Abstract
Objective
To analyze structural, longitudinal MRI findings during the development of accelerated knee osteoarthritis (AKOA) over 4 years.
Materials and methods
From the Osteoarthritis Initiative (OAI), knees with no radiographic osteoarthritis (KL 0/1) developing advanced-stage osteoarthritis (KL 3/4; AKOA) within a 4-year (y) timeframe were selected. MRIs were graded using the modified Whole-Organ Magnetic Resonance Imaging Score (WORMS) at the beginning of the 4-year timeframe (index visit), at 2-year, and 4-year follow-up. Morphological and clinical findings associated with KL 3/4 onset within 2 years compared to 4 years were assessed using generalized estimating equations.
Results
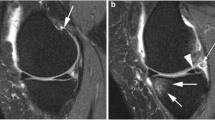
AKOA was found in 162 knees of 149 subjects (age 63.25 ± 8.3; 103 females; BMI 29.4 ± 3.9). Moderate to severe meniscal lesions WORMS ≥ 3 were present in 25% (41/162) at the index visit, 64% (104/162) at 2-year and 93% (151/162) at 4-year follow-up. Meniscal extrusion was the most prevalent finding (ranging from 18% at the index visit, 45% at 2-year and 94% at 4-year follow-up) and root tears were the most common types of tears (9% at the index visit; 22% at 2 years and 38% at 4 years). Risk factors associated with KL 3/4 onset within 2 years included root tears at the index visit (adjusted OR, 2.82; 95% CI: 1.33, 6.00; p = 0.007) and incident knee injury (42%, 49/116 vs. 24%, 11/46, p = 0.032).
Conclusions
Meniscal abnormalities, in particular extrusion and root tears, were the most prevalent morphological features found in subjects with AKOA. These results suggest that meniscal abnormalities have a significant role in accelerated progression of OA.



Similar content being viewed by others
References
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–96. https://doi.org/10.1016/S0140-6736(12)61729-2.
Driban JB, Eaton CB, Lo GH, Ward RJ, Lu B, McAlindon TE. Association of knee injuries with accelerated knee osteoarthritis progression: data from the osteoarthritis initiative. Arthritis Care Res. 2014;66(11):1673–9. https://doi.org/10.1002/acr.22359.
Driban JB, Stout AC, Lo GH, Eaton CB, Price LL, Lu B, et al. Best performing definition of accelerated knee osteoarthritis: data from the osteoarthritis initiative. Ther Adv Musculoskelet Dis. 2016;8(5):165–71. https://doi.org/10.1177/1759720X16658032.
Guermazi A, Hayashi D, Roemer FW, Niu J, Quinn EK, Crema MD, et al. Brief report: partial- and full-thickness focal cartilage defects contribute equally to development of new cartilage damage in knee osteoarthritis: the multicenter osteoarthritis study. Arthritis Rheumatol. 2017;69(3):560–4. https://doi.org/10.1002/art.39970.
Felson DT. Epidemiology of hip and knee osteoarthritis. Epidemiol Rev. 1988;10:1–28.
Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795–801. https://doi.org/10.1002/art.21724.
Roemer FW, Kwoh CK, Hannon MJ, Hunter DJ, Eckstein F, Grago J, et al. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol. 2017;27(1):404–13. https://doi.org/10.1007/s00330-016-4361-z.
Yau MS, Yerges-Armstrong LM, Liu Y, Lewis CE, Duggan DJ, Renner JB, et al. Genome-wide association study of radiographic knee osteoarthritis in north American Caucasians. Arthritis Rheumatol. 2017;69(2):343–51. https://doi.org/10.1002/art.39932.
Wang X, Blizzard L, Jin X, Chen Z, Zhu Z, Han W, et al. Quantitative assessment of knee effusion-synovitis in older adults: association with knee structural abnormalities. Arthritis Rheumatol. 2016;68(4):837–44. https://doi.org/10.1002/art.39526.
Kraus VB, Collins JE, Charles HC, Pieper CF, Whitley L, Losina E, et al. Predictive validity of radiographic trabecular bone texture in knee osteoarthritis: the osteoarthritis research society international/Foundation for the National Institutes of Health osteoarthritis biomarkers consortium. Arthritis Rheumatol. 2018;70(1):80–7. https://doi.org/10.1002/art.40348.
Davis JE, Liu SH, Lapane K, Harkey MS, Price LL, Lu B, et al. Adults with incident accelerated knee osteoarthritis are more likely to receive a knee replacement: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37(4):1115–8. https://doi.org/10.1007/s10067-018-4025-2.
Driban JB, Eaton CB, Lo GH, Price LL, Lu B, Barbe MF, et al. Overweight older adults, particularly after an injury, are at high risk for accelerated knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2016;35(4):1071–6. https://doi.org/10.1007/s10067-015-3152-2.
Driban JB, Price LL, Eaton CB, Lu B, Lo GH, Lapane KL, et al. Individuals with incident accelerated knee osteoarthritis have greater pain than those with common knee osteoarthritis progression: data from the osteoarthritis initiative. Clin Rheumatol. 2016;35(6):1565–71. https://doi.org/10.1007/s10067-015-3128-2.
