Abstract
Purpose
In the 2010 WHO classification, a Ki-67 proliferation index of 20% is the cut-off between intermediate-grade and high-grade gastroenteropancreatic neuroendocrine neoplasia (GEP-NEN). However, in clinical practice, tumours with a Ki-67 index of >15% are often considered high grade and treated with chemotherapy. In 40–70% of high-grade NENs, somatostatin receptors are overexpressed, enabling peptide receptor radionuclide therapy (PRRT) to be performed. We investigated the role of PRRT with 177Lu-DOTATATE in patients with GEP-NEN and a high Ki-67 proliferation index.
Methods
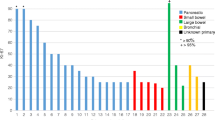
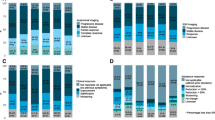
A total of 33 patients with advanced GEP-NENs, positive somatostatin receptor imaging (SRI+) and a Ki-67 proliferation index ranging from 15% to 70% were treated with Lu-PRRT. A cumulative activity of 18.5 GBq or 27.8 GBq of 177Lu-DOTATATE was administered in four or five cycles. Receiver operating characteristic (ROC) curve analysis was used to determine the best threshold of Ki-67 expression to predict disease progression.
Results
All patients completed the intended treatment. The median follow-up was 43 months (range 3–69 months). Two patients (6%) achieved a partial response and 21 (64%) showed stable disease, giving a disease control rate (DCR) of 70%. The median progression-free survival (PFS) was 23 months (95% CI 14.9–31.0 months) and the median overall survival was 52.9 months (95% CI 17.1–68.9 months). ROC curve analysis at 23 months revealed that the best Ki-67 index cut-off was 35%. In 23 patients (70%) the Ki-67 index was ≤35% and in 10 patients (30%) the Ki-67 index was in the range 36–70%. The DCR in the former group was 87% and 30% in the latter. The median PFS was 26.3 months (95% CI 18.4–37.7 months) and 6.8 months (95% CI 2.1–27 months), respectively (p = 0.005).
Conclusions
Lu-PRRT showed antitumour activity in SRI+ GEP-NENs of intermediate and high-grade. DCR and PFS were significantly better in patients with a Ki-67 index of ≤35% than in those with a Ki-67 index of >35%. On the basis of these results, PRRT should be considered as a therapeutic option in patients with high-grade SRI+ GEP-NENs, in particular those with a Ki-67 proliferation index of ≤35%.



Similar content being viewed by others
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9:61–72.
Bosman FT, Carneiro F, Hruban RH, Theise ND. World Health Organization (WHO) classification of tumours of the digestive system. Lyon, France: IARC Press; 2012.
Vilar E, Salazar R, Pérez-García J, Cortes J, Oberg K, Tabernero J. Chemotherapy and role of the proliferation marker Ki-67 in digestive neuroendocrine tumors. Endocr Relat Cancer. 2007;14:221–32.
Binderup T, Knigge U, Loft A, Federspiel B, Kjaer A. 18F-fluorodeoxyglucose positron emission tomography predicts survival of patients with neuroendocrine tumors. Clin Cancer Res. 2010;16:978–85.
National Comprehensive Cancer Network (NCCN). Clinical Practice Guidelines in Oncology, Neuroendocrine Tumors, version 1.2015. 2015. Available at: https://www.nccn.org.
Iwasa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S, et al. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol. 2010;40:313–8.
Yamaguchi T, Machida N, Morizane C, Kasuga A, Takahashi H, Sudo K, et al. Multicenter retrospective analysis of systemic chemotherapy for advanced neuroendocrine carcinoma of the digestive system. Cancer Sci. 2014;105:1176–81.
Mitry E, Baudin E, Ducreux M, Sabourin JC, Rufié P, Aparicio T, et al. Treatment of poorly differentiated neuroendocrine tumours with etoposide and cisplatin. Br J Cancer. 1999;81:1351–5.
Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in anaplastic variance of these neoplasm. Cancer. 1991;68:227–32.
Fjallskog ML, Granberg DP, Welin SL, Eriksson C, Oberg KE, Janson ET, et al. Treatment with cisplatin and etoposide in patients with neuroendocrine tumors. Cancer. 2001;92:1101–7.
Basturk O, Yang Z, Tang LH, Hruban RH, Adsay V, McCall CM, et al. The high grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogeneous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol. 2015;39:683–90.
Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24:152–60.
Perren A, Couvelard A, Scoazec JY, Costa F, Borbath I, Delle Fave G, et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: pathology: diagnosis and prognostic stratification. Neuroendocrinology. 2017;105:196–200.
Vélayoudom-Céphise FL, Duvillard P, Foucan L, Hadoux J, Chougnet CN, Leboulleux S, et al. Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer. 2013;20:649–57.
Fjällskog ML, Ludvigsen E, Stridsberg M, Oberg K, Eriksson B, Janson ET. Expression of somatostatin receptor subtypes 1 to 5 in tumor tissue and intratumoral vessels in malignant endocrine pancreatic tumors. Med Oncol. 2003;20:59–67.
Lu ZH, Li J, Lu M, Zhang XT, Li J, Zhou J, et al. Feasibility and efficacy of combined cisplatin plus irinotecan chemotherapy for gastroenteropancreatic neuroendocrine carcinomas. Med Oncol. 2013;30:664.
