Abstract
Objective
To report the prevalence of MRI features commonly associated with posterior ankle impingement syndrome in elite ballet dancers and athletes and to compare findings between groups.
Materials and methods
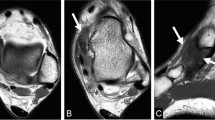
Thirty-eight professional ballet dancers (47.4% women) were age- and sex-matched to 38 elite soccer or cricket fast bowler athletes. All participants were training, playing, and performing at full workload and underwent 3.0-T standardised magnetic resonance imaging of one ankle. De-identified images were assessed by one senior musculoskeletal radiologist for findings associated with posterior ankle impingement syndrome (os trigonum, Stieda process, posterior talocrural and subtalar joint effusion-synovitis, flexor hallucis longus tendon pathology and tenosynovitis, and posterior ankle bone marrow oedema). Imaging scoring reliability testing was performed.
Results
Posterior talocrural effusion-synovitis (90.8%) and subtalar joint effusion-synovitis (93.4%) were common in both groups, as well as the presence of either an os trigonum or Stieda process (61.8%). Athletes had a higher prevalence of either os trigonum or Stieda process than dancers (74%, 50% respectively, P = 0.03). Male athletes had a higher prevalence of either os trigonum or Stieda process than male dancers (90%, 50% respectively, P = 0.01), or female athletes (56%, P = 0.02). Posterior subtalar joint effusion-synovitis size was larger in dancers than athletes (P = 0.02). Male and female dancers had similar imaging findings. There was at least moderate interobserver and intraobserver agreement for most MRI findings.
Conclusion
Imaging features associated with posterior impingement were prevalent in all groups. The high prevalence of os trigonum or Stieda process in male athletes suggests that this is a typical finding in this population.






Similar content being viewed by others
References
Peace KAL, Hillier JC, Hulme A, Healy JC. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59(11):1025–33.
Hamilton W. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Jt Surgery. 1996;78(10):1491–500.
Brodsky AE, Khalil MA. Talar compression syndrome. Foot Ankle. 1987;7(6):338–44.
Wredmark T, Carlstedt CA, Bauer H, Saartok T. Os trigonum syndrome: a clinical entity in ballet dancers. Foot Ankle. 1991;11(6):404–6.
Marotta JJ, Micheli LJ. Os trigonum impingement in dancers. Am J Sports Med. 1992;20(5):533–6.
Bureau NJ, Cardinal E, Hobden R, Aubin B. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology. 2000;215(2):497–503.
Ribbans WJ, Ribbans HA, Cruickshank JA, Wood EV. The management of posterior ankle impingement syndrome in sport: a review. Foot Ankle Surg. 2015;21(1):1–10.
Kalbouneh HM, Alajoulin O, Alsalem M, et al. Incidence of symptomatic os trigonum among nonathletic patients with ankle sprain. Surg Radiol Anat. 2019;41(12):1433–9.
Mansingh A. Posterior ankle impingement in fast bowlers in cricket. West Indian Med J. 2011;60(1):77–81.
Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120–4.
Hedrick MR, McBryde AM. Posterior ankle impingement. Foot Ankle Int. 1994;15(1):2–8.
Hamilton W. Stenosing tenosynovitis of the flexor hallucis longus tendon and posterior impingement upon the os trigonum in ballet dancers. Foot Ankle. 1982;3(2):74–80.
Messiou C, Robinson P, O’Connor PJ, Grainger A. Subacute posteromedial impingement of the ankle in athletes: MR imaging evaluation and ultrasound guided therapy. Skeletal Radiol. 2006;35(2):88–94.
van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16(8):871–6.
Coskun N, Yuksel M, Cevener M, et al. Incidence of accessory ossicles and sesamoid bones in the feet: a radiographic study of the Turkish subjects. Surg Radiol Anat. 2009;31(1):19–24.
Cicek ED, Bankaoglu M. Prevalence of elongated posterior talar process (Stieda process) detected by radiography. Int J Morphol. 2020;38(4):894–8.
Zwiers R, Baltes TPA, Opdam KTM, Wiegerinck JI, van Dijk CN. Prevalence of os trigonum on CT imaging. Foot Ankle Int. 2018;39(3):338–42.
Zwiers R, Dobbe JGG, Streekstra GJ, et al. Exorotated radiographic views have additional diagnostic value in detecting an osseous impediment in patients with posterior ankle impingement. Jt Disord Orthop Sport Med. 2019;4(4):181–7.
Fu X, Ma L, Zeng Y, et al. Implications of classification of os trigonum: a study based on computed tomography three-dimensional imaging. Med Sci Monit. 2019;25:1423–8.
Russell JA, Shave RM, Yoshioka H, Kruse DW, Koutedakis Y, Wyon MA. Magnetic resonance imaging of the ankle in female ballet dancers en pointe. Acta Radiol. 2010;51(6):655–61.
Felton PJ, Lister SL, Worthington PJ, King MA. Comparison of biomechanical characteristics between male and female elite fast bowlers. J Sport Sci. 2019;37(6):665–70.
Russell JA, Shave RM, Kruse DW, Koutedakis Y, Wyon MA. Ankle and foot contributions to extreme plantar- and dorsiflexion in female ballet dancers. Foot Ankle Int. 2011;32(2):183–8.
