Abstract
Objective
Tibial spiking (i.e., spurring of tibial spines), eburnation, and osteophytes are considered features of osteoarthritis. This investigation employed direct inspection of the medial and lateral tibial plateaus in paleopathological specimens to analyze the frequency and morphological features of osteoarthritis and to define any relationship between the size of osteophytes and that of the intercondylar tibial spines.
Materials and Methods
A total of 35 tibial bone specimens were evaluated for the degree of osteoarthritis and presence of eburnation. Each plateau was also divided into four quadrants and the presence and size of bone outgrowths were recorded in each quadrant. The “medial/lateral tibial intercondylar spine index” for each specimen was calculated as follows: (medial/lateral intercondylar tibial spine height)/(anteroposterior width of the superior tibial surface). The relationships between medial and lateral tibial height indexes with the degree of osteoarthritis were then tested.
Results
Osteophytes were observed more frequently in the anterior quadrants of both tibial plateaus than in the posterior quadrants (29 vs 16 for the medial tibial plateau [p = 0.01] and 28 vs 20 for the lateral tibial plateau [p = 0.04]). Eburnation was seen more frequently in the posterior regions of both tibial plateaus than in the anterior regions (17 vs 5, p < 0.01). In specimens with no signs of osteoarthritis the lateral intercondylar tibial index was significantly lower than that in specimens with some degree of osteoarthritis (p = 0.02). The medial intercondylar tibial index of the specimens with no signs of osteoarthritis was not significantly different from that of the specimens with some degree of osteoarthritis (p = 0.45). There was a positive correlation between the lateral spine height index and the overall grading of osteoarthritis, (r = 0.6, p < 0.01). In the anteromedial and posteromedial quadrants of the lateral tibial plateau, the association between the lateral intercondylar tibial spine index and the grade of osteophytes was 0.5 (p < 0.01) and 0.7 (p < 0.01) respectively.
Conclusion
Spiking of the lateral tibial intercondylar spine is associated with osteophyte formation and osteoarthritis. Eburnation occurs mainly in the posterior parts of the tibial plateaus while osteophytes arise mainly in the anterior parts. These findings suggest that stresses occurring in the flexed knee may contribute to many of the morphological abnormalities of osteoarthritis.
Similar content being viewed by others
Introduction
Osteoarthritis is a degenerative disease that involves articular cartilage and targets certain joints such as the knee. Radiographic findings of osteoarthritis include joint space narrowing, marginal osteophytes, bone cysts and subchondral bone sclerosis, and the absence of bone atrophy [1]. Osteophytes are formed in response to abnormal stresses at the joint margins; however, other factors such as genetic susceptibility and systemic predisposition may also contribute to their formation [2]. Conventional radiography is the most widely accepted modality for the detection of osteoarthritis, especially for epidemiological purposes. Indeed, the generally accepted classification system that grades the radiographic severity of osteoarthritis was introduced by Kellgren and Lawrence in 1957 [3], and their grading system emphasizes the presence and size of the osteophytes along with joint space narrowing. Radiographs, however, are generally inadequate in assessing the occurrence and characteristics of small osteophytes and enthesophytes (Figs. 1, 2) [4]. One of the radiographic features employed for the detection of osteoarthritis is tibial “spiking.” Indeed, tibial spiking (i.e., spurring of tibial spines) is reported as a reliable marker in the detection of early osteoarthritis [5–7]. However, the reliability of this finding as a feature of an early stage of osteoarthritis is not clear since tibial spiking is also evident in cases of well-established osteoarthritis [7]. Compared with radiography, direct physical inspection of bone allows more accurate analysis of the presence, site and characteristics of surface irregularities, and excrescences [8, 9]. This investigation employed direct inspection of the medial and lateral tibial plateaus in paleopathological specimens to analyze the frequency and morphological features of surface bone excrescences and to define any relationship between the size of osteophytes and that of the intercondylar tibial spines.
