Abstract
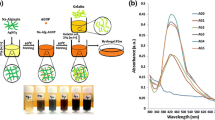
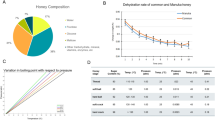
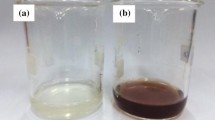
Novel alginate hydrogels with silver nanoparticles (AgNPs) and honey components were produced with the aim to target multidrug-resistant bacterial strains causing nosocomial wound infections. AgNP synthesis was optimized in highly concentrated honey solutions so that a 5-month stable, colloid solution with 50% of honey and ~ 8 nm AgNPs at neutral pH was obtained. The colloid solution was further used to produce nano-composite Ag/alginate hydrogels in different forms (microbeads, microfibers and discs) that retained all AgNPs and high fractions of honey components (40–60%) as determined by the phenol–sulfuric acid and Folin-Ciocalteu methods. The hydrogels were characterized by UV–Vis spectroscopy and Fourier-transform infrared-attenuated total reflectance spectroscopy while the antibacterial activity was investigated against a broad spectrum of Gram-negative and Gram-positive bacteria, including 13 multi-resistant clinical strains of Acinetobacter baumannii, one clinical strain of Pseudomonas aeruginosa and one clinical strain of Staphylococcus aureus. At the total released silver concentration of ~ 9 μg/ml, the hydrogels exhibited strong bactericidal activity against standard and most of the investigated multi-resistant hospital strains with the exemption of 3 clinical strains of A. baumannii in which antibacterial effects were absent. These results reveal the need for further in-depth studies of bacterial resistance mechanisms and, in the same time, potentials of the novel Ag/alginate hydrogels with honey components to combat wound infections and enhance healing as non-sticky, antibacterial, and bioactive dressings.








Similar content being viewed by others
Data availability
Data not available/data will be made available on request.
References
Alam F, Islam MA, Gan SH, Khalil MI (2014) Honey: a potential therapeutic agent for managing diabetic wounds. Evid Based Complement Alternat Med 2014:1–16. https://doi.org/10.1155/2014/169130
Al-Dhabi NA, Mohammed Ghilan AK, Arasu MV (2018) Characterization of silver nanomaterials derived from marine Streptomyces sp. Al-Dhabi-87 and its in vitro application against multidrug resistant and extended-spectrum beta-lactamase clinical pathogens. Nanomaterials 8:1–13. https://doi.org/10.3390/nano8050279
Armentano I, Dottori M, Fortunati E, Mattioli S, Kenny JM (2010) Biodegradable polymer matrix nanocomposites for tissue engineering: a review. Polym Degrad Stab 95:2126–2146. https://doi.org/10.1016/j.polymdegradstab.2010.06.007
Bhattacharya R, Mukherjee P (2008) Biological properties of “naked” metal nanoparticles. Adv Drug Deliv Rev 60:1289–1306. https://doi.org/10.1016/j.addr.2008.03.013
Bogdan M, Drenjancevic D, Harsanji Drenjancevic I, Bedenic B, Zujic Atalic V, Talapko J, Vukovic D (2018) In vitro effect of subminimal inhibitory concentrations of antibiotics on the biofilm formation ability of Acinetobacter baumannii clinical isolates. J Chemother 30:16–24. https://doi.org/10.1080/1120009X.2017.1378835
Bowler PG, Duerden BI, Armstrong DG (2001) Wound microbiology and associated approaches to wound management. Clin Microbiol Rev 14:244–269. https://doi.org/10.1128/CMR.14.2.244-269.2001
Cai B, Echols R, Magee G, Arjona Ferreira JK, Morgan G, Ariyasu M, Sawada T, Nagata TD (2017) Prevalence of carbapenem-resistant gram-negative infections in the United States predominated by Acinetobacter baumannii and Pseudomonas aeruginosa. Open Forum Infect Dis 4:1–7. https://doi.org/10.1093/ofid/ofx176