Tol JL, Slim E, van Soest AJ, van Dijk CN. The relationship of the kicking action in soccer and anterior ankle impingement syndrome. Am J Sports Med. 2002;30(1):45–50.
Spratford W, Hicks A. Increased delivery stride length places greater loads on the ankle joint in elite male cricket fast bowlers. J Sport Sci. 2014;32(12):1101–9.
Worthington P, King M, Ranson C. The influence of cricket fast bowlers’ front leg technique on peak ground reaction forces. J Sport Sci. 2013;31(4):434–41.
Orloff H, Sumida B, Chow J, Habibi L, Fujino A, Kramer B. Ground reaction forces and kinematics of plant leg position during instep kicking in male and female collegiate soccer players. Sport Biomech. 2008;7(2):238–47.
Walter HL. Ground reaction forces in ballet dancers landing in flat shoes versus pointe shoes. J Danc Med Sci. 2011;15(2):61.
McPherson AM, Schrader JW, Docherty CL. Ground reaction forces in ballet differences resulting from footwear and jump conditions. J Danc Med Sci. 2019;23(1):34–9.
Stuelcken MC, Sinclair PJ. A pilot study of the front foot ground reaction forces in elite female fast bowlers. J Sci Med Sport. 2009;12(2):258–61.
Clarsen B, Rønsen O, Myklebust G, Flørenes TW, Bahr R. The Oslo Sports Trauma Research Center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. 2014;48(9):754–60.
Bahr R. No injuries, but plenty of pain? On the methodology for recording overuse symptoms in sports. Br J Sports Med. 2009;43(13):966–72.
Harringe ML, Lindblad S, Werner S. Do team gymnasts compete in spite of symptoms from an injury? Br J Sports Med. 2004;38(4):398–401.
Guermazi A, Roemer FW, Crema MD, Englund M, Hayashi D. Imaging of non-osteochondral tissues in osteoarthritis. Osteoarthr Cart. 2014;22(10):1590–605.
Knapik DM, Guraya SS, Jones JA, Cooperman DR, Liu RW. Incidence and fusion of os trigonum in a healthy pediatric population. J Pediatr Orthop. 2019;39(9):e718–21.
Gursoy M, Dag F, Mete BD, Bulut T, Uluc ME. The anatomic variations of the posterior talofibular ligament associated with os trigonum and pathologies of related structures. Surg Radiol Anat. 2015;37(8):955–62.
Schweitzer ME, van Leersum M, Ehrlich SS, Wapner K. Fluid in normal and abnormal ankle joints: amount and distribution as seen on MR images. Am J Roentgenol. 1994;162(1):111–4.
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37–46.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–90.
McDougall A. The os trigonum. J Bone Jt Surgery. 1955;37(2):257–65.
Tsuruta T, Shiokawa Y, Kato A, et al. Radiological study of the accessory skeletal elements in the foot and ankle (author’s transl). Nihon Seikeigeka Gakkai Zasshi. 1981;55(4):357–70.
Ozer M, Yildirim A. Evaluation of the prevalence of os trigonum and talus osteochondral lesions in ankle magnetic resonance imaging of patients with ankle impingement syndrome. J Foot Ankle Surg. 2019;58(2):273–7.
McCormack M, Briggs J, Hakim A, Grahame R. Joint laxity and the benign joint hypermobility syndrome in student and professional ballet dancers. J Rheumatol. 2004;31(1):173–8.
Russell JA, Kruse DW, Koutedakis Y, Mcewan IM, Wyon MA. Pathoanatomy of posterior ankle impingement in ballet dancers. Clin Anat. 2010;23(6):613–21.
Kudas S, Donmez G, Isik C, Celebi M, Cay N, Bozkurt M. Posterior ankle impingement syndrome in football players: case series of 26 elite athletes. Acta Orthop Traumatol Turc. 2016;50(6):649–54.
Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability. Foot Ankle Spec. 2014;7(4):298–326.
Hertel J. Functional instability following lateral ankle sprain. Sport Med. 2000;29(5):361–71.
Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sport Exerc. 1999;31(11):1501–8.
Ménétrey J, Fritschy D. Subtalar subluxation in ballet dancers. Am J Sports Med. 1999;27(2):143–9.
Russell JA, Yoshioka H. Assessment of female ballet dancers’ ankles in the en pointe position using high field strength magnetic resonance imaging. Acta Radiol. 2016;57(8):978–84.
Acknowledgements
A sincere thank you to the dancers and athletes of The Australian Ballet, Cricket Australia, Cricket Victoria and Melbourne City Football Club for their participation in this study. The authors sincerely thank A. Kountouris of Cricket Australia for his collaborative efforts; K. Sims, N. Adcock, M. Tucker, D. Stanborough, L. Kennedy, L. Poon, and B. Robertson for assisting in participant recruitment; S. Emery, M. Hook, V. Tran, and J. Baillie for their assistance with data collection; A. Garnham, J. Walsh and T. O’Shea for their assistance in image acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baillie, P., Cook, J., Ferrar, K. et al. Magnetic resonance imaging findings associated with posterior ankle impingement syndrome are prevalent in elite ballet dancers and athletes. Skeletal Radiol 50, 2423–2431 (2021). https://doi.org/10.1007/s00256-021-03811-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03811-x