Abstract
Objective
To evaluate the frequency, clinico-pathologic and imaging features of malignant tumors in peripheral nerves which are of non-neurogenic origin (non-neurogenic peripheral nerve malignancy—PNM).
Materials and methods
We retrospectively reviewed our pathology database for malignant peripheral nerve tumors from 07/2014–07/2019 and performed a systematic review. Exclusion criteria were malignant peripheral nerve sheath tumor (MPNST). Clinico-pathologic and imaging features, apparent diffusion coefficient (ADCmin), and standard uptake values (SUVmax) are reported.
Results
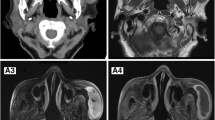
After exclusion of all neurogenic tumors (benign = 196, MPNST = 57), our search yielded 19 non-neurogenic PNMs (7%, n = 19/272), due to primary intraneural malignancy (16%, n = 3/19) and secondary perineural invasion from an adjacent malignancy (16%, n = 3/19) or metastatic disease (63%, n = 12/19). Non-neurogenic PNMs were located in the lumbosacral plexus/sciatic nerves (47%, n = 9/19), brachial plexus (32%, n = 6/19), femoral nerve (5%, n = 1/19), tibial nerve (5%, n = 1/19), ulnar nerve (5%, n = 1/19), and radial nerve (5%, n = 1/19). On MRI (n = 14/19), non-neurogenic PNM tended to be small (< 5 cm, n = 10/14), isointense to muscle on T1-W (n = 14/14), hyperintense on T2-WI (n = 12/14), with enhancement (n = 12/12), low ADCmin (0.5–0.7 × 10–3 mm2/s), and variable metabolic activity (SUVmax range 2.1–13.1). A target sign was absent (n = 14/14) and fascicular sign was rarely present (n = 3/14). Systematic review revealed 89 cases of non-neurogenic PNM.
Conclusion
Non-neurogenic PNMs account for 7% of PNT in our series and occur due to metastases and primary intraneural malignancy. Although non-neurogenic PNMs exhibit a non-specific MRI appearance, they lack typical signs of neurogenic tumors such as the target sign. Quantitative imaging features identified by DWI (low ADC) and F18-FDG PET/CT (high SUV) may be helpful clues to the diagnosis.






Similar content being viewed by others
References
Wilson TJ, Amrami KK, Howe BM, Spinner RJ. Clinical and radiological follow-up of intraneural perineuriomas. Neurosurgery. 2019;85(6):786–92.
Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999;19(5):1253–80.
Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 2005;102(2):246–55.
Ahlawat S, Fayad LM. Imaging cellularity in benign and malignant peripheral nerve sheath tumors: utility of the "target sign" by diffusion weighted imaging. Eur J Radiol. 2018;102:195–201.
Demehri S, Belzberg A, Blakeley J, Fayad LM. Conventional and functional MR imaging of peripheral nerve sheath tumors: initial experience. AJNR Am J Neuroradiol. 2014;35(8):1615–20.
Ahlawat S, Khandheria P, Del Grande F, Morelli J, Subhawong TK, Demehri S, et al. Interobserver variability of selective region-of-interest measurement protocols for quantitative diffusion weighted imaging in soft tissue masses: comparison with whole tumor volume measurements. J Magn Reson Imaging. 2016;43(2):446–54.
Treglia G, Taralli S, Bertagna F, Salsano M, Muoio B, Novellis P, et al. Usefulness of whole-body fluorine-18-fluorodeoxyglucose positron emission tomography in patients with neurofibromatosis type 1: a systematic review. Radiol Res Pract. 2012;2012:431029.
Kurtz KA, Hoffman HT, Zimmerman MB, Robinson RA. Perineural and vascular invasion in oral cavity squamous carcinoma: increased incidence on re-review of slides and by using immunohistochemical enhancement. Arch Pathol Lab Med. 2005;129(3):354–9.
Mendenhall WM, Amdur RJ, Williams LS, Mancuso AA, Stringer SP, Price MN. Carcinoma of the skin of the head and neck with perineural invasion. Head Neck. 2002;24(1):78–83.
Chang PC, Fischbein NJ, McCalmont TH, Kashani-Sabet M, Zettersten EM, Liu AY, et al. Perineural spread of malignant melanoma of the head and neck: clinical and imaging features. AJNR Am J Neuroradiol. 2004;25(1):5–11.
