Abstract
Objective
To determine the benefits, risks, and limitations associated with wrapping a patient with lead shielding during fluoroscopy-guided kyphoplasty procedures as a way to reduce operator radiation exposure.
Materials and methods
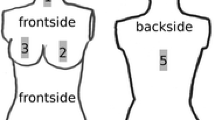
An anthropomorphic phantom was used to mimic a patient undergoing a kyphoplasty procedure under fluoroscopic guidance. Radiation measurements of the air kerma rate (AKR) were made at several locations and under various experimental conditions. First, AKR was measured at various angles along the horizontal plane of the phantom and at varying distances from the phantom, both with and without a lead apron wrapped around the lower portion of the phantom (referred to here as phantom shielding). Second, the effect of an operator’s apron was simulated by suspending a lead apron between the phantom and the measurement device. AKR was measured for the four shielding conditions—phantom shielding only, operator apron only, both phantom shielding and operator apron, and no shielding. Third, AKR measurements were made at various heights and with varying C-arm angle.
Results
At all locations, the phantom shielding provided no substantial protection beyond that provided by an operator’s own lead apron. Phantom shielding did not reduce AKR at a height comparable to that of an operator’s head.
Conclusions
Previous reports of using patient shielding to reduce operator exposure fail to consider the role of an operator’s own lead apron in radiation protection. For an operator wearing appropriate personal lead apparel, patient shielding provides no substantial reduction in operator dose.



Similar content being viewed by others
References
Choi HC. Fluoroscopic radiation exposure during percutaneous kyphoplasty. J Korean Neurosurg Soc. 2011;49:37–42.
Fitousi NT, Efstathopoulos EP, Delis HB, Kottou S, Kelekis AD, Panayiotakis GS. Patient and staff dosimetry in vertebroplasty. Spine. 2006;31(23):E887–9.
Hadelsberg UP, Harel R. Hazards of ionizing radiation and its impact on spine surgery. World Neurosurg. 2016;92:353–9.
Harstall R, Heini PF, Mini RL, et al. Radiation exposure to the surgeon during fluoroscopically assisted percutaneous vertebroplasty: A prospective study. Spine. 2005;30:1893–8.
Lonjon N, Le Corre M, Le Roy J, Greffier J, Fuentes S, Tonetti J, et al. Surgeon’s and patient’s radiation exposure through vertebral body cement augmentation procedures: A prospective multicentric study of 49 cases. World Neurosurg. 2016;93:371–6.
Luchs JS, Rosioreanu A, Gregorius D, Venkataramanan N, Koehler V, Ortiz AO. Radiation safety during spine interventions. JVIR. 2005;16(1):107–11.
Mroz TE, Yamashita T, Davros WJ, Lieberman IH. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech. 2008;21(2):96–100.
Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, et al. Radiation safety and spine surgery: Systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 2014;82(6):1337–43.
Von Wrangel A, Cederblad A, Rodriguez-Catarino M. Fluoroscopically guided percutaneous vertebroplasty: Assessment of radiation doses and implementation of procedural routines to reduce operator exposure. Acta Radiol. 2009;50(5):490–6.
Leake CB, Brinjikji W, Cloft HJ, Kallmes DF. Trends of inpatient spine augmentation: 2001-2008. Am J Neuroradiol. 2011;32(8):1464–8.
Theocharopoulos N, Perisinakis K, Damilakis J, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Occupational exposure from common fluoroscopic projections used in orthopaedic surgery. J Bone Joint Surg Am. 2003;85-A(9):1698–703.
Cloft HJ, Jensen ME. Kyphoplasty: An assessment of a new technology. Am J Neuroradiol. 2007;28(2):200–3.
National Council on Radiation Protection and Measurements. Radiation dose management for fluoroscopically-guided interventional medical procedures. NCRP Report No. 168. Bethesda, Maryland: National Council on Radiation Protection and Measurements.
Kruger R, Faciszewski T. Radiation dose reduction to medical staff during vertebroplasty: A review of techniques and methods to mitigate occupational dose. Spine. 2003;28:1608–13.
Lange HW, von Boetticher H. Reduction of operator radiation dose by a pelvic lead shield during cardiac catheterization by radial access. J Am Coll Cardiol Intv. 2012;5(4):445–9.
Performance Standards for Ionizing Radiation Emitting Products, 21 C.F.R. part 1020, sec.30 (h)(6) (2016).
Miller TR, Zhou J, Jindal G, Shivashankar R, Beaty N, Gandhi D. The efficacy of shielding systems for reducing operator exposure during neurointerventional procedures: A real-world prospective study. AJNR 2016 (epub ahead of print)
Marsh RM, Silosky M. Brain tumors, interventionalists, and radiation: How real is the risk? Endovascular Today. 2016;15(8):66–9.
Finkelstein MM. Is brain cancer an occupational disease of cardiologists? Can J Cardiol. 1998;14:1385–8.
Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013;111:1368–72.
Schueler BA. Operator shielding: How and why. Tech Vasc Interv Radiol. 2010;13(3):167–71.
Iqtidar AF, Jeon C, Rothman R, Snead R, Ryne CT. Reduction in operator radiation exposure during transradial catheterization and intervention using a simple lead drape. Am Heart J. 2013;165:293–8.
Murphy JC, Darragh K, Walsh SJ, Hanratty CG. Efficacy of the RADPAD protective drape during real world complex percutaneous coronary intervention procedures. Am J Cardiol. 2011;108:1408–10.
Musallam A, Volis I, Dadaev S, Abergel E, Soni A, Yalonetsky S, et al. A randomized study comparing the use of a pelvic lead shield during trans-radial interventions; threefold decrease in radiation to the operator but double exposure to the patient. Catheter Cardiovasc Interv. 2015;85(7):1164–70.
Politi L, Biondi-Zoccai G, Nocetti L, Costi T, Monopoli D, Rossi R, et al. Reduction of scatter radiation during transradial percutaneous coronary angiography: A randomized tiral using a lead-free radiation shield. Catheter Cardiovasc Interv. 2012;79:97–102.
Pasciak AS, Jones AK. Time to take the gloves off: The use of radiation reduction gloves can greatly increase patient dose. J Appl Clin Med Phys. 2014;15(6):351–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Smith, J.R., Marsh, R.M. & Silosky, M.S. Is lead shielding of patients necessary during fluoroscopic procedures? A study based on kyphoplasty. Skeletal Radiol 47, 37–43 (2018). https://doi.org/10.1007/s00256-017-2756-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2756-9