Abstract
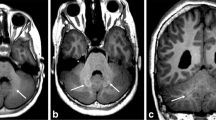
Gadolinium-based contrast agents (GBCAs) are widely used in medical imaging, with greater than 300 million doses administered since their introduction. The risk of adverse reactions is very low, and GBCAs were thought to be very safe until the discovery of nephrogenic systemic fibrosis (NSF). Since that time, gadolinium has been found to deposit throughout the body, including the brain, where it is visible on non-contrast T1-weighted MR images in people with normal renal function. The clinical effects of this deposition remain unknown and may not exist. In this review the authors provide a comprehensive update on GBCAs and their potential risks, within a historical context and through the lens of a pediatric radiologist.

Similar content being viewed by others
References
Runge VM (2016) Safety of the gadolinium-based contrast agents for magnetic resonance imaging, focusing in part on their accumulation in the brain and especially the dentate nucleus. Investig Radiol 51:273–279
Gulani V, Calamante F, Shellock FG et al (2017) Gadolinium deposition in the brain: summary of evidence and recommendations. Lancet Neurol 16:564–570
Runge VM, Stewart RG, Clanton JA et al (1983) Work in progress: potential oral and intravenous paramagnetic NMR contrast agents. Radiology 147:789–791
Adding LC, Bannenberg GL, Gustafsson LE (2001) Basic experimental studies and clinical aspects of gadolinium salts and chelates. Cardiovasc Drug Rev 19:41–56
Fraum TJ, Ludwig DR, Bashir MR, Fowler KJ (2017) Gadolinium-based contrast agents: a comprehensive risk assessment. J Magn Reson Imaging 46:338–353
Port M, Idée JM, Medina C et al (2008) Efficiency, thermodynamic and kinetic stability of marketed gadolinium chelates and their possible clinical consequences: a critical review. Biometals 21:469–490
Trout AT, Dillman JR, Ellis JH et al (2011) Patterns of intravenous contrast material use and corticosteroid premedication in children — a survey of Society of Chairs of Radiology in Children’s Hospitals (SCORCH) member institutions. Pediatr Radiol 41:1272–1283
Schueller-Weidekamm C, Lodemann KP, Grisar J et al (2013) Contrast-enhanced MR imaging of hand and finger joints in patients with early rheumatoid arthritis: do we really need a full dose of gadobenate dimeglumine for assessing synovial enhancement at 3T? Radiology 268:161–169
Runge V (2017) Critical questions regarding gadolinium deposition in the brain and body after injections of the gadolinium-based contrast agents, safety, and clinical recommendations in consideration of the EMA’s pharmacovigilance and risk assessment committee recommendation for suspension of the marketing authorizations for 4 linear agents. Investig Radiol 52:317–323
U.S. Food and Drug Administration (2004) Drug approval package: MultiHance. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2004/021357_021358_Multihance.cfm. Accessed 15 Aug 2017
Dillman JR, Ellis JH, Cohan RH et al (2007) Frequency and severity of acute allergic-like reactions to gadolinium-containing i.v. contrast media in children and adults. AJR Am J Roentgenol 189:1533–1538
Behzadi AH, Zhao Y, Farooq Z, Prince MR (2018) Immediate allergic reactions to gadolinium-based contrast agents: a systematic review and meta-analysis. Radiology 286:731
American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice (2016) Committee opinion no. 656: guidelines for diagnostic imaging during pregnancy and lactation. Obstet Gynecol 127:e75–e80
Jingu A, Fukuda J, Taketomi-Takahashi A, Tsushima Y (2014) Breakthrough reactions of iodinated and gadolinium contrast media after oral steroid premedication protocol. BMC Med Imaging 14:34
Dillman JR, Ellis JH, Cohan RH et al (2008) Allergic-like breakthrough reactions to gadolinium contrast agents after corticosteroid and antihistamine premedication. AJR Am J Roentgenol 190:187–190
Webb JA, Thomsen HS, Morcos SK et al (2005) The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol 15:1234–1240
Oh KY, Roberts VH, Schabel MC et al (2015) Gadolinium chelate contrast material in pregnancy: fetal biodistribution in the nonhuman primate. Radiology 276:110–118
Ray JG, Vermeulen MJ, Bharatha A et al (2016) Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA 316:952–961
