Abstract
Background
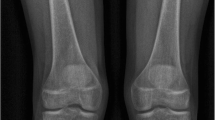
Hip displacement in children with cerebral palsy (CP) is monitored by measuring migration percentage on anteroposterior pelvis radiographs. However, proper positioning for radiography in children with spasticity is difficult. The reliability and accuracy of migration percentage as a function of patient positioning is unknown.
Objective
To determine the effects of patient positioning on migration percentage measurements in children with CP.
Materials and methods
We identified children with CP (≤18-year-old) with pelvis CT and anteroposterior pelvis radiograph obtained <6 months apart (10/2018–11/2021). Digitally reconstructed radiographs were generated from each pelvis CT, to simulate nine different patient positions: neutral; 10° and 20° lordosis and kyphosis; and 10° and 20° right rotation and left rotation. Two radiologists measured migration percentages from the simulated and real pelvis radiographs. We used Spearman’s rho to assess inter-rater reliability, and Wilcoxon signed rank test to determine statistical significance.
Results
We studied sixty-three children (male=41; median age=8 years; range=4–18 years). The two radiologists’ migration percentage measurements were highly correlated with each other across all simulated and real radiographs (Spearman’s rho=0.86–0.99, P<0.01). For both readers and hips, migration percentages measured from real radiographs were significantly different from those measured from neutral simulated radiographs (P<0.01), with median absolute difference=5–6 percentage points (PP) and interquartile range (IQR)=9–12 PP. When comparing migration percentage measurements from neutral simulated radiographs to those in kyphosis/lordosis and right/left rotations, median absolute differences were 2–4 PP (IQR=3–8 PP) and 4–15 PP (IQR=6–17 PP), respectively.
Conclusion
Inter-rater reliability of measured migration percentages is high, but accuracy decreases with patient positional changes.
Graphical abstract






Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Code availability
Not applicable
References
Oskoui M, Coutinho F, Dykeman J et al (2013) An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55:509–519
Durkin MS, Benedict RE, Christensen D et al (2016) Prevalence of cerebral palsy among 8-year-old children in 2010 and preliminary evidence of trends in its relationship to low birthweight. Paediatr Perinat Epidemiol 30:496–510
Soo B, Howard JJ, Boyd RN et al (2006) Hip displacement in cerebral palsy. J Bone Joint Surg Am 88:121–129
Hagglund G, Lauge-Pedersen H, Wagner P (2007) Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord 8:101
Hagglund G, Andersson S, Duppe H et al (2005) Prevention of dislocation of the hip in children with cerebral palsy. The first ten years of a population-based prevention programme. J Bone Joint Surg Br 87:95–101
DiFazio R, Shore B, Vessey JA et al (2016) Effect of hip reconstructive surgery on health-related quality of life of non-ambulatory children with cerebral palsy. J Bone Joint Surg Am. 98:1190–8
Connelly A, Flett P, Graham HK, Oates J (2009) Hip surveillance in Tasmanian children with cerebral palsy. J Paediatr Child Health 45:437–743
Wynter M, Gibson N, Kentish M et al (2011) The development of Australian standards of care for hip surveillance in children with cerebral palsy: how did we reach consensus? J Pediatr Rehabil Med 4:1–12
Robb JE, Hagglund G (2013) Hip surveillance and management of the displaced hip in cerebral palsy. J Child Orthop 7:407–13
Hagglund G, Alriksson-Schmidt A, Lauge-Pedersen H et al (2014) Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J 96:1546–1552
Shrader MW, Wimberly L, Thompson R (2019) Hip surveillance in children with cerebral palsy. J Am Acad Orthop Surg 15:760–768
Reimers J (1980) The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 184:1–100
Shore B, Spence D, Graham HK (2012) The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med 5:126–134
Craven A, Pym A, Boyd RN (2014) Reliability of radiologic measures of hip displacement in a cohort of preschool-aged children with cerebral palsy. J Pediatr Orthop 34:597–602
Demir N, Demirel M, Turna O et al (2021) Effect of clinician’s experience and expertise on the inter- and intra-observer reliability of hip migration index in children with cerebral palsy: a STROBE-compliant retrospective study. Medicine (Baltimore) 100:e24538
Portinaro NM, Murray DW, Bhullar TP, Benson MK (1995) Errors in measurement of acetabular index. J Pediatr Orthop 15:780–784
Tachibana T, Fujii M, Kitamura K et al (2019) Does acetabular coverage vary between the supine and standing positions in patients with hip dysplasia? Clin Orthop Relat Res 477:2455–2466
Bhanushali A, Chimutengwende-Gordon M, Beck M et al (2021) The variation in hip stability measurements between supine and standing radiographs of dysplastic hips. Bone Joint J 103-B:1662–1668
Bax MC, Flodmark O, Tydeman C (2007) Definition and classification of cerebral palsy. From syndrome toward disease. Dev Med Child Neurol Suppl 109:39–41
American College of Radiology (2018) ACR-SPR-SSR practice parameter for the performance of radiography of the extremities (Res. 6). In: American College of Radiology. ACR Standards. Reston, VA: American College of Radiology
Dobson F, Boyd RN, Parrott J et al (2002) Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br. 84:720–726
Siebenrock KA, Kalbermatten DF, Ganz R (2003) Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 407:241–248
Imai N, Ito T, Suda K et al (2013) Pelvic flexion measurement from lateral projection radiographs is clinically reliable. Clin Orthop Relat Res 471:1271–1276
Pierrepont J, Hawdon G, Miles BP et al (2017) Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint J 99:184–191
Benjamini Y, Yekutieli D (2005) Quantitative trait Loci analysis using the false discovery rate. Genetics 171:783–790
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
IRB approved
Consent to participate
IRB exempt status
Consent for publication
IRB exempt status
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jarrett, D.Y., Stamoulis, C., Shore, B.J. et al. Pelvis radiographs in children with cerebral palsy: effects of patient positioning on calculating migration percentages. Pediatr Radiol 53, 2662–2671 (2023). https://doi.org/10.1007/s00247-023-05783-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05783-7