Srirajaskanthan R, Watkins J, Marelli L, Khan K, Caplin ME. Expression of somatostatin and dopamine 2 receptors in neuroendocrine tumours and the potential role for new biotherapies. Neuroendocrinology. 2009;89:308–14.
Artale S, Giannetta L, Cerea G, Maggioni D, Pedrazzoli P, Schiavetto I, et al. Treatment of metastatic neuroendocrine carcinomas based on WHO classification. Anticancer Res. 2005;25:4463–9.
Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, et al. Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol. 2005;23:2754–62.
Kratochwil C, Stefanova M, Mavriopoulou E, Holland-Letz T, Dimitrakopoulou-Strauss A, Afshar-Oromieh A, et al. SUV of [68Ga]DOTATOC-PET/CT predicts response probability of PRRT in neuroendocrine tumors. Mol Imaging Biol. 2015;17:313–8.
Ambrosini V, Campana D, Polverari G, Peterle C, Diodato S, Ricci C, et al. Prognostic value of 68Ga-DOTANOC PET/CT SUVmax in patients with neuroendocrine tumors of the pancreas. J Nucl Med. 2015;56:1843–8.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177 Lu-DOTA 0,Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–30.
Sansovini M, Severi S, Ianniello A, Nicolini S, Fantini L, Mezzenga E, et al. Long-term follow-up and role of FDG-PET in advanced pancreatic neuroendocrine patients treated with 177Lu-DOTATATE. Eur J Nucl Med Mol Imaging. 2017;44:490–9.
Paganelli G, Sansovini M, Ambrosetti A, Severi S, Monti M, Scarpi ED, et al. 177 Lu-Dota-octreotate radionuclide therapy of advanced gastrointestinal neuroendocrine tumors: results from a phase II study. Eur J Nucl Med Mol Imaging. 2014;41:1845–51.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Breeman WA, de Blois E, Bakker WH. Radiolabeling DOTA peptides with 90Yand 177Lu to a high specific activity. In: Chinol M, Paganelli G, editors. Radionuclide peptide cancer therapy. New York: Taylor & Francis; 2006. p. 119–26.
Bongiovanni A, Recine F, Riva N, Foca F, Liverani C, Mercatali L, et al. Outcome analysis of first-line somatostatin analog treatment in metastatic pulmonary neuroendocrine tumors and prognostic significance of 18FDG-PET/CT. Clin Lung Cancer. 2017;18:415–20.
Severi S, Nanni O, Bodei L, Sansovini M, Ianniello A, Nicoletti S, et al. Role of 18FDG PET/CT in patients treated with 177Lu-DOTATATE for advanced differentiated neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2013;40:881–8.
Claringbold PG, Turner JH. Pancreatic neuroendocrine tumor control: durable objective response to combination 177Lu-octreotate-capecitabine-temozolomide radiopeptide chemotherapy. Neuroendocrinology. 2016;103:432–9.
Kashyap R, Hofman MS, Michael M, Kong G, Akhurst T, Eu P, et al. Favourable outcomes of (177)Lu-octreotate peptide receptor chemoradionuclide therapy in patients with FDG-avid neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2015;42:176–85.
Paganelli G, Sansovini M, Ianniello A, Bodei L, Nicolini S, Grassi I, et al. 177Lu dotatate peptide receptor radionuclide therapy in combination with metronomic capecitabine in GEP-NENs with high glucose metabolism. Preliminary data of the LUX prospective phase II study. Clin Transl Imaging. 2017;5(Suppl 1):S11. (PO180)
Acknowledgements
The authors thank Gráinne Tierney for editorial assistance. They also thank Monica Golinucci and the other members of the Nuclear Medicine and Radiometabolic Medicine Unit team for support and assistance.
Funding
This study was partially supported by AIRC (Associazione Italiana per la Ricerca sul Cancro; grant number: G10679).
Author information
Authors and Affiliations
Contributions
Study concept and design: Giovanni Paganelli, Severi Stefano.
Provision of study materials or patients: Silvia Nicolini, Stefano Severi, Annarita Ianniello, Maddalena Sansovini, Alberto Bongiovanni, Giovanni Paganelli.
Collection and assembly of data: July 2011 to April 2016.
Diagnostic and therapeutic imaging: Federica Matteucci and Alice Rossi.
Analysis and interpretation of data: Giovanni Paganelli, Emanuela Scarpi, Silvia Nicolini.
Drafting of the manuscript: Silvia Nicolini.
Critical revision of the manuscript for important intellectual content: Giovanni Paganelli.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
The protocol was approved by the Ethics Committee of Area Vasta Romagna and by the competent Italian regulatory authorities. The study was performed in accordance with the principles of Good Clinical Practice and the Declaration of Helsinki.
Informed consent
All patients gave their written informed consent.
Rights and permissions
About this article
Cite this article
Nicolini, S., Severi, S., Ianniello, A. et al. Investigation of receptor radionuclide therapy with 177Lu-DOTATATE in patients with GEP-NEN and a high Ki-67 proliferation index. Eur J Nucl Med Mol Imaging 45, 923–930 (2018). https://doi.org/10.1007/s00259-017-3925-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3925-8