Photograph of the superior surface of the left tibia showing four quadrants in each plateau. Each quadrant was named with respect to the sagittal and coronal planes of the body. Also note two marginal beak-like osteophytes (grade 1) in the medial and lateral plateaus (arrows). MED medial plateau, LAT lateral plateau, AM anteromedial, AL anterolateral, PM posteromedial, PL posterolateral
Materials and methods
A total of 44 well preserved, skeletally mature tibial specimens from the collection of a local museum were initially analyzed. Most of the bones had their origin in the early to mid-1900s. Information regarding the gender, occupation, or age at death was available for only a few specimens. Five of these bone specimens were then excluded from the study due to severe deformity or artifacts. Eight of the specimens were in pairs (i.e., right and left tibiae). To minimize any bias produced by similarity between right and left knees in these paired specimens, only one tibial specimen was randomly chosen from each pair for further assessment and the other was excluded from the analysis [10]. Therefore, a total of 35 tibial bone specimens were evaluated. Each tibial plateau was divided into four quadrants of a circle. Each quadrant was named with respect to its position relative to the sagittal and coronal planes of the body. One of the observers (M.H.), a medical doctor, who had prior experience in the inspection of paleopathological specimens [11] assessed the four quadrants, (i.e., anteromedial, anterolateral, posteromedial, and posterolateral) by visual and tactile observation for the presence or absence of outgrowths (Figs. 1, 3). The outgrowths were classified on a continuous scale of 0 to 3 (0 = no outgrowth, 1 = small beak-like outgrowth, 3 = large (≥2 mm) or mushroom-like outgrowth, and 2 = outgrowth between grades 1 and 3). If there was more than one outgrowth (with different grades) in a single quadrant, the highest grade was recorded. Thus, in quadrants with multiple outgrowths of different grades, only one osteophyte grade per quadrant was recorded. The height of the medial and lateral intercondylar tibial spines was also measured, calculated from the tip of the spine to its base at the intercondylar surface using a caliper. All the measurements were expressed in millimeters. Measured values were then normalized in view of the difference in the size of the tibial specimens. The anteroposterior width of the superior tibial surface, in the midline, was also measured in each specimen. Therefore, the “medial/lateral tibial intercondylar spine index” for each specimen was calculated as follows:
The presence of eburnation (i.e., polished, ivory-like bone surface), porosity (i.e., decreased bone density) of the tibial plateaus, and bone cysts (i.e., presence of intraosseous cavities) were also recorded by visual observation of the tibial plateaus. The severity of osteoarthritis of each specimen was judged on the basis of a global assessment of all expected abnormalities: osteophytosis, eburnation, and cysts. Each specimen was then classified on a scale of 0 to 3 (0 = no findings, 1 = minimal findings, 2 = moderate findings, and 3 = severe findings). A total of 15 specimens were re-assessed randomly 3 weeks after the first observation period by the same observer to evaluate the reproducibility of the data.
The Spearman’s rank correlation coefficient, t test and Chi-squared tests were used for further analysis of this study when needed. Kappa and Kappa weighted coefficients were used to express the inter-rater agreement and reproducibility of the data. All p values were two-tailed and a p value less than 0.05 was considered significant. SPSS 16.0 was utilized for statistical analyses (SPSS, Chicago, IL, USA).
Results
Of the 35 assessed specimens, 49% (n = 17) were right tibiae and 51% (n = 18) were left tibiae. No significant differences were observed between the quadrants of the tibial plateaus as far as the presence of osteophytes (p = 0.09) were concerned. However, when quadrants were combined and the data further analyzed, osteophytes were observed more frequently in the anterior quadrants of both tibial plateaus than in the posterior quadrants (29 vs 16 for the medial tibial plateau [p = 0.01] and 28 vs 20 for the lateral tibial plateau [p = 0.04]). The detailed distribution of osteophytes and their grades in each quadrant of the tibial plateaus are shown in Table 1.
Kappa weighted values for reproducibility of the measurements were as follows: for grading of osteophytes in the medial and lateral tibial plateaus Kappa weighted values were 0.85 and 0.80 respectively. Kappa values for the medial and lateral intercondylar tibial index were 0.91 and 0.88 respectively. The Kappa value for the global assessment of osteoarthritis was 0.86.
In the overall grading of osteoarthritis, 28.6% (n = 10) of the specimens had no sign of osteoarthritis. Low grade osteoarthritis (grade 1) was observed in 28.6% (n = 10) of the specimens. Intermediate osteoarthritis (grade 2) and severe osteoarthritis (grade 3) were identified in 14.2% (n = 5) and 28.6% (n = 10) of the specimens respectively.