Maru N, Ohori M, Kattan MW, Scardino PT, Wheeler TM. Prognostic significance of the diameter of perineural invasion in radical prostatectomy specimens. Hum Pathol. 2001;32(8):828–33.
Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009;115(15):3379–91.
Capek S, Howe BM, Amrami KK, Spinner RJ. Perineural spread of pelvic malignancies to the lumbosacral plexus and beyond: clinical and imaging patterns. Neurosurg Focus. 2015;39(3):E14.
Marek T, Howe BM, Amrami KK, Spinner RJ. Perineural spread of nonmelanoma skin cancer to the brachial plexus: identifying anatomic pathway(s). World Neurosurg. 2018;114:e818–23.
Crush AB, Howe BM, Spinner RJ, Amrami KK, Hunt CH, Johnson GB, et al. Malignant involvement of the peripheral nervous system in patients with cancer: multimodality imaging and pathologic correlation. Radiographics. 2014;34(7):1987–2007.
Advani P, Paulus A, Murray P, Jiang L, Goff R, Pooley R, et al. A rare case of primary high-grade large B-cell lymphoma of the sciatic nerve. Clin Lymphoma Myeloma Leuk. 2015;15(6):e117–20.
Aghion DM, Capek S, Howe BM, Hepel JT, Sambandam S, Oyelese AA, et al. Perineural tumor spread of bladder cancer causing lumbosacral plexopathy: an anatomic explanation. Acta Neurochir. 2014;156(12):2331–6.
Alter RY, Wamsley CC, Mullen JT, Haile WZ, Goldsmith JD, Kasper EM. Peripheral nerve fibromyxoid sarcoma. J Neurosurg. 2014;121(3):576–9.
Babu MA, Spinner RJ, Dyck PJ, Amrami KK, Nathan MA, Kawashima A, et al. Recurrent prostatic adenocarcinoma with perineural spread to the lumbosacral plexus and sciatic nerve: comparing high resolution MRI with torso and endorectal coils and F-18 FDG and C-11 choline PET/CT. Abdom Imaging. 2013;38(5):1155–60.
Bang JS, Adsul N, Lim JH, Jang IT. Extra-osseous Ewing sarcoma of sciatic nerve masquerading as benign nerve sheath tumor and presented as lumbar radiculopathy: case report and review of literature. World Neurosurg. 2018;115:89–93.
Cabrilo I, Burkhardt K, Schaller K, Tessitore E. Renal carcinoma relapse presenting as a peripheral nerve sheath tumor: a case report and brief review of the literature. Neurochirurgie. 2013;59(3):128–32.
Candy N, Young A, Allinson K, Carr O, McMillen J, Trivedi R. Metastatic neuroendocrine carcinoma of unknown origin arising in the femoral nerve sheath. World Neurosurg. 2017;104:1047.e1041–6.
Capek S, Hebert-Blouin MN, Puffer RC, Martinoli C, Frick MA, Amrami KK, et al. Tumefactive appearance of peripheral nerve involvement in hematologic malignancies: a new imaging association. Skelet Radiol. 2015;44(7):1001–9.
Capek S, Howe BM, Tracy JA, Garcia JJ, Amrami KK, Spinner RJ. Prostate cancer with perineural spread and dural extension causing bilateral lumbosacral plexopathy: case report. J Neurosurg. 2015;122(4):778–83.
Capek S, Sullivan PS, Howe BM, Smyrk TC, Amrami KK, Spinner RJ, et al. Recurrent rectal cancer causing lumbosacral plexopathy with perineural spread to the spinal nerves and the sciatic nerve: an anatomic explanation. Clin Anat. 2015;28(1):136–43.
Daher A, Kamiya-Matsuoka C, Woodman K. Patient with 2 hematologic malignancies presenting as neurolymphomatosis. J Clin Neuromuscul Dis. 2018;19(3):124–30.
Del Grande A, Sabatelli M, Luigetti M, Conte A, Granata G, Rufini V, et al. Primary multifocal lymphoma of peripheral nervous system: case report and review of the literature. Muscle Nerve. 2014;50(6):1016–22.
Descamps MJ, Barrett L, Groves M, Yung L, Birch R, Murray NM, et al. Primary sciatic nerve lymphoma: a case report and review of the literature. J Neurol Neurosurg Psychiatry. 2006;77(9):1087–9.
Di Tommaso L, Magrini E, Consales A, Poppi M, Pasquinelli G, Dorji T, et al. Malignant granular cell tumor of the lateral femoral cutaneous nerve: report of a case with cytogenetic analysis. Hum Pathol. 2002;33(12):1237–40.
