Abstract
Background
More than 70% of human immunodeficiency virus (HIV)-positive children sustain respiratory diseases in their lifetime. Imaging plays an important role in establishing early and correct diagnosis.
Objective
To evaluate the diagnostic accuracy of 3-Tesla (T) thorax MRI in HIV-positive children, using chest CT as the gold standard.
Materials and methods
We included 25 children with confirmed HIV-positive status and pulmonary complaints who were referred for chest CT. All children had 3-T thorax MRI using T2-W turbo spin-echo sequence, steady-state free precession gradient echo sequence, T2-W turbo spin-echo MultiVane XD sequence, and T1-weighted modified Dixon sequences. We evaluated the images for various pulmonary and mediastinal findings and calculated the sensitivity and specificity of 3-T thoracic MRI.
Results
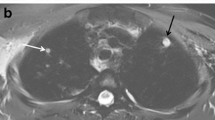
Sensitivity of 3-T MRI was 100% for detecting nodules >4 mm (95% confidence interval [CI] 66.3–100%), pleural effusion (CI 29.2–100%) and lymphadenopathy (CI 81.5–100%). It demonstrated a specificity of 100% for nodules >4 mm (CI 79.4–100%), pleural effusion (CI 84.6–100%) and lymphadenopathy (CI 59–100%). For consolidation/collapse, sensitivity and specificity were 93.8% (CI 69.8–99.8%) and 88.9% (CI 51.8–99.7%), respectively. The sensitivity and specificity for detecting bronchiectasis were 75% (CI 42.8–94.5%) and 100% (CI 75.3–100%), respectively, while for ground-glass opacity, sensitivity and specificity were 75% (CI 34.9–96.8%) and 94.1% (CI 71.3–99.9%), respectively. Nodules <4 mm were not well detected on MRI, with sensitivity of 35% (CI 15.4–59.2%).
Conclusion
Thoracic MRI at 3 T demonstrates a high sensitivity and specificity for detecting nodules >4 mm, effusion and lymphadenopathy in HIV-positive children.



Similar content being viewed by others
References
(2019) Global HIV/AIDS overview. AIDS.gov. https://www.aids.gov/federal-resources/around.../global-aids-overview. Accessed 29 Aug 2019
Norton KI, Kattan M, Rao JS et al (2001) Chronic radiographic lung changes in children with vertically transmitted HIV-1 infection. AJR Am J Roentgenol 176:1553–1558
Akinbami AA, Adegboyega AO, Oshinaike OO et al (2011) Chest X-ray findings in HIV patients in relation to the CD4 count. Nig Q J Hosp Med 21:306–311
Welte T (2014) Imaging in the diagnosis of lung disease: more sophisticated methods require greater interdisciplinary collaboration. Dtsch Arztebl Int 111:179–180
American College of Radiology (ACR) (2019) ACR appropriateness criteria: acute respiratory illness in HIV-positive patients. www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonThoracicImaging/AcuteRespiratoryIllnessinHIVPositivePatients-Doc2.aspx. Accessed 29 Aug 2019
Brenner DJ, Hall EJ (2007) Computed tomography — an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Sodhi KS, Krishna S, Saxena AK et al (2015) Clinical application of 'justification' and 'optimization' principle of ALARA in pediatric CT imaging: "how many children can be protected from unnecessary radiation?". Eur J Radiol 84:1752–1757
Brody AS, Frush DP, Huda W, Brent RL (2007) Radiation risk to children from computed tomography. Pediatrics 120:677–682
Yikilmaz A, Koc A, Coskun A et al (2011) Evaluation of pneumonia in children: comparison of MRI with fast imaging sequences at 1.5 T with chest radiographs. Acta Radiol 52:914–919
Biederer J, Mirsadraee S, Beer M et al (2012) MRI of the lung (3/3)-current applications and future perspectives. Insights Imaging 3:373–386
Peltola V, Ruuskanen O, Svedstrom E (2008) Magnetic resonance imaging of lung infections in children. Pediatr Radiol 38:1225–1231
Zar HJ, Andronikou S, Nicol MP (2017) Advances in the diagnosis of pneumonia in children. BMJ 358:j2739
Hirsch W, Sorge I, Krohmer S et al (2008) MRI of the lungs in children. Eur J Radiol 68:278–288
Manson DE (2013) MR imaging of the chest in children. Acta Radiol 54:1075–1085
Sodhi KS, Sharma M, Saxena AK et al (2017) MRI in thoracic tuberculosis of children. Indian J Pediatr 84:670–676
Rizzi EB, Schinina V, Cristofaro M et al (2011) Detection of pulmonary tuberculosis: comparing MR imaging with HRCT. BMC Infect Dis 11:243
