Abstract
Objective
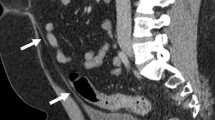
Glomuvenous malformation (GVM) is an inherited autosomal dominant trait. The lesions, which appear as bluish nodules or plaque-like cutaneous elevations, are usually tender and more firm than sporadic venous malformations. Conventionally, the lesions are thought to be limited to the cutaneous and subcutaneous tissue planes. The objective was to characterize the depth of involvement of GVM lesions.
Materials and Methods
Magnetic resonance imaging (MRI) findings in GVM were retrospectively evaluated by two radiologists. The signal characteristics, tissue distribution, pattern of contrast enhancement of the lesions in GVM were documented.
Results
Thirty patients (19 female) aged 1–35 years (mean 18 years) were diagnosed with GVM based on clinical features (n = 20) and/or histopathological findings (n = 10). The lesions were present in the lower extremity (n = 15), upper extremity (n = 6), cervico-facial region (n = 6), pelvis (n = 2), and chest wall (n = 1). All patients had skin and subcutaneous lesions. Fifty percent of the patients (n = 15) demonstrated subfascial intramuscular (n = 15), intra-osseous (n = 1), and intra-articular involvement (n = 1).
Conclusion
Contrary to the conventional belief that GVMs are generally limited to the skin and subcutaneous tissue, deep subfascial extension of the lesions is common.


Similar content being viewed by others
References
Brouillard P, Boon LM, Mulliken JB, Enjolras O, Ghassibe M, Warman ML, et al. Mutations in a novel factor, glomulin, are responsible for glomuvenous malformations (“glomangiomas”). Am J Hum Genet. 2002;70(4):866–74.
Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Arch Dermatol. 2004;140(8):971–6.
Vercellino N, Nozza P, Oddone M, Bava GL. Large plaque-like glomuvenous malformation (glomangioma) simulating venous malformation. Clin Exp Dermatol. 2006;31(4):538–41.
Mallory SB, Enjolras O, Boon LM, Rogers E, Berk DR, Blei F, et al. Congenital plaque-type glomuvenous malformations presenting in childhood. Arch Dermatol. 2006;142(7):892–6.
Dompmartin A, Vikkula M, Boon LM. Venous malformation: update on aetiopathogenesis, diagnosis and management. Phlebology. 2010;25(5):224–35.
Berenguer B, Burrows PE, Zurakowski D, Mulliken JB. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg. 1999;104(1):1–11; discussion 12–15.
Conflict of interest
No conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaikh, R., Alomari, A.I., Mulliken, J.B. et al. Subfascial involvement in glomuvenous malformation. Skeletal Radiol 43, 895–897 (2014). https://doi.org/10.1007/s00256-014-1836-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-1836-3