Abstract
Background
Increasing evidence supports an association among congenital heart disease (CHD), structural brain lesions on neuroimaging, and increased risk of neurodevelopmental delay and other structural anomalies. Fetal MRI has been found to be effective in demonstrating fetal structural and developmental abnormalities.
Objective
To determine the contribution of fetal MRI to identifying cardiovascular and non-cardiovascular anomalies in fetuses with CHD compared to prenatal US and fetal echocardiography.
Materials and methods
We performed a retrospective study of fetuses with CHD identified by fetal echocardiography. Exams were performed on 1.5-tesla (T) or 3-T magnets using a balanced turbo field echo sequence triggered by an external electrocardiogram simulator with a fixed heart rate of 140 beats per minute (bpm). Fetal echocardiography was performed by pediatric cardiologists and detailed obstetrical US by maternal–fetal medicine specialists prior to referral to MRI. We compared the sensitivity of fetal MRI and fetal echocardiography for the diagnosis of cardiovascular anomalies, as well as the sensitivity of fetal MRI and referral US for the diagnosis of non-cardiac anomalies. We performed statistical analysis using the McNemar test.
Results
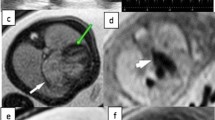
We identified 121 anomalies in 31 fetuses. Of these, 73 (60.3%) were cardiovascular and 48 (39.7%) involved other organ systems. Fetal echocardiography was more sensitive for diagnosing cardiovascular anomalies compared to fetal MRI, but the difference was not statistically significant (85.9%, 95% confidence interval [CI] 77.8–94.0% vs. 77.5%, 95% CI 67.7–87.2%, respectively; McNemar test 2.29; P=0.13). The sensitivity of fetal MRI was higher for diagnosing extracardiac anomalies when compared to referral US (84.1%, 95% CI 73.3–94.9% vs. 31.8%, 95% CI 18.1–45.6%, respectively; McNemar test 12.9; P<0.001). The additional information provided by fetal MRI changed prognosis, counseling or management for 10/31 fetuses (32.2%), all in the group of 19 fetuses with anomalies in other organs and systems besides CHD.
Conclusion
Fetal MRI performed in a population of fetuses with CHD provided additional information that altered prognosis, counseling or management in approximately one-third of the fetuses, mainly by identifying previously unknown anomalies in other organs and systems.






Similar content being viewed by others
References
Khalil A, Bennet S, Thilaganathan B et al (2016) Prevalence of prenatal brain abnormalities in fetuses with congenital heart disease: a systematic review. Ultrasound Obstet Gynecol 48:296–307
Griffiths PD, Mousa HA, Finney C et al (2019) An integrated in utero MR method for assessing structural brain abnormalities and measuring intracranial volumes in fetuses with congenital heart disease: results of a prospective case-control feasibility study. Neuroradiology 61:603–611
Mlczoch E, Brugger P, Ulm B et al (2013) Structural congenital brain disease in congenital heart disease: results from a fetal MRI program. Eur J Paediatr Neurol 17:153–160
Brossard-Racine M, du Plessis AJ, Vezina G et al (2014) Prevalence and spectrum of in utero structural brain abnormalities in fetuses with complex congenital heart disease. AJNR Am J Neuroradiol 35:1593–1599
Limperopoulos C, Tworetzky W, McElhinney DB et al (2010) Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121:26–33
Zeng S, Zhou QC, Zhou JW et al (2015) Volume of intracranial structures on three-dimensional ultrasound in fetuses with congenital heart disease. Ultrasound Obstet Gynecol 46:174–181
Sun L, Macgowan CK, Sled JG et al (2015) Congenital heart disease reduced fetal cerebral oxygen consumption is associated with smaller brain size in fetuses with congenital heart disease. Circulation 131:1313–1323
Schellen C, Ernst S, Gruber GM et al (2015) Fetal MRI detects early alterations of brain development in tetralogy of Fallot. Am J Obstet Gynecol 213:392.e1–392.e7
Clouchoux C, du Plessis AJ, Bouyssi-Kobar M et al (2013) Delayed cortical development in fetuses with complex congenital heart disease. Cereb Cortex 23:2932–2943
Masoller N, Sanz-CorteS M, Crispi F et al (2016) Mid-gestation brain Doppler and head biometry in fetuses with congenital heart disease predict abnormal brain development at birth. Ultrasound Obstet Gynecol 47:65–73
Eom M, Choi YD, Kim YS et al (2007) Clinico-pathological characteristics of congenital pulmonary lymphangiectasis: report of two cases. J Korean Med Sci 22:740–745
France NE, Brown RJK (1971) Congenital pulmonary lymphangiectasis: report of 11 examples with special reference to cardiovascular findings. Arch Dis Child 46:528–532
Raman SP, Pipavath SNJ, Raghu G et al (2009) Imaging of thoracic lymphatic diseases. AJR Am J Roentgenol 193:1504–1513