Serra G, Milito C, Mitrevski M et al (2011) Lung MRI as a possible alternative to CT scan for patients with primary immune deficiencies and increased radiosensitivity. Chest 140:1581–1589
Arslan S, Poyraz N, Ucar R et al (2016) Magnetic resonance imaging may be a valuable radiation-free technique for lung pathologies in patients with primary immunodeficiency. J Clin Immunol 36:66–72
Eibel R, Herzog P, Dietrich O et al (2006) Pulmonary abnormalities in immunocompromised patients: comparative detection with parallel acquisition MR imaging and thin-section helical CT. Radiology 241:880–891
Leutner CC, Gieseke J, Lutterbey G et al (2000) MR imaging of pneumonia in immunocompromised patients: comparison with helical CT. AJR Am J Roentgenol 175:391–397
Montella S, Maglione M, Bruzzese D et al (2012) Magnetic resonance imaging is an accurate and reliable method to evaluate non-cystic fibrosis paediatric lung disease. Respirology 17:87–91
Sodhi KS, Khandelwal N, Saxena A et al (2016) Rapid lung MRI: paradigm shift in evaluation of febrile neutropenia in children with leukemia: a pilot study. Leuk Lymphoma 57:70–75
Gorkem SB, Coskun A, Yikilmaz A et al (2013) Evaluation of pediatric thoracic disorders: comparison of unenhanced fast-imaging-sequence 1.5-T MRI and contrast-enhanced MDCT. AJR Am J Roentgenol 200:1352–1357
Ozcan HN, Gormez A, Ozsurekci Y et al (2017) Magnetic resonance imaging of pulmonary infection in immunocompromised children: comparison with multidetector computed tomography. Pediatr Radiol 47:146–153
Yan C, Tan X, Wei Q et al (2015) Lung MRI of invasive fungal infection at 3 tesla: evaluation of five different pulse sequences and comparison with multidetector computed tomography (MDCT). Eur J Radiol 25:550–557
Attenberger UI, Morelli JN, Henzler T et al (2014) 3 tesla proton MRI for the diagnosis of pneumonia/lung infiltrates in neutropenic patients with acute myeloid leukemia: initial results in comparison to HRCT. Eur J Radiol 83:e61–e66
Hansell DM, Bankier AA, MacMahon H et al (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 246:697–722
Montella S, Santamaria F, Salvatore M (2009) Assessment of chest high-field magnetic resonance imaging in children and young adults with noncystic fibrosis chronic lung disease: comparison to high-resolution computed tomography and correlation with pulmonary function. Investig Radiol 44:532–538
Sodhi KS, Sharma M, Lee EY et al (2018) Diagnostic utility of 3T lung MRI in children with interstitial lung disease: a prospective pilot study. Acad Radiol 25:380–386
Lutterbey G, Grohé C, Gieseke J et al (2007) Initial experience with lung-MRI at 3.0 T: comparison with CT and clinical data in the evaluation of interstitial lung disease activity. Eur J Radiol 61:256–261
Montella S, Santamaria F, Salvatore M et al (2009) Lung disease assessment in primary ciliary dyskinesia: a comparison between chest high-field magnetic resonance imaging and high-resolution computed tomography findings. Ital J Pediatr 35:24
Fink C, Puderbach M, Biederer J et al (2007) Lung MRI at 1.5 and 3 tesla: observer preference study and lesion contrast using five different pulse sequences. Investig Radiol 42:377–383
Sodhi KS, Khandelwal N, Saxena AK et al (2016) Rapid lung MRI in children with pulmonary infections: time to change our diagnostic algorithms. J Magn Reson Imaging 43:1196–1206
Dournes G, Yazbek J, Benhassen W et al (2018) 3D ultrashort echo time MRI of the lung using stack-of-spirals and spherical k-space coverages: evaluation in healthy volunteers and parenchymal diseases. J Magn Reson Imaging 48:1489–1497
Acknowledgments
The authors acknowledge Ms. Kusum Chopra and Mr. Ramesh Goel for statistical analysis of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 9 kb)
Rights and permissions
About this article
Cite this article
Rana, P., Sodhi, K.S., Bhatia, A. et al. Diagnostic accuracy of 3-T lung magnetic resonance imaging in human immunodeficiency virus-positive children. Pediatr Radiol 50, 38–45 (2020). https://doi.org/10.1007/s00247-019-04523-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04523-0