Abstract
Objectives
To retrospectively evaluate the correlation between intradiscal gas and infection in patients percutaneously biopsied for suspected discitis-osteomyelitis.
Materials and methods
We retrospectively reviewed all CT-guided discitis-osteomyelitis biopsies performed between 2002 and 2022. Two independent trained musculoskeletal radiologists evaluated for presence of gas on CT and/or MRI within 1 week of the biopsy. Disagreements were resolved by a third musculoskeletal radiologist. CT was considered the gold standard for the detection of intradiscal gas. Pathology, microbiology, and imaging and clinical follow-up were used as the gold standard for presence of infection. Interrater agreement on CT and MRI, sensitivity, and positive predictive value were calculated, using the presence of gas as an indicator (test positive) for “no infection.”
Results
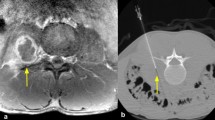
There were 284 biopsies in 275 subjects (mean age 58 ± 1.0 (range 4–99) years; 101 (37%) females and 174 (63%) males). Of the biopsies, 12 (4%) were cervical, 80 (28%) were thoracic, 192 (68%) were lumbar, and 200 (70%) were considered true discitis-osteomyelitis based on pathology, imaging, and clinical follow-up. Interrater agreement was excellent for CT (kappa = 0.83) and poor for MRI (kappa = − 0.021). The presence of gas had a 94% specificity and 76% negative predictive value for the absence of infection.
Conclusion
CT is the preferred method for detecting intradiscal gas. The presence of gas means that discitis-osteomyelitis is unlikely. If intradiscal gas is present in the setting of discitis-osteomyelitis, the gas bubbles tend to be smaller and fewer in number.


Similar content being viewed by others
References
Chang CY, Pelzl C, Jesse MK, Habibollahi S, Habib U, Gyftopoulos S. Image-guided biopsy in acute diskitis-osteomyelitis: a systematic review and meta-analysis. Am J Roentgenol. 2023;220:499–511.
Husseini JS, Habibollahi S, Nelson SB, Rosenthal DI, Chang CY. Best Practices: CT-guided percutaneous sampling of vertebral discitis-osteomyelitis and technical factors maximizing biopsy yield. AJR Am J Roentgenol. 2021;217:1057–68.
Issa K, Diebo BG, Faloon M, Naziri Q, Pourtaheri S, Paulino CB, et al. The epidemiology of vertebral osteomyelitis in the United States from 1998 to 2013. Clin Spine Surg. 2018;31:E102–8.
Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur Spine J. 2013;22:2787–99.
Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, et al. Pyogenic spondylodiscitis: an overview. J Infect Public Health. 2010;3:5–16.
Wang Z, Lenehan B, Itshayek E, Boyd M, Dvorak M, Fisher C, et al. Primary pyogenic infection of the spine in intravenous drug users: a prospective observational study. Spine. 2012;37:685–92.
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, et al. 2015 Infectious Diseases Society of America (IDSA) clinical practice guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis Off Publ Infect Dis Soc Am. 2015;61:e26-46.
Gras G, Buzele R, Parienti JJ, Debiais F, Dinh A, Dupon M, et al. Microbiological diagnosis of vertebral osteomyelitis: relevance of second percutaneous biopsy following initial negative biopsy and limited yield of post-biopsy blood cultures. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2014;33:371–5.
Govender S. Spinal infections. J Bone Joint Surg Br. 2005;87-B:1454–8.
An HS, Seldomridge JA. Spinal infections: diagnostic tests and imaging studies. Clin Orthop. 2006;444:27–33.
Modic MT, Feiglin DH, Piraino DW, Boumphrey F, Weinstein MA, Duchesneau PM, et al. Vertebral osteomyelitis: assessment using MR. Radiology. 1985;157:157–66.
Ledermann HP, Schweitzer ME, Morrison WB, Carrino JA. MR imaging findings in spinal infections: rules or myths? Radiology. 2003;228:506–14.
Seller M, Burghardt RD, Rolling T, Hansen-Algenstaedt N, Schaefer C. Clostridium perfringens: a rare cause of spondylodiscitis case report and review of the literature. Br J Neurosurg. 2018;32:574–6.
Aghaei Lasboo A, Walker MT, Hijaz TA. An unusual appearance of discitis due to gas-forming Escherichia coli with associated pneumocephalus. Spine. 2010;35:E257-259.
Schömig F, Li Z, Becker L, Vu-Han T-L, Pumberger M, Diekhoff T. Gas within the intervertebral disc does not rule out spinal infection-a case series of 135 patients with spontaneous spondylodiscitis. Diagn Basel Switz. 2022;12:1089.
