Abstract
Background
The diagnosis of primary pulmonary tuberculosis (PTB) in children relies heavily on the radiographic demonstration of mediastinal lymphadenopathy. Plain radiographs may be unreliable and CT is the current ‘gold standard’ for demonstrating this. Only two previous studies have described the CT findings of mediastinal adenopathy exclusively in children.
Objective
To determine the prevalence, distribution, characteristics and effect on the bronchial tree of mediastinal lymphadenopathy using modern CT techniques, in children suspected of PTB.
Materials and methods
One hundred children (54 boys, 46 girls) with clinically suspected PTB were prospectively recruited from an overnight admission ward if they met the WHO criteria for suspected PTB. CT scans were evaluated by a panel of radiologists with regard to a predetermined set of criteria.
Results
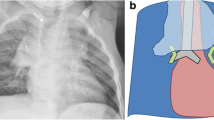
Lymph nodes were present in 92 patients, and nodes greater than 1 cm were present in 46 patients. Enhancement of lymph nodes was present in 67 patients and was almost invariably ‘ghost-like’ ring enhancement. Calcification was present in only 9 patients. The most common location for lymphadenopathy was the subcarinal position (n=90), followed by the hila (n=85; left 74, right 72, bilateral 61), the anterior mediastinum (n=79), the precarinal position (n=64) and the right paratracheal position (n=63). Multiple sites of involvement were present in 88 patients, and a single site for lymphadenopathy (subcarinal) was present in only 4 patients. Bronchial compression was identified in 29 patients. Most commonly, the left main bronchus was involved (n=21), followed by the right main bronchus (n=14) and the bronchus intermedius (n=8), 16 right-sided compressions in total.
Conclusions
Lymphadenopathy was common, but only 46 patients had lymph nodes greater than 1 cm. Enhancement characteristics of tuberculous adenopathy differ from that described previously. Typical enhancement was ‘ghost-like’ rather than discreet ring enhancing with a low-density centre. The site most frequently involved by nodes also differs from previous studies. The subcarinal region should be the site receiving most attention for the identification of lymphadenopathy, as this is most frequently involved and is also the site of the largest lymph-node masses. The presence of lymph-node groups at other recognised sites adds confidence when there is doubt, as multifocal involvement is common. Approximately one-quarter of patients with hilar adenopathy may have bronchial compression in childhood.

Similar content being viewed by others
References
Andronikou S, Welman CJ, Kader E (2002) The CT features of abdominal tuberculosis in children. Pediatr Radiol 32:75–81
Lamont AC, Cremin BJ, Pelteret RM (1986) Radiological patterns of pulmonary TB in the paediatric age group. Pediatr Radiol 16:2–7
Salazar GE, Schmitz TL, Cama R, et al (2001) Pulmonary tuberculosis in children in a developing country. Pediatrics 108:448–453
Schaaf HS, Beyers N, Gie RP, et al (1995) Respiratory tuberculosis in childhood: the diagnostic value of clinical features and special investigations. Pediatr Infect Dis J 14:189–194
Correa AG (1997) Unique aspects of tuberculosis in the pediatric population. Clin Chest Med 18:89–98
Agrons GA, Markowitz RI, Kramer SS (1993) Pulmonary tuberculosis in children. Semin Roentgenol 28:158–172
Parisi MT, Jensen MC, Wood BP (1994) Pictorial review of the usual and unusual roentgen manifestations of childhood tuberculosis. Clin Imaging 18:149–154
Leung AN, Muller NL, Pineda PR, et al (1992) Primary tuberculosis in childhood: radiographic manifestations. Radiology 182:87–91
Desai SS (1994) Early diagnosis of spinal tuberculosis by MRI. J Bone Joint Surg Br 76:863–869
Neu N, Saiman L, San Gabriel P, et al (1999) Diagnosis of pediatric tuberculosis in the modern era. Pediatr Infect Dis J 18:122–126
Schaaf HS, Gie RP, Beyers N, et al (1993) Tuberculosis in infants less than three months of age. Arch Dis Child 69:371–374
Palmer PE (1979) Pulmonary tuberculosis—usual and unusual radiographic presentations. Semin Roentgenol 14:204–243
Harisinghani MG, McLoud TC, Shepard JO, et al (2000) Tuberculosis from head to toe. Radiographics 20:449–470
Delacourt C, Mani TM, Bonnerot V, et al (1993) Computed tomography with a normal chest radiograph in tuberculous infection. Arch Dis Child 69:430–432
Kim WS, Moon WK, Kim IO, et al (1997) Pulmonary tuberculosis in children: evaluation with CT. AJR 168:1005–1009
Du Toit G, Swingler G, Iloni K (2002) Observer variation in detecting lymphadenopathy on chest radiography. Int J Tuberc Lung Dis 6:814–817
Gulati M, Suri S, Kaur G, et al (1994) CT manifestations of tubercular mediastinal lymphadenopathy. Indian J Chest Dis Allied Sci 36:3–7
Department of Health, Republic of South Africa (1999) Epidemiological comments, vol 1, no. 2. Notifiable medical conditions, June 1999
World Health Organisation (1983) The worldwide magnitude of protein-energy malnutrition: an overview from the World Health Organisation. Provisional guidelines for the diagnosis and classification of the EPI target diseases for primary health care, surveillance and special studies. EPI/GEN/83/4. World Health Organisation, Geneva
Andronikou S (2002) Pathological correlation of CT-detected mediastinal lymphadenopathy in children: the lack of size threshold criteria for abnormality. Pediatr Radiol 32:912
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andronikou, S., Joseph, E., Lucas, S. et al. CT scanning for the detection of tuberculous mediastinal and hilar lymphadenopathy in children. Pediatr Radiol 34, 232–236 (2004). https://doi.org/10.1007/s00247-003-1117-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-003-1117-0