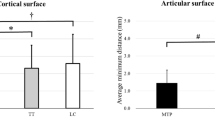
Eburnation was observed more frequently in the posterior parts the tibial plateaus than in the anterior parts (17 vs 5, p < 0.01) .The mean heights of the medial and lateral intercondylar tibial spines were 2.63 mm (range: 1–10 mm) and 2.47 mm (range: 1–6 mm) respectively. The mean anteroposterior width of the tibial plateau was 51.18 (range: 44–61 mm). In specimens with no signs of osteoarthritis (i.e., the global grading = 0) the lateral intercondylar tibial index was significantly lower than that in specimens with some degree of osteoarthritis (9.2 vs 17.8, p = 0.02). However, the medial intercondylar tibial index of the specimens with no signs of osteoarthritis was not significantly different from that of the specimens with some degree of osteoarthritis (12.1 vs 14.7, p = 0.45). There was a statistically significant positive correlation between the lateral spine height index and the overall grading of osteoarthritis (r = 0.6, p < 0.01). The association between the medial intercondylar tibial spine index and the overall grading of osteoarthritis was not significant (r = 0.2, p = 0.29).
In the anteromedial quadrant of the lateral tibial plateau, the association between the lateral intercondylar tibial spine index and the grade of osteophytes was 0.5 (p < 0.01). In the posteromedial quadrant of the lateral tibial plateau, the association between the lateral intercondylar tibial spine index and the grade of osteophytes was 0.7 (p < 0.01).
No association was found between the grade of osteophytes in the anterolateral or posterolateral quadrants of the lateral tibial plateau with the lateral tibial spine index. There was no significant association between the medial tibial spine index with the grade of osteophytes in any of the quadrants of the medial tibial plateau. The correlation between the grade of osteophytes in different quadrants of the medial and lateral tibial plateaus and the medial and lateral intercondylar tibial index is shown in Table 2.
Discussion
In this study osteophytes were more frequently observed in anterior quadrants and eburnation was more common in posterior quadrants of the tibial plateaus. Eburnation and increased bone density typically occur in regions where the articular cartilage is lost. In comparison, chondrogenesis and enchondral ossification in response to abnormal stresses on the articular surface are responsible for osteophyte formation [12, 13]. Thus, osteophytes develop in regions of the joint that still possess some articular cartilage. Cartilage loss and subsequent sclerosis and eburnation of the posterior regions of the tibial plateaus may relate, at least in part, to backward sliding of the femoral condyles during knee flexion, which would lead to greater compression of the posterior tibial cartilage, leading to cartilage loss. Relative preservation of articular cartilage is a possible reason for more frequent osteophyte formation in the anterior quadrants of the tibial plateaus. Capsular traction during knee flexion may lead to tensile stress in the anterior tibial margin and subsequent enthesophyte formation as well.
In a study of 55 patients with marked signs of osteoarthritis, Reiff et al. [7] showed that, compared with controls, the patients with marked osteoarthritis had significantly higher intercondylar spine height. They concluded that intercondylar spine height can be considered a sign of osteoarthritis. In our study, the association between the intercondylar spine indexes and the global grading of osteoarthritis was significant only for the lateral intercondylar spine and not for the medial intercondylar spine. Furthermore, the lateral spine height index correlated only with the grade of osteophytes arising in the medial quadrants in the lateral tibial plateau (i.e., anteromedial and posteromedial quadrants); no correlation was found between the medial intercondylar spine index and changes in any of the quadrants of the medial tibial plateau. In osteoarthritis of the knee, the medial compartment is ten times more frequently involved than the lateral compartment, leading to varus deformity [14, 15]. The lateral tibial spine is in close contact with the anterior and posterior horns of the lateral meniscus. It is also adjacent to other structures such as fibers from the anterior cruciate ligament as well as certain meniscofemoral ligaments [16–19]. Tensile forces on some of the above-mentioned structures may increase varus deformity and could explain the formation of bony outgrowths on or near the lateral tibial spine. Although Donnelly et al. [20], in a study of 1,003 women, reported a positive association between medial and lateral tibial intercondylar spine height and medial and lateral osteophytes, their study did not confirm that isolated tibial spiking is a reliable marker for the presence of osteoarthritis of the knee. They concluded that tibial spiking should not routinely be reported as a sign of early osteoarthritis. These investigators found that intercondylar spine angulations (i.e,. angulation of the tip of the medial and lateral intercondylar spines) had a higher association than intercondylar spine height with regard to tibial osteophytes.