Cavassin ED, de Figueiredo LFP, Otoch JP, Martins Seckler M, de Oliveira RA, Fantinelli Franco F, Spolon Marangoni V, Zucolotto V, Shafferman Levin AS, Figueiredo Costa S (2015) Comparison of methods to detect the in vitro activity of silver nanoparticles (AgNP) against multidrug resistant bacteria. J Nanobiotechnol 13:1–16. https://doi.org/10.1186/s12951-015-0120-6
Dakal TC, Kumar A, Majumdar RS, Yadav V (2016) Mechanistic basis of antimicrobial actions of silver nanoparticles. Front Microbiol 7:1–17. https://doi.org/10.3389/fmicb.2016.01831
Das B, Dash SK, Mandal D, Ghosh T, Chattopadhyay S, Tripathy S, Das S, Dey SK, Das D, Roy S (2017) Green synthesized silver nanoparticles destroy multidrug resistant bacteria via reactive oxygen species mediated membrane damage. Arab J Chem 10:862–876. https://doi.org/10.1016/j.arabjc.2015.08.008
Deng Y, Li J, Pub Y, Chen Y, Zhao J, Tang J (2016) Ultra-fine silver nanoparticles dispersed in mono-dispersed amino functionalized poly glycidyl methacrylate based microspheres as an effective anti-bacterial agent. React Funct Polym 103:92–98. https://doi.org/10.1016/j.reactfunctpolym.2016.04.007
Deshpande LM, Chopade BA (1994) Plasmid mediated silver resistance in Acinetobacter baumannii. BioMetals 7:49–56
Dos Santos CA, Seckler MM, Ingle AP, Gupta I, Galdiero S, Galdiero M, Gade A, Rai M (2014) Silver nanoparticles: therapeutical uses, toxicity, and safety issues. J Pharm Sci 103:1937–1944. https://doi.org/10.1002/jps.24001
DuBois M, Gilles KA, Hamilton JK, Rebers PA, Smith F (1956) Colorimetric method for determination of sugars and related substances. Anal Chem 28:350–356. https://doi.org/10.1021/ac60111a017
Durán N, Marcato PD, De Conti R, Alves OL, Costab FTM, Brocchi M (2010) Potential use of silver nanoparticles on pathogenic bacteria, their toxicity and possible mechanisms of action. J Braz Chem Soc 21:949–959. https://doi.org/10.1590/S0103-50532010000600002
El-Rab SG, Halawani E, Hassan A (2018) Formulation of ceftriaxone conjugated gold nanoparticles and their medical applications against extended-spectrum β-lactamase producing bacteria and breast cancer. J Microbiol Biotechnol 28:1563–1572. https://doi.org/10.4014/jmb.1711.11037
French VM, Cooper RA, Molan PC (2005) The antibacterial activity of honey against coagulase-negative Staphylococci. J Antimicrob Chemother 56:228–231. https://doi.org/10.1093/jac/dki193
González Fá AJ, Juan A, Di Nezio MS (2017) Synthesis and characterization of silver nanoparticles prepared with honey: the role of carbohydrates. Anal Lett 50:877–888. https://doi.org/10.1080/00032719.2016.1199558
Jadhav K, Dhamecha D, Bhattacharya D, Patil M (2016) Green and ecofriendly synthesis of silver nanoparticles: characterization, biocompatibility studies and gel formulation for treatment of infections in burns. J Photochem Photobiol B 155:109–115. https://doi.org/10.1016/j.jphotobiol.2016.01.002
Jovanovic Z, Stojkovska J, Obradovic B, Miskovic-Stankovic V (2012) Alginate hydrogel microbeads incorporated with Ag nanoparticles obtained by electrochemical method. Mater Chem Phys 133:182–189. https://doi.org/10.1016/j.matchemphys.2012.01.005
Kempf M, Rolain JM (2012) Emergence of resistance to carbapenems in Acinetobacter baumannii in Europe: clinical impact and therapeutic options. Int J Antimicrob Agents 39:105–114. https://doi.org/10.1016/j.ijantimicag.2011.10.004