American College of Radiology (2017) Manual on contrast media version 10.3. https://www.acr.org/Clinical-Resources/Contrast-Manual. Accessed 12 Dec 2017
Grobner T (2006) Gadolinium: a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 21:1104–1108
U.S. Food and Drug Administration (2007) Public health advisory: gadolinium-containing contrast agents for magnetic resonance imaging (MRI) — Omniscan, OptiMARK, Magnevist, ProHance, and MultiHance. http://waybackarchive-itorg/7993/20161022205104/http://wwwfdagov/NewsEvents/Newsroom/PressAnnouncements/2007/ucm108919htm. Accesssed 01 May 2018
Wang Y, Alkasab TK, Narin O et al (2011) Incidence of nephrogenic systemic fibrosis after adoption of restrictive gadolinium-based contrast agent guidelines. Radiology 260:105–112
Altun E, Martin DR, Wertman R et al (2009) Nephrogenic systemic fibrosis: change in incidence following a switch in gadolinium agents and adoption of a gadolinium policy — report from two U.S. universities. Radiology 253:689–696
Nardone B, Saddleton E, Laumann AE et al (2014) Pediatric nephrogenic systemic fibrosis is rarely reported: a RADAR report. Pediatr Radiol 44:173–180
European Medicines Agency (2017) Gadolinium-containing contrast agents. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Gadolinium-containing_contrast_agents/human_referral_000182.jsp. Accessed 15 Sept 2017
Huckle JE, Altun E, Jay M, Semelka RC (2016) Gadolinium deposition in humans: when did we learn that gadolinium was deposited in vivo? Investig Radiol 51:236–240
Darrah TH, Prutsman-Pfeiffer JJ, Poreda RJ et al (2009) Incorporation of excess gadolinium into human bone from medical contrast agents. Metallomics 1:479–488
White GW, Gibby WA, Tweedle MF (2006) Comparison of Gd(DTPA-BMA) (Omniscan) versus Gd(HP-DO3A) (ProHance) relative to gadolinium retention in human bone tissue by inductively coupled plasma mass spectroscopy. Investig Radiol 41:272–278
Gibby WA, Gibby KA, Gibby WA (2004) Comparison of Gd DTPA-BMA (Omniscan) versus Gd HP-DO3A (ProHance) retention in human bone tissue by inductively coupled plasma atomic emission spectroscopy. Investig Radiol 39:138–142
Kanda T, Ishii K, Kawaguchi H et al (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841
Adin ME, Kleinberg L, Vaidya D et al (2015) Hyperintense dentate nuclei on T1-weighted MRI: relation to repeat gadolinium administration. AJNR Am J Neuroradiol 36:1859–1865
McDonald RJ, McDonald JS, Kallmes DF et al (2015) Intracranial gadolinium deposition after contrast-enhanced MR imaging. Radiology 275:772–782
Robert P, Lehericy S, Grand S et al (2015) T1-weighted hypersignal in the deep cerebellar nuclei after repeated administrations of gadolinium-based contrast agents in healthy rats: difference between linear and macrocyclic agents. Investig Radiol 50:473–480
Ramalho J, Castillo M, Alobaidy M et al (2015) High signal intensity in globus pallidus and dentate nucleus on unenhanced T1-weighted MR images: evaluation of two linear gadolinium-based contrast agents. Radiology 276:836–844
Robert P, Violas X, Grand S et al (2016) Linear gadolinium-based contrast agents are associated with brain gadolinium retention in healthy rats. Investig Radiol 51:73–82
Jost G, Lenhard DC, Sieber MA (2016) Signal increase on unenhanced T1-weighted images in the rat brain after repeated, extended doses of gadolinium-based contrast agents: comparison of linear and macrocyclic agents. Investig Radiol 51:83–89
Kanda T, Osawa M, Oba H et al (2015) High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology 275:803–809
Radbruch A, Weberling LD, Kieslich PJ et al (2015) Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 275:783–791
Cao Y, Huang DQ, Shih G, Prince MR (2016) Signal change in the dentate nucleus on T1- weighted MR images after multiple administrations of gadopentetate dimeglumine versus gadobutrol. AJR Am J Roentgenol 206:414–419
Weberling LD, Kieslich PJ, Kickingereder P et al (2015) Increased signal intensity in the dentate nucleus on unenhanced T1-weighted images after gadobenate dimeglumine administration. Investig Radiol 50:743–748
Stojanov DA, Aracki-Trenkic A, Vojinovic S et al (2016) Increasing signal intensity within the dentate nucleus and globus pallidus on unenhanced T1W magnetic resonance images in patients with relapsing-remitting multiple sclerosis: correlation with cumulative dose of a macrocyclic gadolinium-based contrast agent, gadobutrol. Eur Radiol 26:807–815