Advanced age is considered one of the risk factors for osteophyte formation [21]. Our specimens were derived from an older population and osteophytes of different grades existed in the majority of the specimens, introducing a selection bias. Further, clinical information was not available and the significance of these observed osteophytes (e.g., grade 1) remains a question whose answer will require further studies. Another weakness of our study was the unavailability of the corresponding femurs so we could not evaluate coexistent morphological changes in the femur and the role of femorotibial alignment [22, 23]. Finally, only one observer analyzed all of the specimens although he did so twice for some of the specimens. This observer had prior experience in the inspection of paleopathological specimens and the repeatability of his assessments was high.
In conclusion, our study suggests that spiking of the lateral tibial intercondylar spine is associated with osteophyte formation and osteoarthritis. Further studies with case control groups are required for a more comprehensive understanding of the role of the intercondylar spines as a marker of early and/or late osteoarthritis. Our study also suggests that eburnation (i.e., increased bone density) as a sign of osteoarthritis occurs mainly in the posterior parts of the tibial plateaus, while osteophytes arise mainly in the anterior parts. These findings suggest that stresses occurring in the flexed knee may contribute to many of the morphological abnormalities of osteoarthritis.
References
Jaffe HL. Metabolic, degenerative and inflammatory diseases of bones and joint. Philadelphia: Lea & Febiger; 1972. p. 735–78.
Rogers J, Shepstone L, Dieppe P. Bone formers: osteophyte and enthesophyte formation are positively associated. Ann Rheum Dis. 1997;56(2):85–90.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Rogers J, Watt I, Dieppe P. Comparison of visual and radiographic detection of bony changes at the knee joint. Br Med J. 1990;300:367–8.
Sutton D. A textbook of radiology and imaging. 4th ed. Edinburgh: Churchill Livingstone; 1987. p. 113.
Resnick D, Niwayama G. Diagnosis of bone and joint disorders. 2nd ed. Philadelphia: Saunders; 1988. p. 1448.
Reiff DB, Heron CW, Stoker DJ. Spiking of the tubercles of the intercondylar eminence of the tibial plateau in osteoarthritis. Br J Radiol. 1991;64:915–7.
Esposito A, Souto SC, Catalano OA, Doria AS, Trigo PB, Resnick D. Pattern of osteophytes and enthesophytes in the proximal ulna: an anatomic, paleopathologic, and radiologic study. Skeletal Radiol. 2006;35(11):847–56.
Rogers J, Shepstone L, Dieppe P. Bone formers: osteophyte and enthesophyte formation are positively associated. Ann Rheum Dis. 1997;56(2):85–90.
Zhang Y, Glynn RJ, Felson DT. Musculoskeletal disease research: should we analyze the joint or the person? J Rheumatol. 1996;23(7):1130–4.
Hayeri MR, Trudell DJ, Resnick D. Anterior ankle impingement and talar bony outgrowths: osteophyte or enthesophyte? Paleopathologic and cadaveric study with imaging correlation. AJR Am J Roentgenol. 2009;193(4):W334–8.
Moskowitz RW, Goldberg VM. Studies of osteophyte pathogenesis in experimentally induced osteoarthritis. J Rheumatol. 1987;14(2):311–20.
Van der Kraan PM, van den Berg WB. Osteophytes: relevance and biology. Osteoarthritis Cartilage. 2007;15(3):237–44.
Ahlback S. Osteoarthritis of the knee: a radiographic investigation. Acta Radiol. 1968;277(1):7–72.
Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632–6.
Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy. 1995;11(4):386–94.
Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–31.
Arnoczky SP. Anatomy of the anterior cruciate ligament. Clin Orthop Relat Res. 1983;172:19–25.
Wan ACT, Felle P. The menisco-femoral ligaments. Clin Anat. 1995;8:323.
Donnelly S, Hart DJ, Doyle DV, Spector TD. Spiking of the tibial tubercles—a radiological feature of osteoarthritis? Ann Rheum Dis. 1996;55(2):105–8.
Hernborg J, Nilsson BE. Age and sex incidence of osteophytes in the knee joint. Acta Orthop Scand. 1973;44(1):66–8.
Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–95.
Wada M, Tatsuo H, Baba H, Asamoto K, Nojyo Y. Femoral intercondylar notch measurements in osteoarthritic knees. Rheumatology. 1999;38:554–8.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00256-010-0908-2
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Hayeri, M.R., Shiehmorteza, M., Trudell, D.J. et al. Proximal tibial osteophytes and their relationship with the height of the tibial spines of the intercondylar eminence: paleopathological study. Skeletal Radiol 39, 877–881 (2010). https://doi.org/10.1007/s00256-009-0838-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-009-0838-z