Abstract
Background
Ideally, suspected airway compression in symptomatic children with lymphobronchial tuberculosis (TB) would be diagnosed using modern computed tomography (CT) assisted by coronal minimum intensity projection (MinIP) reconstructions. However, in TB-endemic regions with limited resources, practitioners rely on conventional radiography for diagnosing TB and its complications. Furthermore, airway compression detected on conventional radiographs would upgrade a patient into the severe category according to the new World Health Organization guidelines, precluding the patient from shorter treatment protocols. The accuracy of conventional radiographs in the context of detecting airway compression in children with TB has not been specifically evaluated against an imaging gold standard.
Objective
We aimed to compare frontal chest radiographs against thick-slab angled coronal CT MinIP in identifying airway stenosis at ten specific sites and to determine observer agreement between the modalities regarding the degree of stenosis.
Materials and methods
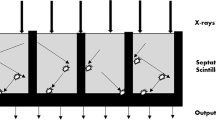
This retrospective cross-sectional study compared chest radiographs with standardized angled coronal CT MinIP in children with symptomatic lymphobronchial TB at ten predetermined airway locations. Chest radiographs were evaluated by one pediatric radiologist and CT MinIP reconstructions were independently interpreted by three readers. Sensitivity and specificity were calculated using CT MinIP as the gold standard. Stenosis was graded as 1 for mild (1–50%), 2 for moderate (51–75%), 3a for severe (76–99%), and 3b for total occlusion (100%). Agreement between the two modalities regarding severity of stenosis was calculated using the kappa coefficient for each affected site.
Results
A total of 37 patients were included in the study. The median age of patients was 14.3 months (interquartile range 8.0–23.2). Three hundred and seventy individual bronchi (10 from each of the 37 patients) were evaluated for stenosis. Chest radiographs showed that 31 out of 37 (84%) patients had stenosis in at least one of ten evaluated sites, most commonly the left main bronchus and bronchus intermedius, and this was confirmed via CT MinIP. The gold standard (CT MinIP) demonstrated stenosis in at least one of ten sites in all 37 patients (100%). Left main bronchus stenosis was detected by chest radiography with a 92.9% sensitivity and 100% specificity. Sensitivity and specificity for bronchus intermedius stenosis were 80% and 75%, respectively. There was substantial agreement for grade of stenosis between chest radiographs and CT (kappa=0.67) for the left main bronchus and moderate agreement (kappa=0.58) for the bronchus intermedius. Severe stenosis was found in 78 bronchi on CT compared to 32 bronchi (Grade 3a: 9, Grade 3b: 23) on chest radiographs.
Conclusion
The diagnosis of pulmonary TB in children continues to rely heavily on imaging, and we have shown that in young children, chest radiographs had a high sensitivity and specificity for detecting airway stenosis at certain anatomical sites, when adequately visualized, resulting from tuberculous lymph node compression at left main bronchus and bronchus intermedius. For most sites, the interobserver agreement was poor. Stenosis of the left main bronchus and bronchus intermedius should be the focus of chest radiograph interpretation and can assist both diagnosis and classification of patients for treatment.
Graphical Abstract





Similar content being viewed by others
Data availability
The data presented in this study is available on reasonable request from the corresponding author.
