Abstract
Objective
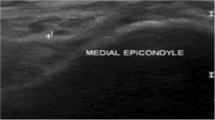
To evaluate the usefulness of the longitudinal extent (LE) of high ulnar nerve signal intensity (SI) for the diagnosis of ulnar neuropathy at the elbow (UNE).
Materials and methods
This retrospective study included 68 patients who underwent elbow MRI. Twenty-seven and 41 patients were enrolled in the UNE and control groups, respectively. Qualitative and quantitative analyses of the SI and size of the ulnar nerve at the cubital tunnel, proximal, and distal to the cubital tunnel were performed. Cross-sectional area (CSA) and nerve-to-muscle contrast ratio (NMCR) were measured at each level. The LE of the hyperintense ulnar nerve was evaluated using axial and coronal images. The presence of space-occupying lesions (SOLs), subluxation, and muscle denervation were recorded. Univariate and multivariate analyses were performed to identify independent predictive factors.
Results
Ulnar nerve hyperintensity at and distal to the cubital tunnel, presence of compression, SOL, muscle denervation, LE of hyperintense ulnar nerve, NMCR, and CSA at and distal to the cubital tunnel significantly differed between the two groups. Multivariate logistic regression analysis showed that the LE of the hyperintense ulnar nerve and CSA at the cubital tunnel were independent predictive factors for UNE (p < 0.05).
Conclusion
LE of the hyperintense ulnar nerve could be a useful predictive factor for UNE.



Similar content being viewed by others
References
Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006;26(5):1267–87.
Landau ME, Campbell WW. Clinical features and electrodiagnosis of ulnar neuropathies. Phys Med Rehabil Clin N Am. 2013;24(1):49–66.
Keen NN, Chin CT, Engstrom JW, Saloner D, Steinbach LS. Diagnosing ulnar neuropathy at the elbow using magnetic resonance neurography. Skeletal Radiol. 2012;41(4):401–7.
Baumer P, Dombert T, Staub F, Kaestel T, Bartsch AJ, Heiland S, et al. Ulnar neuropathy at the elbow: MR neurography–nerve T2 signal increase and caliber. Radiology. 2011;260(1):199–206.
Beekman R, Schoemaker MC, Van Der Plas JP, Van Den Berg LH, Franssen H, Wokke JH, et al. Diagnostic value of high-resolution sonography in ulnar neuropathy at the elbow. Neurology. 2004;62(5):767–73.
Campbell WW. Ulnar neuropathy at the elbow. Muscle Nerve. 2000;23(4):450–2.
Antoniadis G, Richter HP. Pain after surgery for ulnar neuropathy at the elbow: a continuing challenge. Neurosurgery. 1997; 41(3):585–589; discussion 589–591.
Breitenseher JB, Kranz G, Hold A, Berzaczy D, Nemec SF, Sycha T, et al. MR neurography of ulnar nerve entrapment at the cubital tunnel: a diffusion tensor imaging study. Eur Radiol. 2015;25(7):1911–8.
Nakashian MN, Ireland D, Kane PM. Cubital tunnel syndrome: current concepts. Curr Rev Musculoskelet Med. 2020;13(4):520–4.
Britz GW, Haynor DR, Kuntz C, Goodkin R, Gitter A, Maravilla K, et al. Ulnar nerve entrapment at the elbow: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery. 1996; 38(3):458–465; discussion 465.
Terayama Y, Uchiyama S, Ueda K, Iwakura N, Ikegami S, Kato Y, et al. Optimal measurement level and ulnar nerve cross-sectional area cutoff threshold for identifying ulnar neuropathy at the elbow by MRI and ultrasonography. The Journal of hand surgery. 2018;43(6):529–36.
Vucic S, Cordato DJ, Yiannikas C, Schwartz RS, Shnier RC. Utility of magnetic resonance imaging in diagnosing ulnar neuropathy at the elbow. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. 2006;117(3):590–5.
Kawahara Y, Yamaguchi T, Honda Y, Tomita Y, Uetani M. The ulnar nerve at elbow extension and flexion: assessment of position and signal intensity on MR images. Radiology. 2016;280(2):483–92.
Gupta R, Steward O. Chronic nerve compression induces concurrent apoptosis and proliferation of Schwann cells. J Comp Neurol. 2003;461(2):174–86.
Rempel DM, Diao E. Entrapment neuropathies: pathophysiology and pathogenesis. J Electromyogr Kinesiol. 2004;14(1):71–5.
Tapadia M, Mozaffar T, Gupta R. Compressive neuropathies of the upper extremity: update on pathophysiology, classification, and electrodiagnostic findings. The Journal of hand surgery. 2010;35(4):668–77.
Sakurai M, Miyasaka Y. Neural fibrosis and the effect of neurolysis. J Bone Joint Surg Br. 1986;68(3):483–8.
Husarik DB, Saupe N, Pfirrmann CW, Jost B, Hodler J, Zanetti M. Elbow nerves: MR findings in 60 asymptomatic subjects–normal anatomy, variants, and pitfalls. Radiology. 2009;252(1):148–56.
Tagliafico AS. Ulnar neuropathy at the elbow: is MR imaging reliable? Radiology. 2011; 261(2):659–660; author reply 660.
Sivakumaran T, Sneag DB, Lin B, Endo Y. MRI of the ulnar nerve pre- and post-transposition: imaging features and rater agreement. Skeletal Radiol. 2021;50(3):559–70.
Mansournia MA, Geroldinger A, Greenland S, Heinze G. Separation in logistic regression: causes, consequences, and control. Am J Epidemiol. 2018;187(4):864–70.
Chang KV, Wu WT, Han DS, Ozcakar L. Ulnar nerve cross-sectional area for the diagnosis of cubital tunnel syndrome: a meta-analysis of ultrasonographic measurements. Arch Phys Med Rehabil. 2018;99(4):743–57.
Chhabra A, Madhuranthakam AJ, Andreisek G. Magnetic resonance neurography: current perspectives and literature review. Eur Radiol. 2018;28(2):698–707.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by the institutional review board, and the requirement for informed consent was waived.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S., Chung, B.M., Kim, W.T. et al. Diagnosing ulnar neuropathy at the elbow on MRI: importance of the longitudinal extent of the hyperintense ulnar nerve. Skeletal Radiol 51, 1473–1481 (2022). https://doi.org/10.1007/s00256-022-03990-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-03990-1