Abstract
Objective
To determine the effect of needle position and foraminal stenosis on contrast flow directionality during CT-guided transforaminal epidural steroid injections (TFESI).
Materials and methods
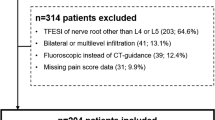
One hundred five consecutive CT-guided injections were performed in 68 patients (mean age, 65.5 years) from January 1 to December 31 2017, all with preceding MRI. Two readers independently reviewed CT images to assess needle position and to determine direction of contrast flow, which was defined as central or peripheral. The MRIs were independently reviewed by the readers to determine the degree of foraminal stenosis. Inter-reader agreement for both was evaluated with the kappa statistic. Analyses were performed to determine effect of needle position, degree of foraminal stenosis, and volume of contrast injected with directionality of contrast flow, and association between contrast flow directionality with immediate post-procedural pain scores.
Results
Central direction of contrast flow was demonstrated in 41/78 (52.6%) of cases with posterolateral needle position, and 20/27 (74.1%) with central or anteromedial needle position (p = 0.07). There was no difference in direction of contrast flow with high-grade versus absence of high-grade neuroforaminal narrowing, or with volume of contrast injected. There was no difference in immediate post-procedure pain scores regardless of contrast flow directionality.
Conclusions
Needle position is not significantly associated with contrast flow directionality during CT-guided TFESI, although there was a trend towards relatively decreased central flow with posterolateral positioning. Degree of foraminal stenosis and volume of injected contrast did not affect contrast flow directionality. There was no difference in immediate post-procedural pain scores with either direction of contrast flow.





Similar content being viewed by others
References
Boswell MV, Hansen HC, Trescot AM, Hirsch JA. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician. 2003;6(3):319–34.
Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003;6(1):3–81.
Ackerman WE, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104(5):1217–22. tables of contents
Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000;3(4):374–98.
Gupta R, Singh S, Kaur S, Singh K, Aujla K. Correlation between epidurographic contrast flow patterns and clinical effectiveness in chronic lumbar discogenic radicular pain treated with epidural steroid injections via different approaches. Korean J Pain. 2014;27(4):353–9.
Vassiliev D. Spread of contrast during L4 and L5 nerve root infiltration under fluoroscopic guidance. Pain Physician. 2007;10(3):461.
Furman MB, Lee TS, Mehta A, Simon JI, Cano WG. Contrast flow selectivity during transforaminal lumbosacral epidural steroid injections. Pain Physician. 2008;11(6):855–61.
Everett CR Shah RVSN. A systematic review of diagnostic utility of selective nerve root blocks. Pain Physician. 2005;8(2):225–34.
Datta S, Everett A, Trescot A, Schultz D, Adlaka R, et al. An updated systematic review of the diagnostic utility of selective nerve root blocks. Pain Physician. 2007;10(1):113–28.
Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004;83(5):378.
Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kang HS. Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology. 2007;245(2):584–90.
Pairuchvej S, Arirachakaran A, Keorochana G, Wattanapaiboon K, Atiprayoon S, Phatthanathitikarn P, et al. The short and midterm outcomes of lumbar transforaminal epidural injection with preganglionic and postganglionic approach in lumbosacral radiculopathy: a systematic review and meta-analysis. Neurosurg Rev. 2017;1-8.https://doi.org/10.1007/s10143-017-0826-z.
Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007;10(3):501–10.
Irwin A, Khan AL, Fender D, Sanderson PL, Gibson MJ. The role of needle tip position on the accuracy of diagnostic selective nerve root blocks in spinal deformity. Eur Spine J. 2014;23(1):33–9.
Wolff AP, Groen GJ, Wilder-Smith OH. Influence of needle position on lumbar segmental nerve root block selectivity. Reg Anesth Pain Med. 2006;31(6):523–30.
Mandell JC, Czuczman GJ, Gaviola GC, Ghazikhanian V, Cho CH. The lumbar neural foramen and transforaminal epidural steroid injections: an anatomic review with key safety considerations in planning the percutaneous approach. Am J Roentgenol. 2017;209(1):W26–35.
Pfirrmann CWA, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness—a study with patients and cadavers. Radiology. 2001;221(3):704–11.
Lee S, Lee JW, Yeom JS, Kim K-J, Kim H-J, Chung SK, et al. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010;194(4):1095–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011;12(6):864–70.
Stalcup ST, Crall TS, Gilula L, Riew KD. Influence of needle-tip position on the incidence of immediate complications in 2,217 selective lumbar nerve root blocks. Spine J. 2006;6(2):170–6.
Atluri S, Glaser SE, Shah RV, Sudarshan G. Needle position analysis in cases of paralysis from transforaminal epidurals: consider alternative approaches to traditional technique. Pain Physician. 2013;16(4):321–34.
Park JW, Nam H-S, Park Y. Usefulness of posterolateral transforaminal approach in lumbar radicular pain. Ann Rehabil Med. 2011;35(3):395–404.
Zhu J, Falco FJE, Formoso F, Onyewu O, Irwin FL. Alternative approach for lumbar transforaminal epidural steroid injections. Pain Physician. 2011;14(4):331–41.
Makkar JK, Singh NP, Rastogi R. Volume of contrast and selectivity for lumbar transforaminal epidural steroid injection. Pain Physician. 2015;18(1):101–5.
Castro WH, Grönemeyer D, Jerosch J, Seibel R, Lorenz G, Beutelstahl D, et al. How reliable is lumbar nerve root sheath infiltration? Eur Spine J. 1994;3(5):255–7.
Lee JW, Kim SH, Lee IS, Choi JA, Choi JY, Hong SH, et al. Therapeutic effect and outcome predictors of sciatica treated using transforaminal epidural steroid injection. Am J Roentgenol. 2006;187(6):1427–31.
Jeong YC, Lee CH, Kang S, Yoon JS. Contrast spread in the superoposterior approach of transforaminal epidural steroid injections for lumbosacral radiculopathy. Ann Rehabil Med. 2017;41(3):413–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Miskin, N., Gaviola, G.C., Ghazikhanian, V. et al. CT-guided transforaminal epidural steroid injections: do needle position and degree of foraminal stenosis affect the pattern of epidural flow?. Skeletal Radiol 47, 1615–1623 (2018). https://doi.org/10.1007/s00256-018-3002-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-018-3002-9