Abstract
Objective
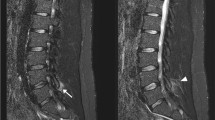
Obesity has been proposed as a risk factor for low back pain (LBP) and intervertebral disc degeneration (IVDD). Even though body mass index (BMI) is used as a parameter for obesity, it could not represent percentage and distribution of the body fat. Subcutaneous fat tissue thickness (SFTT) was proposed as one of the magnetic resonance imaging (MRI) parameters to evaluate the percentage of the body fat. In this study, we aimed to find out whether SFTT at lower back correlated with LBP and spine degeneration.
Materials and methods
We retrospectively reviewed a database of the patients with LBP. Concomitantly, asymptomatic control subjects were retrieved. Patients and control subjects were evaluated in terms of IVDD and Modic changes at all lumbar levels on MRI. SFTT was measured both on MRI and computed tomography (CT) scans, where applicable.
Results
SFTT at the lumbar spine had moderate-to-strong correlations with BMI. SFTT at L1-L2 level was significantly associated with severe IVDD at L5-S1 level, and Modic changes at L4-L5 and L5-S1 levels. BMI had no significant association with severe IVDD and Modic changes at lumbar spine. BMI and mean SFTT of all lumbar levels had ORs of 0.735 (95% CI: 0.631–0.857, p < 0.001) and 1.389 (95% CI: 1.266–1.524, p < 0.001) in predicting symptomatic subjects with LBP.
Conclusion
SFTT at upper lumbar levels could predict severe IVDD and Modic changes better than BMI, specifically in men. SFTT was better than BMI in predicting a symptomatic patient with LBP.





Similar content being viewed by others
References
Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA, American Society of Interventional Pain P. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12:E35-70.
Ozcan-Eksi EE, Eksi MS, Akcal MA. Severe lumbar intervertebral disc degeneration is associated with modic changes and fatty infiltration in the paraspinal muscles at all lumbar levels, Except for L1–L2: a cross-sectional analysis of 50 symptomatic women and 50 age-matched symptomatic men. World Neurosurg. 2019;122:e1069–77.
Leino-Arjas P, Kaila-Kangas L, Solovieva S, Riihimaki H, Kirjonen J, Reunanen A. Serum lipids and low back pain: an association? A follow-up study of a working population sample. Spine (Phila Pa 1976). 2006;31:1032–7.
Kauppila LI. Atherosclerosis and disc degeneration/low-back pain–a systematic review. Eur J Vasc Endovasc Surg. 2009;37:661–70.
Takatalo J, Karppinen J, Taimela S, Niinimaki J, Laitinen J, Sequeiros RB, et al. Association of abdominal obesity with lumbar disc degeneration–a magnetic resonance imaging study. PLoS One. 2013;8:e56244.
Samartzis D, Karppinen J, Mok F, Fong DY, Luk KD, Cheung KM. A population-based study of juvenile disc degeneration and its association with overweight and obesity, low back pain, and diminished functional status. J Bone Joint Surg Am. 2011;93:662–70.
Samartzis D, Karppinen J, Chan D, Luk KD, Cheung KM. The association of lumbar intervertebral disc degeneration on magnetic resonance imaging with body mass index in overweight and obese adults: a population-based study. Arthritis Rheum. 2012;64:1488–96.
Liuke M, Solovieva S, Lamminen A, Luoma K, Leino-Arjas P, Luukkonen R, et al. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes (Lond). 2005;29:903–8.
Gurunathan U, Myles PS. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth. 2016;116:319–21.
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019.
Roubenoff R. Applications of bioelectrical impedance analysis for body composition to epidemiologic studies. Am J Clin Nutr. 1996;64:459S-S462.
Coutinho T, Goel K, Correa de Sa D, Kragelund C, Kanaya AM, Zeller M, et al. Central obesity and survival in subjects with coronary artery disease: a systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol. 2011;57:1877–86.
