Abstract
Objective
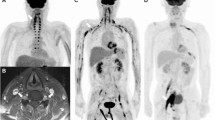
In neurolymphomatosis (NL), the affected nerves are typically described to be enlarged and hyperintense on T2W MR sequences and to avidly enhance on gadolinium-enhanced T1WI. This pattern is highly non-specific. We recently became aware of a “tumefactive pattern” of NL, neuroleukemiosis (NLK) and neuroplasmacytoma (NPLC), which we believe is exclusive to hematologic diseases affecting peripheral nerves.
Materials and methods
We defined a “tumefactive” appearance as complex, fusiform, hyperintense on T2WI, circumferential tumor masses encasing the involved peripheral nerves. The nerves appear to be infiltrated by the tumor. Both structures show varying levels of homogenous enhancement. We reviewed our series of 52 cases of NL in search of this pattern; two extra outside cases of NL, three cases of NLK, and one case of NPLC were added to the series.
Results
We identified 20 tumefactive lesions in 18 patients (14 NL, three NLK, one NPLC). The brachial plexus (n = 7) was most commonly affected, followed by the sciatic nerve (n = 6) and lumbosacral plexus (n = 3). Four patients had involvement of other nerves. All were proven by biopsy: the diagnosis was high-grade lymphoma (n = 12), low-grade lymphoma (n = 3), acute leukemia (n = 2), and plasmacytoma (n = 1).
Conclusions
We present a new imaging pattern of “tumefactive” neurolymphomatosis, neuroleukemiosis, or neuroplasmacytoma in a series of 18 cases. We believe this pattern is associated with hematologic diseases directly involving the peripheral nerves. Knowledge of this association can provide a clue to clinicians in establishing the correct diagnosis. Bearing in mind that tumefactive NL, NLK, and NPLC is a newly introduced imaging pattern, we still recommend to biopsy patients with suspicion of a malignancy.






Similar content being viewed by others
Abbreviations
- NL:
-
Neurolymphomatosis
- NLK:
-
Neuroleukemiosis
- NPLC:
-
Neuroplasmacytoma
- NHL:
-
Non-Hodgkin’s lymphoma
- DLBCL:
-
Diffuse large B-cell lymphoma
- MALT:
-
Mucosa-associated lymphatic tissue lymphoma
- LG BCL with PD:
-
Low-grade B-cell lymphoma with plasmacytic differentiation
- LPL:
-
Lymphoplasmacytic lymphoma
- NOS:
-
Not otherwise specified
- AML:
-
Acute myelogenous leukemia
- W:
-
Weakness
- N:
-
Numbness
- P:
-
Pain
- Par:
-
Paresthesias
- MM:
-
Multiple myeloma
- FDG:
-
18-fluorodeoxyglucose
- PET/CT:
-
Positron emission tomography/computed tomography
References
Grisariu S, Avni B, Batchelor TT, van den Bent MJ, Bokstein F, Schiff D, et al. Neurolymphomatosis: an International Primary CNS Lymphoma Collaborative Group report. Blood. 2010;115(24):5005–11.
Baehring JM, Damek D, Martin EC, Betensky RA, Hochberg FH. Neurolymphomatosis. Neuro Oncol. 2003;5(2):104–15.
Gan HK, Azad A, Cher L, Mitchell PL. Neurolymphomatosis: diagnosis, management, and outcomes in patients treated with rituximab. Neuro Oncol. 2010;12(2):212–5.
Yazawa S, Ohi T, Shiomi K, Takashima N, Kyoraku I, Nakazato M. Brachial plexus neurolymphomatosis: a discrepancy between electrophysiological and radiological findings. Intern Med. 2007;46(8):533–4.
Rosso SM, de Bruin HG, Wu KL, van den Bent MJ. Diagnosis of neurolymphomatosis with FDG PET. Neurology. 2006;67(4):722–3.