Khan F, Hashmi MU, Khalid N, Hayat MQ, Ikram A, Janjua HA (2016) Controlled assembly of silver nano-fluid in Heliotropium crispum extract: a potent anti-biofilm and bactericidal formulation. Appl Surf Sci 387:317–331
Khatami M, Zafarnia N, Heydarpoor Bami M, Sharifi I, Singh H (2018) Antifungal and antibacterial activity of densely dispersed silver nanospheres with homogeneity size which synthesized using chicory: an in vitro study. J Mycol Med 28:637–644. https://doi.org/10.1016/j.apsusc.2016.05.133
Lateef A, Akande MA, Azeez MA, Ojo SA, Folarin BI, Gueguim-Kana EB, Beukes LS (2016) Phytosynthesis of silver nanoparticles (AgNPs) using miracle fruit plant (Synsepalum dulcificum) for antimicrobial, catalytic, anticoagulant, and thrombolytic applications. Nanotechnol Rev 5:1–14. https://doi.org/10.1515/ntrev-2016-0039
Lee H, Churey JJ, Worobo RW (2008) Antimicrobial activity of bacterial isolates from different floral sources of honey. Int J Food Microbiol 126:240–244. https://doi.org/10.1016/j.ijfoodmicro.2008.04.030
Majtan J (2014) Honey: an immunomodulator in wound healing. Wound Repair Regen 22:187–192. https://doi.org/10.1111/wrr.12117
Molan PC (2002) Re-introducing honey in the management of wounds and ulcers – theory and practice. Ostomy Wound Manage 48:28–40
Molan P (2009) Debridement of wounds with honey. J Wound Technol 5:12–17
Molan P, Rhodes T (2015) Honey: a biologic wound dressing. Wounds 27:141–151
Monteiro DR, Gorup LF, Takamiya AS, Ruvollo-Filho AC, Camargo ER, Barbos DB (2009) The growing importance of materials that prevent microbial adhesion: antimicrobial effect of medical devices containing silver. J Antimicrob Agents 34:103–110. https://doi.org/10.1016/j.ijantimicag.2009.01.017
Morones JR, Elechiguerra JL, Camacho A, Holt K, Kouri JB, Ramırez JT, Yacaman MJ (2005) The bactericidal effect of silver nanoparticles. Nanotechnology 16:2346–2353. https://doi.org/10.1088/0957-4484/16/10/059
Nagoba BS, Suryawanshi NM, Wadher B, Selkar S (2015) Acidic environment and wound healing: a review. Wounds 27:5–11
Obradovic B, Stojkovska J, Jovanovic Z, Miskovic-Stankovic V (2012) Novel alginate based nanocomposite hydrogels with incorporated silver nanoparticles. J Mater Sci Mater Med 23:99–107. https://doi.org/10.1007/s10856-011-4522-1
Obradovic B, Miskovic-Stankovic V, Jovanovic Z, Stojkovska J (2015) Production of alginate microbeads with incorporated silver nanoparticles. Patent no. RS53508 (B1), 2015 IPO Republic of Serbia
Pal S, Tak YK, Song JM (2007) Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the Gram-negative bacterium Escherichia coli. Appl Environ Microbiol 73:1712–1720. https://doi.org/10.1128/AEM.02218-06
Panáček A, Kvítek L, Smékalová M, Večeřová R, Kolář M, Röderová M, Dyčka F, Šebela M, Prucek R, Tomanec O, Zbořil R (2018) Bacterial resistance to silver nanoparticles and how to overcome it. Nature Nanotechnology 13(1):65–71. https://doi.org/10.1038/s41565-017-0013-y
Paosen S, Saising J, Septama AW, Voravuthikunchai SP (2017) Green synthesis of silver nanoparticles using plants from Myrtaceae family and characterization of their antibacterial activity. Mater Lett 209:201–206. https://doi.org/10.1016/j.matlet.2017.07.102
Paul W, Sharma CP (2004) Chitosan and alginate wound dressings: a short review. Trends Biomater Artif Organs 18:18–23
Peleg AY, Seifert H, Paterson DL (2008) Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 21:538–582. https://doi.org/10.1128/CMR.00058-07
Percival SL, Bowlera PG, Russell D (2005) Bacterial resistance to silver in wound care. J Hosp Infect 60:1–7. https://doi.org/10.1016/j.jhin.2004.11.014