Dutton DJ, McLaren L. The usefulness of “corrected” body mass index vs. self-reported body mass index: comparing the population distributions, sensitivity, specificity, and predictive utility of three correction equations using Canadian population-based data. BMC Public Health. 2014;14:430.
Smith SR, Lovejoy JC, Greenway F, Ryan D, deJonge L, de la Bretonne J, et al. Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism. 2001;50:425–35.
Kim J, Lim H, Lee SI, Kim YJ. Thickness of rectus abdominis muscle and abdominal subcutaneous fat tissue in adult women: correlation with age, pregnancy, laparotomy, and body mass index. Arch Plast Surg. 2012;39:528–33.
Hernandez R, Younan Y, Mulligan M, Singer AD, Sharma GB, Umpierrez M, et al. Correlation between subcutaneous fat measurements in knee MRI and BMI: relationship to obesity and related co-morbidities. Acta Radiol Open. 2019;8:2058460119853541.
Seidell JC, Bakker CJ, van der Kooy K. Imaging techniques for measuring adipose-tissue distribution–a comparison between computed tomography and 1.5-T magnetic resonance. Am J Clin Nutr. 1990;51:953–7.
Yang L, Mu L, Huang K, Zhang T, Mei Z, Zeng W, et al. Abdominal adipose tissue thickness measured using magnetic resonance imaging is associated with lumbar disc degeneration in a Chinese patient population. Oncotarget. 2016;7:82055–62.
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26:1873–8.
Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–86.
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–9.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Lee JJ, Odeh KI, Holcombe SA, Patel RD, Wang SC, Goulet JA, et al. Fat thickness as a risk factor for infection in lumbar spine surgery. Orthopedics. 2016;39:e1124–8.
Nadeem B, Bacha R, Gilani SA. Correlation of subcutaneous fat measured on ultrasound with body mass index. J Med Ultrasound. 2018;26:205–9.
Özcan-Ekşi EE, Turgut VU, Küçüksüleymanoğlu D, Ekşi MŞ. Obesity could be associated with poor paraspinal muscle quality at upper lumbar levels and degenerated spine at lower lumbar levels: Is this a domino effect? J Clin Neurosci. 2021;94:120–7.
Kvist H, Chowdhury B, Grangard U, Tylen U, Sjostrom L. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48:1351–61.
Zore T, Palafox M, Reue K. Sex differences in obesity, lipid metabolism, and inflammation-A role for the sex chromosomes? Mol Metab. 2018;15:35–44.
Stevens J, Katz EG, Huxley RR. Associations between gender, age and waist circumference. Eur J Clin Nutr. 2010;64:6–15.
Eksi MS, Kara M, Ozcan-Eksi EE, Aytar MH, Gungor A, Ozgen S, et al. Is diabetes mellitus a risk factor for modic changes?: a novel model to understand the association between intervertebral disc degeneration and end-plate changes. J Orthop Sci. 2020;25:571–5.
Cao J, Kong L, Meng F, Zhang Y, Shen Y. Impact of obesity on lumbar spinal surgery outcomes. J Clin Neurosci. 2016;28:1–6.
Sang C, Chen X, Ren H, Meng Z, Jiang J, Qin Y. Correlation between lumbar multifidus fat infiltration and lumbar postoperative infection: a retrospective case-control study. BMC Surg. 2020;20:35.
Peng W, Liang Y, Lu T, Li M, Li DS, Du KH, et al. Multivariate analysis of incision infection after posterior lumbar surgery in diabetic patients: a single-center retrospective analysis. Medicine. 2019;98:e15935.
Acknowledgements
We thank to Göksu Bozdereli Berikol, M.D. for her contributions to the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Özcan-Ekşi, E.E., Kara, M., Berikol, G. et al. A new radiological index for the assessment of higher body fat status and lumbar spine degeneration. Skeletal Radiol 51, 1261–1271 (2022). https://doi.org/10.1007/s00256-021-03957-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03957-8