Rahmani M, Birouk N, Amarti A, Loukili Idrissi A, Marnissi F, Belaidi H, et al. T-cell lymphoma revealed by a mononeuritis multiplex: case report and review of literature. Rev Neurol (Paris). 2007;163(4):462–70.
Kim JH, Jang JH, Koh SB. A case of neurolymphomatosis involving cranial nerves: MRI and fusion PET-CT findings. J Neurooncol. 2006;80(2):209–10.
Reddy CG, Mauermann ML, Solomon BM, Ringler MD, Jerath NU, Begna KH, et al. Neuroleukemiosis: an unusual cause of peripheral neuropathy. Leuk Lymphoma. 2012;53(12):2405–11.
Mahan MA, Ladak A, Johnston PB, Seningen JL, Amrami KK, Spinner RJ. Unique occurrence of mucosa-associated lymphoid tissue lymphoma disseminated to peripheral nerves. J Surg Orthop Adv. 2013;22(4):321–5.
Hanna R, Di Primio GA, Schweitzer M, Torres C, Sheikh A, Chakraborty S. Progressive neurolymphomatosis with cutaneous disease: response in a patient with mycosis fungoides. Skelet Radiol. 2013;42(7):1011–5.
Agrawal S, Gi MT, Ng SB, Puhaindran ME, Singhania P. MRI and PET-CT in the diagnosis and follow-up of a lymphoma case with multifocal peripheral nerve involvement. Diagn Interv Radiol. 2013;19(1):25–8.
Kanamori M, Matsui H, Yudoh K. Solitary T-cell lymphoma of the sciatic nerve: case report. Neurosurgery. 1995;36(6):1203–5.
Baehring JM, Batchelor TT. Diagnosis and management of neurolymphomatosis. Cancer J. 2012;18(5):463–8.
Choi YJ, Shin JA, Kim YH, Cha SJ, Cho JY, Kang SH, et al. Neurolymphomatosis of brachial plexus in patients with non-Hodgkin's lymphoma. Case Rep Oncol Med. 2013;2013:492329.
Peruzzi P, Ray-Chaudhuri A, Slone WH, Mekhjian HS, Porcu P, Chiocca E. Reversal of neurological deficit after chemotherapy in BCL-6-positive neurolymphomatosis. Case report. J Neurosurg. 2009;111(2):247–51.
Roncaroli F, Poppi M, Riccioni L, Frank F. Primary non-Hodgkin's lymphoma of the sciatic nerve followed by localization in the central nervous system: case report and review of the literature. Neurosurgery. 1997;40(3):618–21. discussion 621–612.
Descamps MJ, Barrett L, Groves M, Yung L, Birch R, Murray NM, et al. Primary sciatic nerve lymphoma: a case report and review of the literature. J Neurol Neurosurg Psychiatry. 2006;77(9):1087–9.
Ye BS, Sunwoo IN, Suh BC, Park JP, Shim DS, Kim SM. Diffuse large B-cell lymphoma presenting as piriformis syndrome. Muscle Nerve. 2010;41(3):419–22.
Quinones-Hinojosa A, Friedlander RM, Boyer PJ, Batchelor TT, Chiocca EA. Solitary sciatic nerve lymphoma as an initial manifestation of diffuse neurolymphomatosis. Case report and review of the literature. J Neurosurg. 2000;92(1):165–9.
Eusebi V, Bondi A, Cancellieri A, Canedi L, Frizzera G. Primary malignant lymphoma of sciatic nerve. Report of a case. Am J Surg Pathol. 1990;14(9):881–5.
Wadhwa V, Thakkar RS, Maragakis N, Hoke A, Sumner CJ, Lloyd TE, et al. Sciatic nerve tumor and tumor-like lesions—uncommon pathologies. Skelet Radiol. 2012;41(7):763–74.
Suresh S, Saifuddin A, O'Donnell P. Lymphoma presenting as a musculoskeletal soft tissue mass: MRI findings in 24 cases. Eur Radiol. 2008;18(11):2628–34.