Philip D (2010) Honey mediated green synthesis of silver nanoparticles. Spectrochim Acta A Mol Biomol Spectrosc 75:1078–1081. https://doi.org/10.1016/j.saa.2009.12.058
Queen D, Orsted H, Sanada H, Sussman G (2004) A dressing history. Int Wound J 1:59–77. https://doi.org/10.1111/j.1742-4801.2004.0009.x
Raman G, Park SJ, Sakthivel N, Suresh A (2017) Physico-cultural parameters during AgNPs biotransformation with bactericidal activity against human pathogens. Enzym Microb Technol 100:45–51. https://doi.org/10.1016/j.enzmictec.2017.02.002
Rodríguez-Baño J, Martí S, Soto S, Fernández-Cuenca F, Cisneros JM, Pachón J, Pascual A, Martínez-Martínez L, McQueary C, Actis LA, Vila J, Spanish Group for the Study of Nosocomial Infections (GEIH) (2008) Biofilm formation in Acinetobacter baumannii: associated features and clinical implications. Clin Microbiol Infect 3:276–278. https://doi.org/10.1111/j.1469-0691.2007.01916.x
Rossolini GM, Mantengoli E (2005) Treatment and control of severe infections caused by multiresistant Pseudomonas aeruginosa. Clin Microbiol Infect 11:17–32. https://doi.org/10.1111/j.1469-0691.2005.01161.x
Salas-Orozco M, Niño-Martínez N, Martínez-Castañón GA, Méndez FT, Compean Jasso ME, Ruiz F (2019) Mechanisms of resistance to silver nanoparticles in endodontic bacteria: a literature review. J Nanomater 2019:1–11. https://doi.org/10.1155/2019/7630316
Sarhan W, Azzazy H (2015) High concentration honey chitosan electrospun nanofibers: biocompatibility and antibacterial effects. Carbohydr Polym 122:135–143. https://doi.org/10.1016/j.carbpol.2014.12.051
Scandorieiro S, de Camargo LC, Lancheros C, Yamada-Ogatta S, Nakamura C, de Oliveira A, Andrade C, Duran N, Nakazato G, Kobayashi R (2016) Synergistic and additive effect of oregano essential oil and biological silver nanoparticles against multidrug-resistant bacterial strains. Front Microbiol 7:1–14. https://doi.org/10.3389/fmicb.2016.00760
Seal LA, Robson MC (2018) The influence of pH on chronic wound healing and the antimicrobial activity of chlorine. Ostomy Wound Manage 64:8–10
Skotti E, Anastasaki E, Kanellou G, Polissiou M, Tarantilis PA (2014) Total phenolic content, antioxidant activity and toxicity of aqueous extracts from selected Greek medicinal and aromatic plants. Ind Crop Prod 53:46–54. https://doi.org/10.1016/j.indcrop.2013.12.013
Slawson RM, Van Dyke MI, Lee H, Trevors JT (1992) Germanium and silver resistance, accumulation, and toxicity in microorganisms. Plasmid 27:72–79
Slistan-Grijalva A, Herrera-Urbina R, Rivas-Silva JF, Ávalos-Borja M, Castillón-Barraza FF, Posada-Amarillas A (2005a) Assessment of growth of silver nanoparticles synthesized from an ethylene glycol-silver nitrate-polyvinylpyrrolidone solution. Phys E 25:438–448. https://doi.org/10.1016/j.physe.2004.07.010
Slistan-Grijalva A, Herrera-Urbina R, Rivas-Silva JF, Ávalos-Borja M, Castillón-Barraza FF, Posada-Amarillas A (2005b) Classical theoretical characterization of the surface plasmon absorption band for silver spherical nanoparticles suspended in water and ethylene glycol. Phys E 27:104–112. https://doi.org/10.1016/j.physe.2004.10.014
Sreelakshmi C, Datta KK, Yadav JS, Reddy BV (2011) Honey derivatized Au and Ag nanoparticles and evaluation of its antimicrobial activity. J Nanosci Nanotechnol 11:6995–7000
Stojkovska J, Zvicer J, Jovanovic Z, Mišković-Stanković V, Obradovic B (2012) Controlled production of alginate nanocomposites with incorporated silver nanoparticles aimed for biomedical applications. J Serb Chem Soc 77:1709–1722. https://doi.org/10.2298/JSC121108148S
