Abstract
Purpose
Angular and longitudinal deformities of leg alignment create excessive stresses across joints, leading to pain and impaired function. Multiple measurements are used to assess these deformities on anteroposterior (AP) full-length radiographs. An artificial intelligence (AI) software automatically locates anatomical landmarks on AP full-length radiographs and performs 13 measurements to assess knee angular alignment and leg length. The primary aim of this study was to evaluate the agreements in LLD and knee alignment measurements between an AI software and two board-certified radiologists in patients without metal implants. The secondary aim was to assess time savings achieved by AI.
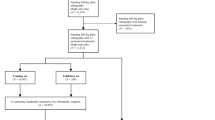
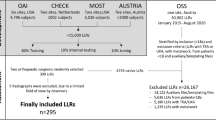
Methods
The measurements assessed in the study were hip-knee-angle (HKA), anatomical-tibiofemoral angle (aTFA), anatomical-mechanical-axis angle (AMA), joint-line-convergence angle (JLCA), mechanical-lateral-proximal-femur-angle (mLPFA), mechanical-lateral-distal-femur-angle (mLDFA), mechanical-medial-proximal-tibia-angle (mMPTA), mechanical-lateral-distal-tibia- angle (mLDTA), femur length, tibia length, full leg length, leg length discrepancy (LLD), and mechanical axis deviation (MAD). These measurements were performed by two radiologists and the AI software on 164 legs. Intraclass-correlation-coefficients (ICC) and Bland–Altman analyses were used to assess the AI’s performance.
Results
The AI software set incorrect landmarks for 11/164 legs. Excluding these cases, ICCs between the software and radiologists were excellent for 12/13 variables (11/13 with outliers included), and the AI software met performance targets for 11/13 variables (9/13 with outliers included). The mean reading time for the AI algorithm and two readers, respectively, was 38.3, 435.0, and 625.0 s.
Conclusion
This study demonstrated that, with few exceptions, this AI-based software reliably generated measurements for most variables in the study and provided substantial time savings.





Similar content being viewed by others
References
Gordon JE, Davis LE. Leg length discrepancy: the natural history (and what do we really know). J Pediatr Orthop. 2019;39(Issue 6, Supplement 1 Suppl 1):S10-s13.
Siffert RS. Lower limb-length discrepancy. J Bone Joint Surg Am. 1987;69(7):1100–6.
Gurney B. Leg length discrepancy. Gait Posture. 2002;15(2):195–206.
Gofton JP, Trueman GE. Studies in osteoarthritis of the hip. II. Osteoarthritis of the hip and leg-length disparity. Can Med Assoc J. 1971;104(9):791–9.
Applebaum A, Nessim A, Cho W. Overview and spinal implications of leg length discrepancy: narrative review. Clin Orthop Surg. 2021;13(2):127–34.
Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci. 2010;6(3):393–8.
Ghanem I, Karam JA, Widmann RF. Surgical epiphysiodesis indications and techniques: update. Curr Opin Pediatr. 2011;23(1):53–9.
Thienpont E, et al. Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg. 2017;137(3):393–400.
Wang B, et al. Valgus malalignment and prevalence of lateral compartmental radiographic knee osteoarthritis (OA): the Wuchuan OA study. Int J Rheum Dis. 2018;21(7):1385–90.
Sharma L, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940–5.
Schwarz GM, et al. Artificial intelligence enables reliable and standardized measurements of implant alignment in long leg radiographs with total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2538–47.
Simon S, et al. Fully automated deep learning for knee alignment assessment in lower extremity radiographs: a cross-sectional diagnostic study. Skeletal Radiol. 2022;51(6):1249–59.
Kallogjeri D, Spitznagel EL Jr, Piccirillo JF. Importance of defining and interpreting a clinically meaningful difference in clinical research. JAMA Otolaryngol-Head Neck Surg. 2020;146(2):101–2.
Martin Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–10.
Hodson TO. Root-mean-square error (RMSE) or mean absolute error (MAE): when to use them or not. Geosci Model Dev. 2022;15(14):5481–7.
Obuchowski NA, Subhas N, Schoenhagen P. Testing for interchangeability of imaging tests. Acad Radiol. 2014;21(11):1483–9.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–90.
Lu MJ, Zhong WH, Liu YX, Miao HZ, Li YC, Ji MH. Sample size for assessing agreement between two methods of measurement by Bland-Altman method. Int J Biostat. 2016;12(2):/j/ijb.2016.12.issue-2/ijb-2015-0039/ijb-2015-0039.xml. https://doi.org/10.1515/ijb-2015-0039.
Lin YH, Chang FS, Chen KH, Huang KC, Su KC. Mismatch between femur and tibia coronal alignment in the knee joint: classification of five lower limb types according to femoral and tibial mechanical alignment. BMC Musculoskelet Disord. 2018;19(1):411. https://doi.org/10.1186/s12891-018-2335-9.
Marques Luis N, Varatojo R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021;6(6):487–94.
Bellemans J, et al. The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients?: the concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1):45–53.
Shimizu M, et al. Examination of the changes in lower extremities related to progression of adult spinal deformity: a longitudinal study of over 22 years. Sci Rep. 2020;10(1):11605.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AC: consultant: ICON Medical and TREACE Medical Concepts Inc.; book royalties: Jaypee, Wolters; speaker: Siemens; medical advisor: Imagebiopsy Lab Inc.; research grant: Imagebiopsy Lab Inc.
OA: consultant: ImageBiopsy Lab.
PP: consultant: ImageBiopsy Lab.
JW: consultant: Ethicon.
MD: employee: ImageBiopsy Lab GmbH.
AH: employee: ImageBiopsy Lab GmbH.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Summary statement
Our study showed that, with the exception of outlier cases, AI-based software demonstrated reliable radiographic assessment of knee angular alignment and leg length determination for most measurements along with significant time savings.
Key points
1. The artificial intelligence algorithm demonstrated excellent agreement (intraclass correlation coefficients > 0.75) for 12/13 measurements used in the study when outlier cases were excluded.
2. Artificial intelligence met the performance targets based on Bland-Altman analysis for 11/13 variables when outlier cases were excluded.
3. The artificial intelligence system generated measurements more than 90% faster than the expert readers.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Archer, H., Reine, S., Xia, S. et al. Deep learning generated lower extremity radiographic measurements are adequate for quick assessment of knee angular alignment and leg length determination. Skeletal Radiol 53, 923–933 (2024). https://doi.org/10.1007/s00256-023-04502-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-023-04502-5