Green RA, O’Donnell P, Briggs TW, Tirabosco R. Two malignant peripheral nerve lesions of non-neurogenic origin. J Med Imaging Radiat Oncol. 2012;56(3):305–9.
Hebert-Blouin MN, Amrami KK, Myers RP, Hanna AS, Spinner RJ. Adenocarcinoma of the prostate involving the lumbosacral plexus: MRI evidence to support direct perineural spread. Acta Neurochir. 2010;152(9):1567–76.
Howe BM, Amrami KK, Nathan MA, Garcia JJ, Spinner RJ. Perineural spread of cervical cancer to the sciatic nerve. Skelet Radiol. 2013;42(11):1627–31.
Kahraman S, Sabuncuoglu H, Gunhan O, Gurses MA, Sirin S. A rare reason of foot drop caused by primary diffuse large b-cell lymphoma of the sciatic nerve: case report. Acta Neurochir. 2010;152(1):125–8.
Kichari JR, Hussain SM, Den Hollander JC, Krestin GP. MR imaging of the brachial plexus: current imaging sequences, normal findings, and findings in a spectrum of focal lesions with MR-pathologic correlation. Curr Probl Diagn Radiol. 2003;32(2):88–101.
Kosutic D, Gajanan K. Rare case of a liposarcoma in the brachial plexus. Ann R Coll Surg Engl. 2016;98(7):e106–8.
Ladha SS, Spinner RJ, Suarez GA, Amrami KK, Dyck PJ. Neoplastic lumbosacral radiculoplexopathy in prostate cancer by direct perineural spread: an unusual entity. Muscle Nerve. 2006;34(5):659–65.
Larque AB, Bredella MA, Nielsen GP, Chebib I. Synovial sarcoma mimicking benign peripheral nerve sheath tumor. Skelet Radiol. 2017;46(11):1463–8.
Lavorato A, Titolo P, Vincitorio F, Cofano F, Garbossa D. Intraneural Ewing sarcoma of fibular nerve: case report, radiologic findings and review of literature. World Neurosurg. 2019;123:212–5.
Lim AT, Clucas D, Khoo C, Parameswaran BK, Lau E. Neurolymphomatosis: MRI and (18) FDG-PET features. J Med Imaging Radiat Oncol. 2016;60(1):92–5.
Mathys J, Vajtai I, Vögelin E, Zimmermann DR, Ozdoba C, Hewer E. Desmoplastic small round cell tumor: a rare cause of a progressive brachial plexopathy. Muscle Nerve. 2014;49(6):922–7.
Mitchell BD, Fox BD, Viswanathan A, Mitchell AH, Powell SZ, Cech DA. Ewing sarcoma mimicking a peripheral nerve sheath tumor. J Clin Neurosci. 2010;17(10):1317–9.
Nagao E, Nishie A, Yoshimitsu K, Irie H, Shioyama Y, Naito S, et al. Gluteal muscular and sciatic nerve metastases in advanced urinary bladder carcinoma: case report. Abdom Imaging. 2004;29(5):619–22.
Oktay K, Guzel E, Bitiren M, Simsek S, Yildirim M, Guzel A. Lung adenocarcinoma metastasis mimicking peripheral nerve sheath tumor: case report and review of literature. World Neurosurg. 2018;120:490–4.
Quinones-Hinojosa A, Friedlander RM, Boyer PJ, Batchelor TT, Chiocca EA. Solitary sciatic nerve lymphoma as an initial manifestation of diffuse neurolymphomatosis. Case report and review of the literature. J Neurosurg. 2000;92(1):165–9.
Raveendran S, Kota AA, Stephen E, Pallapati SCR, Thomas BP. Synovial sarcoma of the brachial plexus - a rare tumor in a rare area: a case report. J Med Case Rep. 2018;12(1):334.
Reddy CG, Mauermann ML, Solomon BM, Ringler MD, Jerath NU, Begna KH, et al. Neuroleukemiosis: an unusual cause of peripheral neuropathy. Leuk Lymphoma. 2012;53(12):2405–11.
Scheithauer BW, Amrami KK, Folpe AL, Silva AI, Edgar MA, Woodruff JM, et al. Synovial sarcoma of nerve. Hum Pathol. 2011;42(4):568–77.
Schulz M, Lamont D, Muthu T, Hussain Z, Balakrishnan V. Metastasis of breast cancer to a lumbar spinal nerve root ganglion. Spine (Phila Pa 1976). 2009;34(20):E735–9.