Wai JWC, Chan MK, Tang KW, Chan SCH. Neurogenic tumour mimicker: two cases of neurolymphomatosis. Hong Kong J Radiol. 2012;15:187–91.
Karam C, Khorsandi A, MacGowan DJ. Clinical reasoning: a 23-year-old woman with paresthesias and weakness. Neurology. 2009;72(2):e5–e10.
Warme B, Sullivan J, Tigrani DY, Fred DM. Chloroma of the forearm: a case report of leukemia recurrence presenting with compression neuropathy and tenosynovitis. Iowa Orthop J. 2009;29:114–6.
Bakst R, Jakubowski A, Yahalom J. Recurrent neurotropic chloroma: report of a case and review of the literature. Adv Hematol. 2011;2011:854240.
Lekos A, Katirji MB, Cohen ML, Weisman Jr R, Harik SI. Mononeuritis multiplex. A harbinger of acute leukemia in relapse. Arch Neurol. 1994;51(6):618–22.
Wang T, Miao Y, Meng Y, Li A. Isolated leukemic infiltration of peripheral nervous system. Muscle Nerve. 2015;51(2):290–93.
Zhu X-Y, Kuo S-H, Wan L-P, Liu Y, Wu Y-C. Isolated peripheral neuropathy as an unusual presentation for an extramedullary relapse of acute leukemia. Neurol Asia. 2014;19(2):203–6.
Hsu JH, Gordon C, Megason G, Majumdar S, Ostrenga A, Herrington B. A rare case of peripheral neuropathy from relapse of acute lymphoblastic leukemia to the brachial plexus. J Pediatr Hematol Oncol. 2012;34(2):e77–9.
Sui XF, Liu WY, Guo W, Xiao F, Yu X. Precursor B-cell lymphoblastic leukemia of the arm mimicking neurogenic tumor: case report. World J Surg Oncol. 2012;10:140.
Green RA, O'Donnell P, Briggs TW, Tirabosco R. Two malignant peripheral nerve lesions of non-neurogenic origin. J Med Imaging Radiat Oncol. 2012;56(3):305–9.
Okamoto Y, Minami M, Tohno E, Anno I, Kunimatshu A, Ueda T. Multifocal peripheral nerve involvement associated with multiple myeloma. Skelet Radiol. 2007;36(12):1191–3.
Misdraji J, Ino Y, Louis DN, Rosenberg AE, Chiocca EA, Harris NL. Primary lymphoma of peripheral nerve: report of four cases. Am J Surg Pathol. 2000;24(9):1257–65.
Kanda T. Biology of the blood–nerve barrier and its alteration in immune mediated neuropathies. J Neurol Neurosurg Psychiatry. 2013;84(2):208–12.
Franco CD. Connective tissues associated with peripheral nerves. Reg Anesth Pain Med. 2012;37(4):363–5.
Kim J, Kim YS, Lee EJ, Kang CS, Shim SI. Primary CD56-positive NK/T-cell lymphoma of median nerve: a case report. J Korean Med Sci. 1998;13(3):331–3.
Stuart JE, Smith AC. Plasmacytoma of the superficial radial nerve. J Hand Surg [Am]. 2001;26(4):776–80.
Acknowledgments
S.C. is supported by European Regional Development Fund - Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123). We thank Dr. Brian P. O’Neill for the wisdom he shared with us during numerous consultations.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Declaration
An approval from the institutional review board was obtained before the conduct of the study. The patients have consented to the inclusion in the study. This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000 and 2009.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Capek, S., Hébert-Blouin, MN., Puffer, R.C. et al. Tumefactive appearance of peripheral nerve involvement in hematologic malignancies: a new imaging association. Skeletal Radiol 44, 1001–1009 (2015). https://doi.org/10.1007/s00256-015-2151-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2151-3