Abstract
Purpose
Since the critical shoulder angle (CSA) is considered a risk factor for shoulder pathology and the intra- and inter-rater variabilities in its calculation are not negligible, we developed a deep learning model that calculates it automatically and accurately.
Methods
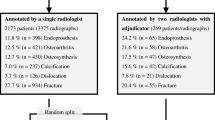
We used a dataset of 8467 anteroposterior x-ray images of the shoulder annotated with 3 landmarks of interest. A Convolutional Neural Network model coupled with a spatial to numerical transform (DSNT) layer was used to predict the landmark coordinates from which the CSA was calculated. The performances were evaluated by calculating the Euclidean distance between the ground truth coordinates and the predicted ones normalized with respect to the distance between the first and the second points, and the error between the CSA angle measured by a human observer and the predicted one.
Results
Regarding the normalized point distances, we obtained a median error of 2.9%, 2.5%, and 2% for the three points among the entire set. Considering CSA calculations, the median errors were 1° (standard deviation 1.2°), 0.88° (standard deviation 0.87°), and 0.99° (standard deviation 1°) for angles below 30°, between 30° and 35°, and above 35°, respectively.
Discussion
These results demonstrate that the model has the potential to be used in clinical settings where the replicability is important. The reported standard error of the CSA measurement is greater than 2° that is above the median error of our model, indicating a potential accuracy sufficient to be used in a clinical setting.





Similar content being viewed by others
Availability of data and materials
The images are confidential. The other data and software are available from the corresponding author upon reasonable request.
Change history
05 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00256-022-04052-2
References
Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Jt J. 2013;95 B(7):935–41.
Rose-Reneau Z, Moorefield AK, Schirmer D, Ismailov E, Downing R, Wright BW. The critical shoulder angle as a diagnostic measure for osteoarthritis and rotator cuff pathology. Cureus. 2020;12(11):e11447.
Viehöfer AF, Snedeker JG, Baumgartner D, Gerber C. Glenohumeral joint reaction forces increase with critical shoulder angles representative of osteoarthritis - a biomechanical analysis. J Orthop Res. 2016;34(6):1047–52.
Tauber M, Habermeyer P, Zumbansen N, Martetschläger F. Lateral acromioplasty for correction of the critical shoulder angle. Obere Extrem. 2020;15(3):228–32.
Spiegl UJ, Horan MP, Smith SW, Ho CP, Millett PJ. The critical shoulder angle is associated with rotator cuff tears and shoulder osteoarthritis and is better assessed with radiographs over MRI. Knee Surgery, Sport Traumatol Arthrosc. 2016;24(7):2244–51.
Galbusera F, Bassani T, Costa F, Brayda-Bruno M, Zerbi A, Wilke HJ. Artificial neural networks for the recognition of vertebral landmarks in the lumbar spine. Comput Methods Biomech Biomed Eng Imaging Vis. 2018;6(4):447–52.
Chung SW, Han SS, Lee JW, Oh K-S, Kim NR, Yoon JP, et al. Automated detection and classification of the proximal humerus fracture by using deep learning algorithm. Acta Orthop. 2018;89(4):468–73.
He Z, Morgan S, Prendergast L. Numerical coordinate regression with convolutional neural networks. 2018. arXiv preprint arXiv:1801.07372.
Szegedy C, Liu W, Jia Y, Sermanet P, Reed S, Anguelov D, et al. Going deeper with convolutions. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 2015. pp. 1–9.
Galbusera F, Niemeyer F, Joachim H, Tito W, Gloria B, Carla C, et al. Fully automated radiological analysis of spinal disorders and deformities : a deep learning approach. Eur Spine J. 2019;28(5):951–60.
Cina A, Bassani T, Panico M, Luca A, Masharawi Y, Bruno MB, et al. 2 - step deep learning model for landmarks localization in spine radiographs. Sci Rep. 2021;0123456789:1–12.
Paszke A, Gross S, Massa F, Lerer A, Bradbury J, Chanan G, et al. PyTorch: an imperative style, high-performance deep learning library. NeurIPS. 2019. p. 32.
Urban G, Porhemmat S, Stark M, Feeley B, Okada K, Baldi P. Classifying shoulder implants in X-ray images using deep learning. Comput Struct Biotechnol J. 2020;18:967–72.
Shim E, Kim JY, Yoon JP, Ki S-Y, Lho T, Kim Y, et al. Automated rotator cuff tear classification using 3D convolutional neural network. Sci Rep. 2020;10(1):15632.
Taghizadeh E, Truffer O, Becce F, Eminian S, Gidoin S, Terrier A, et al. Deep learning for the rapid automatic quantification and characterization of rotator cuff muscle degeneration from shoulder CT datasets. Eur Radiol. 2021;31(1):181–90.
Medina G, Buckless CG, Thomasson E, Oh LS, Torriani M. Deep learning method for segmentation of rotator cuff muscles on MR images. Skeletal Radiol. 2021;50(4):683–92.
Cantarelli Rodrigues T, Deniz CM, Alaia EF, Gorelik N, Babb JS, Dublin J, et al. Three-dimensional MRI bone models of the glenohumeral joint using deep learning: evaluation of normal anatomy and glenoid bone loss. Radiol Artif Intell. 2020;2(5):e190116.
Funding
The study was funded by the Italian Ministry of Health (“Ricerca Corrente”).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by our Institutional Review Board.
Consent to participate
All images were fully anonymized and all subjects gave informed consent for participation.
Consent for publication
All subjects gave informed consent for scientific use of the data including publication of results.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. Luca Maria Sconfienza’s affiliations should be 2 and 5.
Rights and permissions
About this article
Cite this article
Minelli, M., Cina, A., Galbusera, F. et al. Measuring the critical shoulder angle on radiographs: an accurate and repeatable deep learning model. Skeletal Radiol 51, 1873–1878 (2022). https://doi.org/10.1007/s00256-022-04041-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04041-5