg/m2 (age 34 ± 9 years, four women) and ten matched non-obese, healthy controls (BMI 23.9 ± 2.5 kg/m2, age 33 ± 10 years, four women) who underwent PET with the NAT-selective radiotracer (S,S)-[11C]O-methylreboxetine (MRB) before and 6 months after dietary intervention.
Results
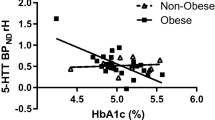
MRI-based individual volume-of-interest analyses revealed an increase in binding potential (BPND) in the insula and the hippocampus of obese individuals, which correlated well with changes in BMI (−3.3 ± 5.3%; p = 0.03) following completion of the dietary intervention. Furthermore, voxel-wise regression analyses showed that lower BPND in these regions, but also in the midbrain and the prefrontal cortex, at baseline was associated with higher achieved weight loss (e.g., hippocampal area R2 = 0.80; p < 0.0001). No changes were observed in non-obese controls.
Conclusion
These first longitudinal interventional data on NAT availability in highly obese individuals indicate that the central NA system is modifiable. Our findings suggest that NAT availability before intervention could help predict the amount and success of weight loss in obese individuals and help adjust treatment options individually by allowing prediction of the benefit of a dietary intervention.


Similar content being viewed by others
References
Finkelstein EA, Linnan LA, Tate DF, Leese PJ. A longitudinal study on the relationship between weight loss, medical expenditures, and absenteeism among overweight employees in the WAY to Health study. J Occup Environ Med. 2009;51:1367–73. https://doi.org/10.1097/JOM.0b013e3181c2bb56.
Haslam DW, James WP. Obesity. Lancet. 2005;366:1197–209. https://doi.org/10.1016/s0140-6736(05)67483-1.
Malnick SD, Knobler H. The medical complications of obesity. QJM. 2006;99:565–79. https://doi.org/10.1093/qjmed/hcl085.
Thorpe KE, Philyaw M. The medicalization of chronic disease and costs. Annu Rev Public Health. 2012;33:409–23. https://doi.org/10.1146/annurev-publhealth-031811-124652.
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9. https://doi.org/10.1016/s0140-6736(05)67663-5.
le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–5. https://doi.org/10.1097/SLA.0b013e3180caa3e3.
Corwin RL, Wojnicki FH, Zimmer DJ, Babbs RK, McGrath LE, Olivos DR, et al. Binge-type eating disrupts dopaminergic and GABAergic signaling in the prefrontal cortex and ventral tegmental area. Obesity (Silver Spring). 2016;24:2118–25. https://doi.org/10.1002/oby.21626.
Morales I, Font L, Currie PJ, Pastor R. Involvement of opioid signaling in food preference and motivation: studies in laboratory animals. Prog Brain Res. 2016;229:159–87. https://doi.org/10.1016/bs.pbr.2016.06.002.
Hesse S, Rullmann M, Luthardt J, Winter K, Hankir MK, Becker GA, et al. Central serotonin transporter availability in highly obese individuals compared with non-obese controls: A [(11)C] DASB positron emission tomography study. Eur J Nucl Med Mol Imaging. 2016;43:1096–104. https://doi.org/10.1007/s00259-015-3243-y.
Huang XF, Zavitsanou K, Huang X, Yu Y, Wang H, Chen F, et al. Dopamine transporter and D2 receptor binding densities in mice prone or resistant to chronic high fat diet-induced obesity. Behav Brain Res. 2006;175:415–9. https://doi.org/10.1016/j.bbr.2006.08.034.
Haahr ME, Hansen DL, Fisher PM, Svarer C, Stenbaek DS, Madsen K, et al. Central 5-HT neurotransmission modulates weight loss following gastric bypass surgery in obese individuals. J Neurosci. 2015;35:5884–9. https://doi.org/10.1523/jneurosci.3348-14.2015.
Bello NT, Walters AL, Verpeut JL, Cunha PP. High-fat diet-induced alterations in the feeding suppression of low-dose nisoxetine, a selective norepinephrine reuptake inhibitor. J Obes. 2013;2013:457047. https://doi.org/10.1155/2013/457047.
Hainer V, Kabrnova K, Aldhoon B, Kunesova M, Wagenknecht M. Serotonin and norepinephrine reuptake inhibition and eating behavior. Ann N Y Acad Sci. 2006;1083:252–69. https://doi.org/10.1196/annals.1367.017.
Gallagher JJ, Zhang X, Hall FS, Uhl GR, Bearer EL, Jacobs RE. Altered reward circuitry in the norepinephrine transporter knockout mouse. PLoS One. 2013;8:e57597. https://doi.org/10.1371/journal.pone.0057597.
Sofuoglu M, Sewell RA. Norepinephrine and stimulant addiction. Addict Biol. 2009;14:119–29. https://doi.org/10.1111/j.1369-1600.2008.00138.x.
Li CS, Potenza MN, Lee DE, Planeta B, Gallezot JD, Labaree D, et al. Decreased norepinephrine transporter availability in obesity: positron emission tomography imaging with (S,S)-[(11)C]O-methylreboxetine. Neuroimage. 2014;86:306–10. https://doi.org/10.1016/j.neuroimage.2013.10.004.
Melasch J, Rullmann M, Hilbert A, Luthardt J, Becker GA, Patt M, et al. The central nervous norepinephrine network links a diminished sense of emotional well-being to an increased body weight. Int J Obes (Lond). 2016;40:779–87. https://doi.org/10.1038/ijo.2015.216.