Yeh KJ, Husseini JS, Hemke R, Nelson SB, Chang CY. CT-guided discitis-osteomyelitis biopsies with negative microbiology: how many days should we wait before repeating the biopsy? Skeletal Radiol. 2020;49:619–23.
Chang CY, Simeone FJ, Nelson SB, Taneja AK, Huang AJ. Is biopsying the paravertebral soft tissue as effective as biopsying the disk or vertebral endplate? 10-year retrospective review of CT-guided biopsy of diskitis-osteomyelitis. AJR Am J Roentgenol. 2015;205:123–9.
Berns DH, Ross JS, Kormos D, Modic MT. The spinal vacuum phenomenon: evaluation by gradient echo MR imaging. J Comput Assist Tomogr. 1991;15:233–6.
Grenier N, Grossman RI, Schiebler ML, Yeager BA, Goldberg HI, Kressel HY. Degenerative lumbar disk disease: pitfalls and usefulness of MR imaging in detection of vacuum phenomenon. Radiology. 1987;164:861–5.
Beit Ner E, Chechik Y, Lambert L-A, Anekstein Y, Mirovsky Y, Smorgick Y. Gas forming infection of the spine: a systematic and narrative review. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2021;30:1708–20.
Cianci F, Ferraccioli G, Ferraccioli ES, Gremese E. Comprehensive review on intravertebral intraspinal, intrajoint, and intradiscal vacuum phenomenon: from anatomy and physiology to pathology. Mod Rheumatol. 2021;31:303–11.
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46.
Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. 3rd ed. Hoboken: John Wiley & Sons; 2003.
Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–13.
Mercaldo ND, Lau KF, Zhou XH. Confidence intervals for predictive values with an emphasis to case-control studies. Stat Med. 2007;26:2170–83.
Feng S-W, Chang M-C, Wu H-T, Yu J-K, Wang S-T, Liu C-L. Are intravertebral vacuum phenomena benign lesions? Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2011;20:1341–8.
Libicher M, Appelt A, Berger I, Baier M, Meeder P-J, Grafe I, et al. The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol. 2007;17:2248–52.
Magnusson W. Über Die Bedingungen Des Her- vortretens Der Wirklichen Gelenkspalte Auf Dem Röntgenbilde. Acta Radiol. 1937;18:733–41.
Ford LT, Gilula LA, Murphy WA, Gado M. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol. 1977;128:1056–7.
Ekşi MŞ, Özcan-Ekşi EE, Akkaş A, Orhun Ö, Arslan HN, Zarbizada M, et al. Intradiscal vacuum phenomenon and spinal degeneration: a cross-sectional analysis of 219 subjects. Curr Med Res Opin. 2022;38:255–63.
D’Anastasi M, Birkenmaier C, Schmidt GP, Wegener B, Reiser MF, Baur-Melnyk A. Correlation between vacuum phenomenon on CT and fluid on MRI in degenerative disks. AJR Am J Roentgenol. 2011;197:1182–9.
Schömig F, Palmowski Y, Nikiforov I, Hartwig T, Pumberger M, Schwabe P, et al. Burst fractures lead to a fracture-associated intervertebral vacuum phenomenon: a case series of 305 traumatic fractures of the thoracolumbar spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2021;30:3068–73.
Bang JH, Cho K-T. Rapidly progressive gas-containing lumbar spinal epidural abscess. Korean J Spine. 2015;12:139–42.
Wee LE, Hnin SWK, Xu Z, Lee LS-U. Strongyloides hyperinfection associated with Enterococcus faecalis bacteremia, meningitis, ventriculitis and gas-forming spondylodiscitis: a case report. Trop Med Infect Dis. 2020;5:44.
Coulier B. The spectrum of vacuum phenomenon and gas in spine. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR. 2004;87:9–16.
Belfquih H, El Mostarchid B, Akhaddar A, Gazzaz M, Boucetta M. Sciatica caused by lumbar epidural gas. Pan Afr Med J. 2014;18:162.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human subjects were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the MassGeneral Brigham (MGB) Human Research IRB (Protocol #: 2020P003048).
Informed consent
The study was approved by the local Institutional Review Board (IRB) and HIPAA compliant. Verbal consent for participation in the study was waived due to retrospective study design.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Husseini, J.S., Hanly, A., Omeroglu, E. et al. Can gas and infection coexist in the intervertebral disc? A retrospective analysis of percutaneously biopsied suspected discitis-osteomyelitis cases. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04631-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04631-5