Saul D, Degenhardt K, Iyoob SD et al (2016) Hypoplastic left heart syndrome and the nutmeg lung pattern in utero: a cause and effect relationship or prognostic indicator? Pediatr Radiol 46:483–489
Noonan JA, Walters LR, Reeves JT (1970) Congenital pulmonary lymphangiectasis. Am J Dis Child 120:314–319
Victoria T, Andronikou S (2014) The fetal MR appearance of ‘nutmeg lung’: findings in 8 cases linked to pulmonary lymphangiectasia. Pediatr Radiol 44:1237–1242
Mackesy MM, Kalish BT, Tworetzky W et al (2017) Sonographic pulmonary abnormalities in fetuses with hypoplastic left heart syndrome and intact atrial septum undergoing attempted atrial septostomy in utero. Ultrasound Q 33:82–85
Barrera CA, Johnson AM, Rychik J et al (2021) Prognostic value of the nutmeg lung pattern/lymphangiectasia on fetal magnetic resonance imaging. Pediatr Radiol 51:1809–1817
Ruchonnet-Metrailler I, Bessieres B, Bonnet D et al (2014) Pulmonary hypoplasia associated with congenital heart diseases: a fetal study. PLoS One 9:e93557
Freud LR, Escobar-Diaz MC, Kalish BT et al (2015) Outcomes and predictors of perinatal mortality in fetuses with Ebstein anomaly or tricuspid valve dysplasia in the current era: a multicenter study. Circulation 132:481–489
Kochanski J, Bardo D, Goncalves L, Lindblade C (2019) Prenatal diagnosis of a unique scimitar syndrome variant — a case report. Prenat Cardiol 2019:42–46
England EC, Cornejo P, Neilson DE et al (2021) Fetal brain small vessel disease 1 caused by a novel mutation in the COL4A1 gene. Pediatr Radiol 51:480–484
Léonard A, Bernard P, Hiel AL, Hubinont C (2009) Prenatal diagnosis of fetal cataract: case report and review of the literature. Fetal Diagn Ther 26:61–67
Seed M, Bradley T, Bourgeois J et al (2009) Antenatal MR imaging of pulmonary lymphangiectasia secondary to hypoplastic left heart syndrome. Pediatr Radiol 39:747–749
Lam CZ, Bhamare TA, Gazzaz T et al (2017) Diagnosis of secondary pulmonary lymphangiectasia in congenital heart disease: a novel role for chest ultrasound and prognostic implications. Pediatr Radiol 47:1441–1451
Blask AR, Fagen KE, Rubio EI et al (2021) Prenatal diagnosis of intestinal nonrotation using magnetic resonance imaging: is it possible? Pediatr Radiol 51:1332–1338
Chaptinel J, Yerly J, Mivelaz Y et al (2017) Fetal cardiac cine magnetic resonance imaging in utero. Sci Rep 7:15540
Roy CW, Seed M, Kingdom JC, Macgowan CK (2017) Motion compensated cine CMR of the fetal heart using radial undersampling and compressed sensing. J Cardiovasc Magn Reson 19:29
Kording F, Schoennagel BP, de Sousa MT et al (2018) Evaluation of a portable Doppler ultrasound gating device for fetal cardiac MR imaging: initial results at 1.5T and 3T. Magn Reson Med Sci 17:308–317
Kording F, Yamamura J, de Sousa MT et al (2018) Dynamic fetal cardiovascular magnetic resonance imaging using Doppler ultrasound gating. J Cardiovasc Magn Reson 20:17
Tavares de Sousa M, Hecher K, Yamamura J et al (2019) Dynamic fetal cardiac magnetic resonance imaging in four-chamber view using Doppler ultrasound gating in normal fetal heart and in congenital heart disease: comparison with fetal echocardiography. Ultrasound Obstet Gynecol 53:669–675
Goncalves LF, Lee W, Mody S et al (2016) Diagnostic accuracy of ultrasonography and magnetic resonance imaging for the detection of fetal anomalies: a blinded case-control study. Ultrasound Obstet Gynecol 48:185–192
Rossi AC, Prefumo F (2014) Additional value of fetal magnetic resonance imaging in the prenatal diagnosis of central nervous system anomalies: a systematic review of the literature. Ultrasound Obstet Gynecol 44:388–393
Jarvis D, Mooney C, Cohen J et al (2017) A systematic review and meta-analysis to determine the contribution of MR imaging to the diagnosis of foetal brain abnormalities in utero. Eur Radiol 27:2367–2380
van Doorn M, Oude Rengerink K, Newsum EA et al (2016) Added value of fetal MRI in fetuses with suspected brain abnormalities on neurosonography: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 29:2949–2961
Sileo FG, Di Mascio D, Rizzo G et al (2021) Role of prenatal magnetic resonance imaging in fetuses with isolated agenesis of corpus callosum in the era of fetal neurosonography: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 100:7–16
van der Hoek-Snieders HEM, van den Heuvel AJML, van Os-Medendorp H et al (2019) Diagnostic accuracy of fetal MRI to detect cleft palate: a meta-analysis. Eur J Pediatr 179:164–171
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goncalves, L.F., Lindblade, C.L., Cornejo, P. et al. Contribution of fetal magnetic resonance imaging in fetuses with congenital heart disease. Pediatr Radiol 52, 513–526 (2022). https://doi.org/10.1007/s00247-021-05234-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05234-1