Hesse S, Becker GA, Rullmann M, Bresch A, Luthardt J, Hankir MK, et al. Central noradrenaline transporter availability in highly obese, non-depressed individuals. Eur J Nucl Med Mol Imaging. 2017;44:1056–64. https://doi.org/10.1007/s00259-016-3590-3.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–74.
Van Strien T, Rookus MA, Bergers GP, Frijters JE, Defares PB. Life events, emotional eating and change in body mass index. Int J Obes. 1986;10:29–35.
Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, et al. Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite. 2008;51:148–55. https://doi.org/10.1016/j.appet.2008.01.001.
Mitchell JE, Mussell MP, Peterson CB, Crow S, Wonderlich SA, Crosby RD, et al. Hedonics of binge eating in women with bulimia nervosa and binge eating disorder. Int J Eating Disord. 1999;26:165–70.
Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Add Behav. 2016;30:113–21. https://doi.org/10.1037/adb0000136.
Rothbart MK, Ahadi SA, Evans DE. Temperament and personality: origins and outcomes. J Pers Soc Psychol. 2000;78:122–35.
Ichise M, Liow JS, Lu JQ, Takano A, Model K, Toyama H, et al. Linearized reference tissue parametric imaging methods: application to [11C]DASB positron emission tomography studies of the serotonin transporter in human brain. J Cereb Blood Flow Metab. 2003;23:1096–112. https://doi.org/10.1097/01.wcb.0000085441.37552.ca.
Hannestad J, Gallezot JD, Planeta-Wilson B, Lin SF, Williams WA, van Dyck CH, et al. Clinically relevant doses of methylphenidate significantly occupy norepinephrine transporters in humans in vivo. Biol Psychiatry. 2010;68:854–60. https://doi.org/10.1016/j.biopsych.2010.06.017.
Dagher A. Functional brain imaging of appetite. Trends Endocrinol Metab. 2012;23:250–60. https://doi.org/10.1016/j.tem.2012.02.009.
Kenny PJ. Common cellular and molecular mechanisms in obesity and drug addiction. Nat Rev Neurosci. 2011;12:638–51. https://doi.org/10.1038/nrn3105.
Small DM, Zald DH, Jones-Gotman M, Zatorre RJ, Pardo JV, Frey S, et al. Human cortical gustatory areas: a review of functional neuroimaging data. Neuroreport. 1999;10:7–14.
Del Parigi A, Gautier JF, Chen K, Salbe AD, Ravussin E, Reiman E, et al. Neuroimaging and obesity: mapping the brain responses to hunger and satiation in humans using positron emission tomography. Ann N Y Acad Sci. 2002;967:389–97.
Kringelbach ML, O'Doherty J, Rolls ET, Andrews C. Activation of the human orbitofrontal cortex to a liquid food stimulus is correlated with its subjective pleasantness. Cereb Cortex. 2003;13:1064–71.
Small DM, Zatorre RJ, Dagher A, Evans AC, Jones-Gotman M. Changes in brain activity related to eating chocolate: from pleasure to aversion. Brain: J Neurol. 2001;124:1720–33.
Del Parigi A, Chen K, Salbe AD, Gautier JF, Ravussin E, Reiman EM, et al. Tasting a liquid meal after a prolonged fast is associated with preferential activation of the left hemisphere. Neuroreport. 2002;13:1141–5.
Squire LR, Ojemann JG, Miezin FM, Petersen SE, Videen TO, Raichle ME. Activation of the hippocampus in normal humans: a functional anatomical study of memory. Proc Natl Acad Sci U S A. 1992;89:1837–41.
Tracy J, Flanders A, Madi S, Laskas J, Stoddard E, Pyrros A, et al. Regional brain activation associated with different performance patterns during learning of a complex motor skill. Cereb Cortex. 2003;13:904–10.
Lathe R. Hormones and the hippocampus. J Endocrinol. 2001;169:205–31.
Bray N. Neural circuits: putting a stop to feeding. Nat Rev Neurosci. 2014;15:564. https://doi.org/10.1038/nrn3809.
Karlsson HK, Tuulari JJ, Tuominen L, Hirvonen J, Honka H, Parkkola R, et al. Weight loss after bariatric surgery normalizes brain opioid receptors in morbid obesity. Mol Psychiatry. 2016;21:1057–62. https://doi.org/10.1038/mp.2015.153.
Funding
This work was supported by the IFB Adiposity Diseases, Federal Ministry of Education and Research (BMBF), Germany; FKZ 01E01001 (http://www.bmbf.de).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board. The study was approved by the Bundesamt für Strahlenschutz (BfS, Federal Office for Radiation Protection; local EC number 206-10-08032010; EudraCT 2012-000568-32) and was performed in accordance with the ICH Guideline for Good Clinical Practice (GCP) and with the principles of the Declaration of Helsinki. The study was registered with the German Clinical Trials Register (DRKS).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This study was awarded the “Junge Wissenschaft im Focus” for young scientists at the 53rd Annual Meeting of the German Association of Nuclear Medicine (DGN).
Rights and permissions
About this article
Cite this article
Vettermann, F.J., Rullmann, M., Becker, G.A. et al. Noradrenaline transporter availability on [11C]MRB PET predicts weight loss success in highly obese adults. Eur J Nucl Med Mol Imaging 45, 1618–1625 (2018). https://doi.org/10.1007/s00259-018-4002-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4002-7