Abstract
Objectives
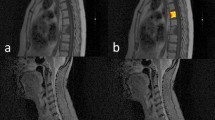
To analyze the characteristics of spinal metastasis in CT scans across diverse cancers for effective diagnosis and treatment, using MRI as the gold standard.
Methods
A retrospective study of 309 patients from four centers, who underwent concurrent CT and spinal MRI, revealing spinal metastasis, was conducted. Data on metastasis including total number, volume, visibility on CT (visible, indeterminate, or invisible), and type of bone change were collected. Through chi-square and Mann–Whitney U tests, we characterized the metastasis across diverse cancers and investigated the variation in the intra-individual ratio representing the percentage of lesions within each category for each patient.
Results
Out of 3333 spinal metastases from 309 patients, 55% were visible, 21% indeterminate, and 24% invisible. Sclerotic and lytic lesions made up 47% and 43% of the visible and indeterminate categories, respectively. Renal cell carcinoma (RCC), prostate cancer, and hepatocellular carcinoma (HCC) had the highest visibility at 86%, 73%, and 67% (p < 0.0001, p < 0.0001, and p = 0.003), while pancreatic cancer was lowest at 29% (p < 0.0001). RCC and HCC had significantly high lytic metastasis ratios (interquartile range (IQR) 0.96–1.0 and 0.31–1.0, p < 0.001 and p = 0.005). Prostate cancer exhibited a high sclerotic lesion ratio (IQR 0.52–0.97, p < 0.001). About 39% of individuals had invisible or indeterminate lesions, even with a single visible lesion on CT. The intra-individual ratio for indeterminate and invisible metastases surpassed 18%, regardless of the maximal size of the visible metastasis.
Conclusions
This study highlights the variability in characteristics of spinal metastasis based on the primary cancer type through unique lesion-centric analysis.





Similar content being viewed by others

Data Availability
The datasets generated or analyzed during the study are not publicly available due to institutional policy but are available from the corresponding author upon reasonable request.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- IHCC:
-
Intrahepatic cholangiocarcinoma
- RCC:
-
Renal cell carcinoma
- IQR:
-
Interquartile range
References
Coleman RE, Croucher PI, Padhani AR, Clézardin P, Chow E, Fallon M, et al. Bone metastases. Nat Rev Dis Primer. 2020;6:83.
Perrin RG, Laxton AW. Metastatic spine disease: epidemiology, pathophysiology, and evaluation of patients. Neurosurg Clin N Am. 2004;15:365–73.
Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008;7:459–66.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Sciubba DM, Petteys RJ, Dekutoski MB, Fisher CG, Fehlings MG, Ondra SL, et al. Diagnosis and management of metastatic spine disease: a review. J Neurosurg Spine. 2010;13:94–108.
O’Sullivan GJ. Imaging of bone metastasis: an update. World J Radiol. 2015;7:202.
Hussain I, Barzilai O, Reiner AS, McLaughlin L, DiStefano NM, Ogilvie S, et al. Spinal Instability Neoplastic Score component validation using patient-reported outcomes. J Neurosurg Spine. 2019;30:432–8.
Coleman RE. Skeletal complications of malignancy. Cancer. 1997;80:1588–94.
Roodman GD. Mechanisms of Bone Metastasis. N Engl J Med. 2004;350:1655–64.
Suva LJ, Washam C, Nicholas RW, Griffin RJ. Bone metastasis: mechanisms and therapeutic opportunities. Nat Rev Endocrinol. 2011;7:208–18.
Ishiwata Y, Hieda Y, Kaki S, Aso S, Horie K, Kobayashi Y, et al. Improved diagnostic accuracy of bone metastasis detection by water-HAP associated to non-contrast CT. Diagnostics. 2020;10:853.
Sciubba DM, Pennington Z, Colman MW, Goodwin CR, Laufer I, Patt JC, et al. Spinal metastases 2021: a review of the current state of the art and future directions. Spine J. 2021;21:1414–29.
Pennington Z, Ahmed AK, Cottrill E, Westbroek EM, Goodwin ML, Sciubba DM. Intra- and interobserver reliability of the Spinal Instability Neoplastic Score system for instability in spine metastases: a systematic review and meta-analysis. Ann Transl Med. 2019;7:218–218.
Yang H-L, Liu T, Wang X-M, Xu Y, Deng S-M. Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol. 2011;21:2604–17.
Jimenez-Carretero D, Bermejo-Peláez D, Nardelli P, Fraga P, Fraile E, San José Estépar R, et al. A graph-cut approach for pulmonary artery-vein segmentation in noncontrast CT images. Med Image Anal. 2019;52:144–59.
Kang MJ, Won Y-J, Lee JJ, Jung K-W, Kim H-J, Kong H-J, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat. 2022;54:330–44.
Mundy GR. Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer. 2002;2:584–93.
Maccauro G, Spinelli MS, Mauro S, Perisano C, Graci C, Rosa MA. Physiopathology of Spine Metastasis. Int J Surg Oncol. 2011;2011:1–8.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2019R1C1C1009044).
Funding
This study was funded by the Ministry of Science and ICT, South Korea (2019R1C1C1009044) on Dong Hyun Kim.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
•The study assessed spinal metastasis characteristics on CT scans across varied cancer types using MRI as a reference.
•Among the 3333 identified spinal metastases, 55% were visible on CT. RCC, prostate cancer, and HCC showed the highest visibility. Prostate cancer mainly displayed sclerotic lesions, whereas RCC and HCC were predominantly lytic.
•Differences in visibility and bone changes on CT scans across diverse cancers were validated through unique lesion-centric analysis.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, J.O., Kim, D.H., Chae, HD. et al. Assessing visibility and bone changes of spinal metastases in CT scans: a comprehensive analysis across diverse cancer types. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04623-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04623-5