Stojkovska J, Kostic D, Jovanovic Z, Vukašinović-Sekulić M, Mišković-Stanković V, Obradovic B (2014) A comprehensive approach to in vitro functional evaluation of Ag/alginate nanocomposite hydrogels. Carbohydr Polym 111:305–314. https://doi.org/10.1016/j.carbpol.2014.04.063
Stojkovska J, Djurdjevic Z, Jancic I, Bufan B, Milenkovic M, Jankovic R, Miskovic-Stankovic V, Obradovic B (2018) Comparative in vivo evaluation of novel formulations based on alginate and silver nanoparticles for wound treatments. J Biomater Appl 32:1197–1211. https://doi.org/10.1177/0885328218759564
Thomas S, Fear M, Humphreys J, Disley L, Waring M (1996) The effect of dressings on the production of exudate from venous leg ulcers. Wounds 8:145–149
Tonks A, Cooper RA, Price AJ, Molan C, Jones KP (2001) Stimulation of TNF-alpha release in monocytes by honey. Cytokine 14:240–242. https://doi.org/10.1006/cyto.2001.0868
Vaidya MY, McBain AJ, Butler JA, Banks CE, Whitehead KA (2017) Antimicrobial efficacy and synergy of metal ions against Enterococcus faecium, Klebsiella pneumonia and Acinetobacter baumannii in planktonic and biofilm phenotypes. Sci Rep 7(5911):1–9. https://doi.org/10.1038/s41598-017-05976-9
Vidovic S, Zvicer J, Stojkovska J, Miskovic-Stankovic V, Obradovic B (2012) Nanocomposite microfibers based on alginate and PVA hydrogels with incorporated silver nanoparticles. J Tissue Eng Regen Med 6:189
Wan G, Ruan L, Yin Y, Yang T, Ge M, Cheng X (2016) Effects of silver nanoparticles in combination with antibiotics on the resistant bacteria Acinetobacter baumannii. Int J Nanomedicine 11:3789–3800. https://doi.org/10.2147/IJN.S104166
Wang T, Gu Q, Zhao J, Mei J, Shao M, Pan Y, Zhang J, Wu H, Zhang Z, Liu F (2015) Calcium alginate enhances wound healing by up-regulating the ratio of collagen types I/III in diabetic rats. Int J Clin Exp Pathol 8:6636–6645
Wang L, Hu C, Shao L (2017) The antimicrobial activity of nanoparticles: present situation and prospects for the future. Int J Nanomedicine 12:1227–1249. https://doi.org/10.2147/IJN.S121956
Wasihun AG, Kasa BG (2016) Evaluation of antibacterial activity of honey against multidrug resistant bacteria in Ayder Referral and Teaching Hospital, Northern Ethiopia. SpringerPlus 5:1–8. https://doi.org/10.1186/s40064-016-2493-x
Wintachain P, Paosen S, Yupanqui CT, Voravuthikunchai SP (2019) Silver nanoparticles synthesized with Eucalyptus critriodora ethanol leaf extract stimulate antibacterial activity against clinically multidrug-resistant Acinetobacter baumannii isolated from pneumonia patients. Microb Pathog 126:245–257. https://doi.org/10.1016/j.micpath.2018.11.018
Yaghoobi R, Kazerouni A, Kazerouni O (2013) Evidence for clinical use of honey in wound healing as an anti-bacterial, anti-inflammatory anti-oxidant and anti-viral agent: a review. Jundishapur J Nat Pharm Prod 8:100–104
Zbuchea A (2014) Up-to-date use of honey for burns treatment. Ann Burns Fire Disasters 27:22–30
Funding
This work was funded by the Ministry of Education, Science and Technological Development of the Republic of Serbia (Grant III 45019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 264 kb)
Rights and permissions
About this article
Cite this article
Stojkovska, J., Petrovic, P., Jancic, I. et al. Novel nano-composite hydrogels with honey effective against multi-resistant clinical strains of Acinetobacter baumannii and Pseudomonas aeruginosa. Appl Microbiol Biotechnol 103, 8529–8543 (2019). https://doi.org/10.1007/s00253-019-10055-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-019-10055-2