Sideras PA, Matthews J, Sakib SM, Ofikwu F, Spektor V. Neurolymphomatosis of the peripheral nervous system: a case report and review of the literature. Clin Imaging. 2016;40(6):1253–6.
Song EJ, Park JS, Ryu KN, Park SY, Jin W. Perineural spread along spinal and obturator nerves in primary vaginal carcinoma: a case report. World Neurosurg. 2018;115:85–8.
Stone JJ, Adamo DA, Khan DZ, Packard AT, Broski SM, Nathan MA, et al. Multimodal imaging aids in the diagnosis of perineural spread of prostate cancer. World Neurosurg. 2019;122:e235–40.
Swanson AA, Giannini C, Folpe AL, Van Dyke DL, Amrami KK, Michalak WA, et al. Low-grade fibromyxoid sarcoma arising within the median nerve. Neuropathology. 2018;38(3):309–14.
Turgut M, Gokpinar D, Barutca S, Erkus M. Lumbosacral metastatic extradural Merkel cell carcinoma causing nerve root compression--case report. Neurol Med Chir (Tokyo). 2002;42(2):78–80.
Uchida K, Kobayashi S, Yayama T, Muramatsu J, Kurokawa T, Imamura Y, et al. Metastatic involvement of sacral nerve roots from uterine carcinoma: a case report. Spine J. 2008;8(5):849–52.
van den Bent MJ, de Bruin HG, Beun GD, Vecht CJ. Neurolymphomatosis of the median nerve. Neurology. 1995;45(7):1403–5.
van den Bent MJ, de Bruin HG, Bos GM, Brutel de la Riviere G, Sillevis Smitt PA. Negative sural nerve biopsy in neurolymphomatosis. J Neurol. 1999;246(12):1159–63.
Wang T, Miao Y, Meng Y, Li A. Isolated leukemic infiltration of peripheral nervous system. Muscle Nerve. 2015;51(2):290–3.
Wigfield CC, Hilton DA, Coleman MG, Whitfield PC. Metastatic adenocarcinoma masquerading as a solitary nerve sheath tumour. Br J Neurosurg. 2003;17(5):459–61.
Ye BS, Sunwoo IN, Suh BC, Park JP, Shim DS, Kim SM. Diffuse large B-cell lymphoma presenting as piriformis syndrome. Muscle Nerve. 2010;41(3):419–22.
Papachristou DJ, Palekar A, Surti U, Cieply K, McGough RL, Rao UN. Malignant granular cell tumor of the ulnar nerve with novel cytogenetic and molecular genetic findings. Cancer Genet Cytogenet. 2009;191(1):46–50.
Wasa J, Nishida Y, Tsukushi S, Shido Y, Sugiura H, Nakashima H, et al. MRI features in the differentiation of malignant peripheral nerve sheath tumors and neurofibromas. AJR Am J Roentgenol. 2010;194(6):1568–74.
DeVries AH, Howe BM, Spinner RJ, Broski SM. B-cell peripheral neurolymphomatosis: MRI and (18)F-FDG PET/CT imaging characteristics. Skelet Radiol. 2019;48(7):1043–50.
Mazal AT, Ashikyan O, Cheng J, Le LQ, Chhabra A. Diffusion-weighted imaging and diffusion tensor imaging as adjuncts to conventional MRI for the diagnosis and management of peripheral nerve sheath tumors: current perspectives and future directions. Eur Radiol. 2019;29(8):4123–32.
Bronstein Y, Tummala S, Rohren E. F-18 FDG PET/CT for detection of malignant involvement of peripheral nerves: case series and literature review. Clin Nucl Med. 2011;36(2):96–100.
Yuh EL, Jain Palrecha S, Lagemann GM, Kliot M, Weinstein PR, Barbaro NM, et al. Diffusivity measurements differentiate benign from malignant lesions in patients with peripheral neuropathy or plexopathy. AJNR Am J Neuroradiol. 2015;36(1):202–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shivani Ahlawat has received support from Department of Defense 2018–2023 and Pfizer (2017–2018). Laura M. Fayad has received support from GERRAF 2008–-10 and Siemens 2011–12. There is no conflict of interest.
Ethical approval
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Luna, R., Fayad, L.M., Rodriguez, F.J. et al. Imaging of non-neurogenic peripheral nerve malignancy—a case series and systematic review. Skeletal Radiol 50, 201–215 (2021). https://doi.org/10.1007/s00256-020-03556-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03556-z