Abstract
Background
Fracture dating from skeletal surveys is crucial in the diagnosis and investigation of infant abuse. However, this task is challenging because of the subjective nature of the radiologic interpretation and the lack of ground truth. Researchers have used birth-related clavicle fractures as a surrogate to study the radiographic pattern of healing; however, they did not elucidate the accuracy performance of the radiologists in dating fractures.
Objective
To determine the accuracy of radiologists in dating birth-related clavicle fractures and compare their performance to that achieved by computer algorithm.
Materials and methods
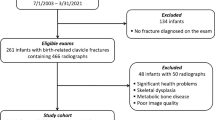
We used a previously assembled birth-related clavicle fracture database consisting of 416 anteroposterior clavicle radiographs as the study cohort. The average and standard deviation of the fracture age within this database were 24 days and 18 days, respectively. Three blinded radiologists independently estimated the ages of the clavicle fractures depicted in the radiographs within the database. We compared these estimation results to those made by a recently published deep-learning (DL) model conducted with the identical infant cohort. We calculated standard error metrics to compare the accuracy performances of the radiologists and the computer model.
Results
The intra- and inter-reader agreements of the fracture age estimates by the radiologists were moderate to good. The radiologists estimated the fracture ages with a mean absolute error (MAE) of 6.1–7.1 days, and standard deviation of the absolute error of 6.3–8.3 days. The accuracy performances of the three radiologists were not significantly different from one another. In comparison, the DL model estimated the age of clavicle fractures with an MAE of 4.2 days, significantly lower than all of the radiologists (P < 0.001).
Conclusion
Three experienced pediatric radiologists dated clavicular fractures with moderate–good intra- and inter-reader agreements. The correlations between the radiologists’ estimates and the ground truth were moderate to good. The fracture ages assigned by the DL model showed superior correlation with the ground truth compared to radiologists’ dating estimates.








Similar content being viewed by others
References
Cumming WA (1979) Neonatal skeletal fractures. Birth trauma or child abuse? J Can Assoc Radiol 30:30–33
O’Connor JF, Cohen J (1987) Dating fractures. In: Kleinman PK (ed) Diagnostic imaging of child abuse. Williams & Wilkins, Baltimore, pp 103–113
Yeo LI, Reed MH (1994) Staging of healing of femoral fractures in children. Can Assoc Radiol J 45:16–19
Islam O, Soboleski D, Symons S et al (2000) Development and duration of radiographic signs of bone healing in children. AJR Am J Roentgenol 175:75–78
Malone CA, Sauer NJ, Fenton TW (2011) A radiographic assessment of pediatric fracture healing and time since injury. J Forensic Sci 56:1123–1130
Halliday K, Broderick N, Somers J, Hawkes R (2011) Dating fractures in infants. Clin Radiol 66:1049–1054
Prosser I, Lawon Z, Evans A et al (2012) A timetable for the radiologic features of fracture healing in young children. AJR Am J Roentgenol 198:1014–1120
Sanchez TR, Nguyen H, Palacios W et al (2013) Retrospective evaluation and dating of non-accidental rib fractures in infants. Clin Radiol 68:e467–e471
Warner C, Maguire S, Trefan L et al (2017) A study of radiological features of healing in long bone fractures among infants less than a year. Skeletal Radiol 46:333–341
Crompton S, Messina F, Klafkowski G et al (2021) Validating scoring systems for fracture healing in infants and young children: pilot study. Pediatr Radiol 51:1682–1689
Kyllonen KM, Monson KL, Smith MA (2022) Postmortem and antemortem forensic assessment of pediatric fracture healing from radiographs and machine learning classification. Biology 11:749
Walters MM, Forbes PW, Buonomo C, Kleinman PK (2014) Healing patterns of clavicular birth injuries as a guide to fracture dating in cases of possible infant abuse. Pediatr Radiol 44:1224–1229
Fadell M, Miller A, Trefan L et al (2017) Radiological features of healing in newborn clavicular fractures. Eur Radiol 27:2180–2187
Tsai A, Grant PE, Warfield SK et al (2022) Deep learning of birth-related infant clavicle fractures: a potential virtual consultant for fracture dating. Pediatr Radiol 52:2206–2214
Koch GG (1982) Intraclass correlation coefficient. In: Kotz S, Johnson NL (eds) Encyclopedia of statistical sciences, vol 4. Wiley, New York, pp 213–217
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Barber I, Perez-Rossello JM, Wilson CR, Kleinman PK (2015) The yield of high-detail radiographic skeletal surveys in suspected infant abuse. Pediatr Radiol 45:69–80
Acknowledgements
Research reported in this publication was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under award number R21HD108634 to Andy Tsai. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Research reported in this publication was also supported in part by the Radiological Society of North America (RSNA) Research & Education Foundation, through Research Seed Grant RSD2133 to Andy Tsai. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the RSNA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsai, A., Pérez-Rosselló, J.M., Ecklund, K. et al. Dating birth-related clavicular fractures: pediatric radiologists versus artificial intelligence. Pediatr Radiol 53, 1117–1124 (2023). https://doi.org/10.1007/s00247-023-05590-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05590-0