Driban JB, Stout AC, Duryea J, Lo GH, Harvey WF, Price LL, et al. Coronal tibial slope is associated with accelerated knee osteoarthritis: data from the osteoarthritis initiative. BMC Musculoskelet Disord. 2016;17:299. https://doi.org/10.1186/s12891-016-1158-9.
Roemer FW, Hayes CW, Miller CG, Hoover K, Guermazi A. Imaging atlas for eligibility and on-study safety of potential knee adverse events in anti-NGF studies (part 1). Osteoarthr Cartil. 2015;23(Suppl 1):S22–42. https://doi.org/10.1016/j.joca.2014.09.015.
Hochberg MC. Serious joint-related adverse events in randomized controlled trials of anti-nerve growth factor monoclonal antibodies. Osteoarthr Cartil. 2015;23(Suppl 1):S18–21. https://doi.org/10.1016/j.joca.2014.10.005.
Hochberg MC, Tive LA, Abramson SB, Vignon E, Verburg KM, West CR, et al. When is osteonecrosis not osteonecrosis?: adjudication of reported serious adverse joint events in the Tanezumab clinical development program. Arthritis Rheumatol. 2016;68(2):382–91. https://doi.org/10.1002/art.39492.
Driban JB, Ward RJ, Eaton CB, Lo GH, Price LL, Lu B, et al. Meniscal extrusion or subchondral damage characterize incident accelerated osteoarthritis: data from the osteoarthritis initiative. Clin Anat. 2015;28(6):792–9. https://doi.org/10.1002/ca.22590.
Davis JE, Harkey MS, Ward RJ, Mackay JW, Lu B, Price LL, et al. Characterizing the distinct structural changes associated with self-reported knee injury among individuals with incident knee osteoarthritis: data from the osteoarthritis initiative. Clin Anat. 2018;31(3):330–4. https://doi.org/10.1002/ca.23054.
Roemer FW, Zhang Y, Niu J, Lynch JA, Crema MD, Marra MD, et al. Tibiofemoral joint osteoarthritis: risk factors for MR-depicted fast cartilage loss over a 30-month period in the multicenter osteoarthritis study. Radiology. 2009;252(3):772–80. https://doi.org/10.1148/radiol.2523082197.
Driban JB, Davis JE, Lu B, Price LL, Ward RJ, MacKay JW, et al. Accelerated knee osteoarthritis is characterized by destabilizing meniscal tears and pre-radiographic structural disease burden. Arthritis Rheumatol. 2018. https://doi.org/10.1002/art.40826.
Peterfy C, Li J, Zaim S, Duryea J, Lynch J, Miaux Y, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skelet Radiol. 2003;32(3):128–32. https://doi.org/10.1007/s00256-002-0603-z.
Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35(10):2047–54.
Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–62.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil. 2008;16(12):1433–41. https://doi.org/10.1016/j.joca.2008.06.016.
Rauscher I, Stahl R, Cheng J, Li X, Huber MB, Luke A, et al. Meniscal measurements of T1rho and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology. 2008;249(2):591–600. https://doi.org/10.1148/radiol.2492071870.
Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. https://doi.org/10.2214/ajr.183.1.1830017.
Plett SK, Hackney LA, Heilmeier U, Nardo L, Yu A, Zhang CA, et al. Femoral condyle insufficiency fractures: associated clinical and morphological findings and impact on outcome. Skelet Radiol. 2015;44(12):1785–94. https://doi.org/10.1007/s00256-015-2234-1.
Chanchek N, Gersing AS, Schwaiger BJ, Nevitt MC, Neumann J, Joseph GB, et al. Association of diabetes mellitus and biochemical knee cartilage composition assessed by T2 relaxation time measurements: data from the osteoarthritis initiative. J Magn Reson Imaging. 2017. https://doi.org/10.1002/jmri.25766.
Neumann J, Guimaraes JB, Heilmeier U, Joseph GB, Nevitt MC, McCulloch CE, et al. Diabetics show accelerated progression of knee cartilage and meniscal lesions: data from the osteoarthritis initiative. Skelet Radiol. 2018. https://doi.org/10.1007/s00256-018-3088-0.
Gersing AS, Schwaiger BJ, Heilmeier U, Joseph GB, Facchetti L, Kretzschmar M, et al. Evaluation of chondrocalcinosis and associated knee joint degeneration using MR imaging: data from the osteoarthritis initiative. Eur Radiol. 2017;27(6):2497–506. https://doi.org/10.1007/s00330-016-4608-8.
Bucknor MD, Nardo L, Joseph GB, Alizai H, Srikhum W, Nevitt MC, et al. Association of cartilage degeneration with four-year weight gain--3T MRI data from the osteoarthritis initiative. Osteoarthr Cartil. 2015;23(4):525–31. https://doi.org/10.1016/j.joca.2014.10.013.