Runge VM (2015) Macrocyclic versus linear gadolinium chelates. Investig Radiol 50:811
Agris J, Pietsch H, Balzer T (2016) What evidence is there that gadobutrol causes increasing signal intensity within the dentate nucleus and globus pallidus on unenhanced T1W MRI in patients with RRMS? Eur Radiol 26:816–817
Radbruch A, Weberling LD, Kieslich PJ et al (2015) High-signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted images: evaluation of the macrocyclic gadolinium-based contrast agent gadobutrol. Investig Radiol 50:805–810
Bjørnerud A, Vatnehol SAS, Larsson C et al (2017) Signal enhancement of the dentate nucleus at unenhanced MR imaging after very high cumulative doses of the macrocyclic gadolinium-based contrast agent gadobutrol: an observational study. Radiology 285:434–444
Hu HH, Pokorney A, Towbin RB, Miller JH (2016) Increased signal intensities in the dentate nucleus and globus pallidus on unenhanced T1-weighted images: evidence in children undergoing multiple gadolinium MRI exams. Pediatr Radiol 46:1590–1598
Roberts DR, Holden KR (2016) Progressive increase of T1 signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images in the pediatric brain exposed to multiple doses of gadolinium contrast. Brain Dev 38:331–336
Roberts DR, Chatterjee AR, Yazdani M et al (2016) Pediatric patients demonstrate progressive T1-weighted hyperintensity in the dentate nucleus following multiple doses of gadolinium-based contrast agent. AJNR Am J Neuroradiol 37:2340–2347
Rossi Espagnet MC, Bernardi B, Pasquini L et al (2017) Signal intensity at unenhanced T1-weighted magnetic resonance in the globus pallidus and dentate nucleus after serial administrations of a macrocyclic gadolinium-based contrast agent in children. Pediatr Radiol 47:1345–1352
Tibussek D, Rademacher C, Caspers J et al (2017) Gadolinium brain deposition after macrocyclic gadolinium administration: a pediatric case-control study. Radiology 285:223–230
Radbruch A, Haase R, Kickingereder P et al (2017) Pediatric brain: no increased signal intensity in the dentate nucleus on unenhanced T1-weighted MR images after consecutive exposure to a macrocyclic gadolinium-based contrast agent. Radiology 283:828–836
Schneider GK, Stroeder J, Roditi G et al (2017) T1 signal measurements in pediatric brain: findings after multiple exposures to gadobenate dimeglumine for imaging of nonneurologic disease. AJNR Am J Neuroradiol 38:1799–1806
Kanda T, Oba H, Toyoda K et al (2016) Brain gadolinium deposition after administration of gadolinium-based contrast agents. Jpn J Radiol 34:3–9
Murata N, Gonzalez-Cuyar LF, Murata K et al (2016) Macrocyclic and other non-group 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue: preliminary results from 9 patients with normal renal function. Investig Radiol 51:447–453
Lancelot E (2016) Revisiting the pharmokinetic profiles of gadolinium-based contrast agents: differences in long term biodistribution and excretion. Investig Radiol 51:691–700
Zhang Y, Cao Y, Shih GL et al (2017) Extent of signal hyperintensity on unenhanced T1-weighted brain MR images after more than 35 administrations of linear gadolinium-based contrast agents. Radiology 282:516–525
Radbruch A, Weberling LD, Kieslich PJ et al (2016) Intraindividual analysis of signal intensity changes in the dentate nucleus after consecutive serial applications of linear and macrocyclic gadolinium-based contrast agents. Investig Radiol 51:683–690
Smith AP, Marino M, Roberts J et al (2017) Clearance of gadolinium from the brain with no pathologic effect after repeated administration of gadodiamide in healthy rates: an analytical and histologic study. Radiology 282:743–751
Rasschaert M, Idee JM, Robert P et al (2017) Moderate renal failure accentuates T1 signal enhancement in the deep cerebellar nuclei of gadodiamide-treated rats. Investig Radiol 52:255–264
Kanda T, Fukosato T, Matsuda M et al (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectrometry. Radiology 276:228–232
Frenzel T, Apte C, Jost G et al (2017) Quantification and assessment of the chemical form of residual gadolinium in the brain after repeated administration of gadolinium based contrast agents: comparative study in rats. Investig Radiol 52:396–404
