Abstract
Objective
To implement an automated quality assurance tool to prospectively track discrepancies in musculoskeletal (MSK) exams submitted for second-opinion radiology interpretation at a tertiary center.
Methods
From 2013 to 2020, a standardized template was included in re-interpretation MSK reports, and a concordance assessment compared with primary interpretation was assigned. Analysis of standardized template implementation and discordance rates was performed. Of the re-interpretations that demonstrated likely clinically relevant discordance, a sample was randomly selected and the EMR was reviewed to evaluate the impact on patient care and change in medical management.
Results
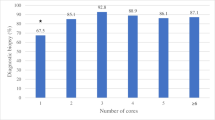
A total of 1052 re-interpretations were identified using the standardized template. Services with higher requests for second-opinion interpretation were oncology (n = 351, 33%) and orthopedic surgery (n = 255, 24%). Overall utilization rate of the template was 65% with marked decreased during the last year (22% rate). In comparison to the primary report, there was a 30% discordance rate (n = 309) with 18% (n = 184) classified as likely clinically relevant. From the subset of discrepancies that could be clinically relevant, there was a change in management in 63% of the cases (19/30) with the re-interpretation ultimately proving correct in 80% of the cases (24/30).
Conclusion
Implementation of a quality assurance tool embedded in the radiology workflow of second-opinion interpretations can facilitate the analysis of patient care impact; however, stricter implementation is necessary. Oncologic studies were the most common indication for re-interpretations. Although the primary and second interpretations in the majority of cases were in agreement, subspecialty MSK radiology interpretation was shown to be more accurate than primary interpretations and impacted clinical management in cases of discrepancy.








Similar content being viewed by others
References
Strosberg C, Gibbs J, Braswell D, Leslie RR, Messina J, Centeno BA, et al. Second opinion reviews for cancer diagnoses in anatomic pathology: a comprehensive cancer center’s experience. Anticancer Res. 2018;38:2989–94.
Zan E, Yousem DM, Carone M, Lewin JS. Second-opinion consultations in neuroradiology. Radiology. 2010;255:135–41.
Loevner LA, Sonners AI, Schulman BJ, Slawek K, Weber RS, Rosenthal DI, et al. Reinterpretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. Am J Neuroradiol. 2002;23:1622–6.
Chalian M, Del Grande F, Thakkar RS, Jalali SF, Chhabra A, Carrino JA. Second-opinion subspecialty consultations in musculoskeletal radiology. Am J Roentgenol. 2016;206:1217–21.
Eakins C, Ellis WD, Pruthi S, Johnson DP, Hernanz-Schulman M, Yu C, et al. Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. Am J Roentgenol. 2012;199:916–20.
Rozenberg A, Kenneally BE, Abraham JA, Strogus K, Roedl JB, Morrison WB, et al. Second opinions in orthopedic oncology imaging: can fellowship training reduce clinically significant discrepancies? Skeletal Radiol. 2019;48:143–7.
Rozenberg A, Kenneally BE, Abraham JA, Strogus K, Roedl JB, Morrison WB, et al. Clinical impact of second-opinion musculoskeletal subspecialty interpretations during a multidisciplinary orthopedic oncology conference. J Am Coll Radiol [Internet]. Elsevier Inc. 2017;14:931–6. https://doi.org/10.1016/j.jacr.2017.01.006.
Khoshpouri P, Khoshpouri P, Yousem K, Yousem DM. How do American radiology institutions deal with second opinion consultations on outside studies? Am J Roentgenol. 2020;214:144–8.
DiPiro PJ, van Sonnenberg E, Tumeh SS, Ros PR. Volume and impact of second-opinion consultations by radiologists at a tertiary care cancer center: Data. Acad Radiol. 2002;9:1430–3.
Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513–6.
Torok CM, Lee C, Nagy P, Yousem DM, Lewin JS. Neuroradiology second opinion consultation service: assessment of duplicative imaging. Am J Roentgenol. 2013;201:1096–100.
Loughrey GJ, Carrington BM, Anderson H, Dobson MJ, Lo Ying Ping F. The value of specialist oncological radiology review of cross-sectional imaging. Clin Radiol. 1999;54:149–54.
Wechsler RJ, Spettell CM, Kurtz AB, Lev-Toaff S, Halpern EJ, Nazarian LN, et al. Effects of training and experience in interpretation of emergency body CT scans’ computed tomography. Radiology. 1996;199:717–20.
Karmazyn B, Wanner MR, Marine MB, Tilmans L, Jennings SG, Hibbard RA. The added value of a second read by pediatric radiologists for outside skeletal surveys. Pediatr Radiol. 2019;49:203–9.
Borgstede JP, Lewis RS, Bhargavan M, Sunshine JH. RADPEER quality assurance program: a multifacility study of interpretive disagreement rates. J Am Coll Radiol. 2004;1:59–65.
Zafar HM, Chadalavada SC, Kahn CE, Cook TS, Sloan CE, Lalevic D, et al. Code abdomen: an assessment coding scheme for abdominal imaging findings possibly representing cancer. J Am Coll Radiol [Internet]. 2015;12:947–50. https://doi.org/10.1016/j.jacr.2015.04.005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review board (IRB) at our hospital and was performed in compliance with the Health Insurance Portability and Accountability Act (HIPAA).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bedoya, M.A., Chi, A.S., Harsha, A.K. et al. Musculoskeletal Outside Interpretation (MOI-RADS): an automated quality assurance tool to prospectively track discrepancies in second-opinion interpretations in musculoskeletal imaging. Skeletal Radiol 50, 723–730 (2021). https://doi.org/10.1007/s00256-020-03601-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03601-x