Baum T, Joseph GB, Arulanandan A, Nardo L, Virayavanich W, Carballido-Gamio J, et al. Association of magnetic resonance imaging-based knee cartilage T2 measurements and focal knee lesions with knee pain: data from the osteoarthritis initiative. Arthritis Care Res. 2012;64(2):248–55. https://doi.org/10.1002/acr.20672.
Driban JB, McAlindon TE, Amin M, Price LL, Eaton CB, Davis JE, et al. Risk factors can classify individuals who develop accelerated knee osteoarthritis: data from the osteoarthritis initiative. J Orthop Res. 2017. https://doi.org/10.1002/jor.23675.
Davis JE, Price LL, Lo GH, Eaton CB, McAlindon TE, Lu B, et al. A single recent injury is a potent risk factor for the development of accelerated knee osteoarthritis: data from the osteoarthritis initiative. Rheumatol Int. 2017;37(10):1759–64. https://doi.org/10.1007/s00296-017-3802-6.
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–24. https://doi.org/10.1056/NEJMoa1305189.
Zikria B, Hafezi-Nejad N, Roemer FW, Guermazi A, Demehri S. Meniscal surgery: risk of radiographic joint space narrowing progression and subsequent knee replacement-data from the osteoarthritis initiative. Radiology. 2017;282(3):807–16. https://doi.org/10.1148/radiol.2016160092.
Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–92.
Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure–function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32(30):7411–31. https://doi.org/10.1016/j.biomaterials.2011.06.037.
Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556–63. https://doi.org/10.1136/ard.2004.023796.
Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A(1):4–9.
Guermazi A, Hayashi D, Jarraya M, Roemer FW, Zhang Y, Niu J, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268(3):814–21. https://doi.org/10.1148/radiol.13122544.
Carreau JH, Sitton SE, Bollier M. Medial meniscus root tear in the middle aged patient: a case based review. Iowa Orthop J. 2017;37:123–32.
Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–31. https://doi.org/10.2106/JBJS.G.00748.
Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025–32. https://doi.org/10.1016/j.arthro.2009.03.015.
Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–9. https://doi.org/10.1177/0363546508323254.
Crema MD, Roemer FW, Felson DT, Englund M, Wang K, Jarraya M, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the multicenter osteoarthritis study. Radiology. 2012;264(2):494–503. https://doi.org/10.1148/radiol.12110986.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502.
Maas O, Joseph GB, Sommer G, Wild D, Kretzschmar M. Association between cartilage degeneration and subchondral bone remodeling in patients with knee osteoarthritis comparing MRI and (99m)Tc-DPD-SPECT/CT. Osteoarthr Cartil. 2015;23(10):1713–20. https://doi.org/10.1016/j.joca.2015.05.014.
Draper CE, Quon A, Fredericson M, Besier TF, Delp SL, Beaupre GS, et al. Comparison of MRI and (1)(8)F-NaF PET/CT in patients with patellofemoral pain. J Magn Reson Imaging. 2012;36(4):928–32. https://doi.org/10.1002/jmri.23682.
Gilbertson EM. Development of periarticular osteophytes in experimentally induced osteoarthritis in the dog. A study using microradiographic, microangiographic, and fluorescent bone-labelling techniques. Ann Rheum Dis. 1975;34(1):12–25.
Blom AB, van Lent PL, Holthuysen AE, van der Kraan PM, Roth J, van Rooijen N, et al. Synovial lining macrophages mediate osteophyte formation during experimental osteoarthritis. Osteoarthr Cartil. 2004;12(8):627–35. https://doi.org/10.1016/j.joca.2004.03.003.
van der Kraan PM, van den Berg WB. Osteophytes: relevance and biology. Osteoarthr Cartil. 2007;15(3):237–44. https://doi.org/10.1016/j.joca.2006.11.006.
van Lent PL, Blom AB, van der Kraan P, Holthuysen AE, Vitters E, van Rooijen N, et al. Crucial role of synovial lining macrophages in the promotion of transforming growth factor beta-mediated osteophyte formation. Arthritis Rheum. 2004;50(1):103–11. https://doi.org/10.1002/art.11422.
Acknowledgements
The analyses in this study were funded through the NIH/NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases grants R01AR064771 and P50-AR060752). We would like to thank the participants and staff of the Coordinating Center of the OAI for their invaluable assistance with patient selection, statistical analysis, and technical support. The study was supported by the OAI, a public–private partnership comprising five NIH contracts (National Institute of Arthritis and Musculoskeletal and Skin Diseases contracts N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262), with research conducted by the OAI Study Investigators. The study was also funded in part by the Intramural Research Program of the National Institute on Aging, NIH. Private funding partners include Merck Research, Novartis Pharmaceuticals, GlaxoSmithKline, and Pfizer; the private sector funding for the OAI is managed by the Foundation for the National Institutes of Health.
Funding
The analyses in this study were funded through the NIH/NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases grants R01AR064771 and P50-AR06075).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Foreman, S.C., Neumann, J., Joseph, G.B. et al. Longitudinal MRI structural findings observed in accelerated knee osteoarthritis: data from the Osteoarthritis Initiative. Skeletal Radiol 48, 1949–1959 (2019). https://doi.org/10.1007/s00256-019-03242-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03242-9