References
(2022) World Health Organization (WHO) consolidated guidelines on tuberculosis: Module 5: Management of tuberculosis in children and adolescents. World Health Organization, Geneva
Van Dyck P, Vanhoenacker FM, Van den Brande P, De Schepper AM (2003) Imaging of pulmonary tuberculosis. Eur Radiol 13:1771–1785
Andronikou S, Joseph E, Lucas S et al (2004) CT scanning for the detection of tuberculous mediastinal and hilar lymphadenopathy in children. Pediatr Radiol 34:232–236
Maydell A, Goussard P, Andronikou S et al (2010) Radiological changes post-lymph node enucleation for airway obstruction in children with pulmonary tuberculosis. Eur J Cardiothorac Surg 38:478–483
Richter-Joubert L, Andronikou S, Workman L, Zar HJ (2017) Assessment of airway compression on chest radiographs in children with pulmonary tuberculosis. Pediatr Radiol 47:1283–1291
Du Plessis J, Goussard P, Andronikou S et al (2009) Comparing three-dimensional volume-rendered CT images with fibreoptic tracheobronchoscopy in the evaluation of airway compression caused by tuberculous lymphadenopathy in children. Pediatr Radiol 39:694–702
Leung AN, Müller NL, Pineda PR, FitzGerald JM (1992) Primary tuberculosis in childhood: radiographic manifestations. Radiology 182:87–91
Andronikou S, Vanhoenacker FM, De Backer AI (2009) Advances in imaging chest tuberculosis: blurring of differences between children and adults. Clin Chest Med 30:717–44, viii
Delacourt C, Mani TM, Bonnerot V et al (1993) Computed tomography with normal chest radiograph in tuberculous infection. Arch Dis Child 69:430–432
Berteloot L, Marcy O, Nguyen B et al (2018) Value of chest X-ray in TB diagnosis in HIV-infected children living in resource-limited countries: the ANRS 12229-PAANTHER 01 study. Int J Tuberc Lung Dis 22:844–850
Swingler GH, du Toit G, Andronikou S et al (2005) Diagnostic accuracy of chest radiography in detecting mediastinal lymphadenopathy in suspected pulmonary tuberculosis. Arch Dis Child 90:1153–1156
Triasih R, Robertson C, de Campo J et al (2015) An evaluation of chest X-ray in the context of community-based screening of child tuberculosis contacts. Int J Tuberc Lung Dis 19:1428–1434. https://doi.org/10.5588/ijtld.15.0201
Uzum K, Karahan OI, Dogan S et al (2003) Chest radiography and thoracic computed tomography findings in children who have family members with active pulmonary tuberculosis. Eur J Radiol 48:258–262
Marais BJ, Gie RP, Schaaf HS et al (2006) Childhood pulmonary tuberculosis: old wisdom and new challenges. Am J Respir Crit Care Med 173:1078–1090
Weismuller MM, Graham SM, Claessens NJM et al (2002) Diagnosis of childhood tuberculosis in Malawi: an audit of hospital practice. Int J Tuberc Lung Dis 6:432–438
Enarson PM, Enarson DA, Gie R (2005) Management of tuberculosis in children in low-income countries. Int J Tuberc Lung Dis 9:1299–1304
Andronikou S, Wieselthaler N (2004) Modern imaging of tuberculosis in children: thoracic, central nervous system and abdominal tuberculosis. Pediatr Radiol 34:861–875
Goussard P, Gie R (2007) Airway involvement in pulmonary tuberculosis. Paediatr Respir Rev 8:118–123
Venkatakrishna SSB, Krim AOA, Calle-Toro J et al (2023) Comparison of single coronal thick-slab minimum intensity projection with flexible bronchoscopy for airway compression in children with lymphobronchial tuberculosis. Clin Radiol. https://doi.org/10.1016/j.crad.2023.03.021
Goussard P, Gie RP, Kling S et al (2013) Bronchoscopic assessment of airway involvement in children presenting with clinically significant airway obstruction due to tuberculosis. Pediatr Pulmonol 48:1000–1007
Lucas S, Andronikou S, Goussard P, Gie R (2012) CT features of lymphobronchial tuberculosis in children, including complications and associated abnormalities. Pediatr Radiol 42:923–931
Kim WS, Choi J-I, Cheon J-E et al (2006) Pulmonary tuberculosis in infants: radiographic and CT findings. AJR Am J Roentgenol 187:1024–1033
Buonsenso D, Pata D, Visconti E et al (2021) Chest CT scan for the diagnosis of pediatric pulmonary TB: radiological findings and its diagnostic significance. Front Pediatr 9:583197
Kim WS, Moon WK, Kim IO et al (1997) Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol 168:1005–1009
Author information
Authors and Affiliations
Contributions
S.A. conceived the study and design. D.B., A.O.A.K., and S.A. performed data collection. S.S.B.V., D.B., S.L., A.O.A.K., and S.A. performed data analysis. S.S.B.V., D.B., S.L., A.O.A.K., and S.A. drafted the initial manuscript. J.S.C.T. and P.G. assisted with edits and review of the drafts. S.S.B.V. and S.A. performed reviews and revisions. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Venkatakrishna, S.S.B., Bester, D., Calle-Toro, J.S. et al. Comparison of chest radiographs against minimum intensity projection reconstruction computed tomography scans for detection of airway stenosis in children with lymphobronchial tuberculosis. Pediatr Radiol 54, 596–605 (2024). https://doi.org/10.1007/s00247-023-05809-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05809-0