Popescu BF, Nichol H (2011) Mapping brain metals to evaluate therapies for neurodegenerative disease. CNS Neurosci Ther 17:256–268
Popescu BF, Robinson CA, Rajput A et al (2009) Iron, copper, and zinc distribution of the cerebellum. Cerebellum 8:74–79
Aoki I, Wu YJ, Silva AC et al (2004) In vivo detection of neuroarchitecture in the rodent brain using manganese-enhanced MRI. NeuroImage 22:1046–1059
Iliff JJ, Wang M, Liao Y et al (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid. Sci Transl Med 4:147ra111
Iliff JJ, Lee H, Yu M et al (2013) Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest 123:1299–1309
Louveau A, Smirnov I, Keyes TJ et al (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523:337–341
Iliff JJ, Goldman SA, Nedergaard M (2015) Implications of the discovery of brain lymphatic pathways. Lancet Neurol 14:977–979
Rai AT, Hogg JP (2001) Persistence of gadolinium in CSF: a diagnostic pitfall in patients with end-stage renal disease. AJNR Am J Neuroradiol 22:1357–1361
Naganawa S, Nakane T, Kawai H, Taoka T (2017) Gd-based contrast enhancement of the perivascular spaces in the basal ganglia. Magn Reson Med Sci 16:61–65
U.S. Food and Drug Administration (2017) FDA drug safety communication: FDA evaluating the risk of brain deposits with repeated use of gadolinium-based contrast agents for magnetic resonance imaging (MRI). https://www.fda.gov/Drugs/DrugSafety/ucm455386.htm. Accessed 14 Aug 2017
Mithal LB, Patel PS, Mithal D et al (2017) Use of gadolinium-based magnetic resonance imaging contrast agents and awareness of brain gadolinium deposition among pediatric providers in North America. Pediatr Radiol 47:657–664
Malayeri AA, Brooks KM, Bryant LH et al (2016) National Institutes of Health perspective on reports of gadolinium deposition in the brain. J Am Coll Radiol 13:237–241
American College of Radiology, American Society of Neuroradiology (2016) ACR-ASNR position statement on the use of gadolinium contrast agents. https://www.asnr.org/wp-content/uploads/2017/03/ACR_ASNR_Position_Statement_on_the_Use_of_Gadolinium_Contrast_Agents.pdf. Accessed 14 Aug 2017
American College of Radiology (2017) ACR response to the European PRAC recommendations. http://www.publicnow.com/view/DA714236788989CE92F38E18EA3CCB6FCC9DFDE3?2017-04-04-17:31:30+01:00-xxx935. Accessed 01 May 2018
U.S. Food and Drug Administration (2017) FDA identifies no harmful effects to date with brain retention of gadolinium-based contrast agents for MRIs; review to continue. https://www.fda.gov/downloads/drugs/drugsafety/ucm559654.pdf. Accessed 14 Aug 2017
European Medicines Agency (2017) EMA’s final opinion confirms restrictions on use of linear gadolinium agents in body scans. http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2017/07/news_detail_002780.jsp&mid=WC0b01ac058004d5c1. Accessed 14 Aug 2017
Firth S (2017) FDA panel backs new warning for gadolinium contrast agents. MedPage Today. https://www.medpagetoday.com/radiology/diagnosticradiology/67811. Accessed 17 Sept 2017
Welk B, McArthur E, Morrow SA et al (2016) Association between gadolinium contrast exposure and the risk of parkinsonism. JAMA 316:96–98
Forslin Y, Shams S, Hashim F et al (2017) Retention of gadolinium-based contrast agents in multiple sclerosis: retrospective analysis of an 18-year longitudinal study. AJNR Am J Neuroradiol 38:1311–1316
McDonald RJ, McDonald JS, Kallmes DF et al (2017) Gadolinium deposition in human brain tissues after contrast-enhanced MR imaging in adult patients without intracranial abnormalities. Radiology 285:546–554
Semelka RC, Ramalho J, Vakharia A et al (2016) Gadolinium deposition disease: initial description of a disease that has been around for a while. Magn Reson Imaging 34:1383–1390
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Podberesky disclosed the following: consultant for Guerbet; speaker’s bureau for Canon Medical Systems USA (formerly Toshiba America Medical Systems), travel reimbursement from GE Healthcare, Siemens, and Philips; author royalties from Elsevier. Dr. Rozenfeld has nothing to disclose.
Rights and permissions
About this article
Cite this article
Rozenfeld, M.N., Podberesky, D.J. Gadolinium-based contrast agents in children. Pediatr Radiol 48, 1188–1196 (2018). https://doi.org/10.1007/s00247-018-4165-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4165-1