Abstract
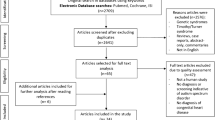
Millions of children and adults are living with congenital heart disease (CHD). Their risk for behavioral problems has not been the subject of a meta-analysis. We performed a systematic review and meta-analysis of measures of behavioral problems in people born with CHD compared to peers without CHD. We searched Pubmed, CINAHL, Embase, PsycInfo, and the Cochrane Library from January 1, 1986 to November 15, 2021. We included studies that reported a measure of behavioral problems in patients with CHD in children and adults older than 3 years of age. We screened 26,343 search results, and 24 studies met inclusion criteria. The quality of evidence was generally low. Subjects with CHD had a small increase in internalizing problems [standardized mean difference (SMD): 0.198, p = 0.02] and total behavior problems (SMD: 0.287, p = 0.013), but no difference in externalizing behavioral problems. There was significant heterogeneity in all three domains of behavior problems analyzed, and it could not be explained by variables such as age, severity, assessor, or assessment tool. There are small increases in parent- and self-reported overall behavioral problems and internalizing problems in patients with CHD compared to healthy controls. Wide confidence intervals in the meta-analyses leave open the possibility that certain factors may increase the risk of behavioral problems in this group, and future studies with important attention paid to potential confounders may help identify risk factors.




Similar content being viewed by others
Data Availability
All data used in the generation of the findings in this paper will be made immediately available upon request.
References
Hoffman J (2013) The global burden of congenital heart disease. Cardiovasc J Afr 24(4):141–145
Best KE, Rankin J (2016) Long-term survival of individuals born with congenital heart disease: a systematic review and meta-analysis. J Am Heart Assoc 5(6):e002846
Gilboa SM, Devine OJ, Kucik JE et al (2016) Congenital heart defects in the united states: estimating the magnitude of the affected population in 2010. Circulation 134(2):101–109
Calderon J, Willaime M, Lelong N et al (2018) Population-based study of cognitive outcomes in congenital heart defects. Arch Dis Child 103(1):49
Cohen S, Earing MG (2018) Neurocognitive impairment and its long-term impact on adults with congenital heart disease. Prog Cardiovasc Dis 61(3):287–293
Zaidi S, Brueckner M (2017) Genetics and genomics of congenital heart disease. Circ Res 120(6):923–940
Wallenstein MB, Harper LM, Odibo AO et al (2012) Fetal congenital heart disease and intrauterine growth restriction: a retrospective cohort study. J Matern Fetal Neonatal Med 25(6):662–665
Licht DJ, Wang J, Silvestre DW et al (2004) Preoperative cerebral blood flow is diminished in neonates with severe congenital heart defects. J Thorac Cardiovasc Surg 128(6):841–849
Thommessen M, Heiberg A, Kase BF (1992) Feeding problems in children with congenital heart disease: the impact on energy intake and growth outcome. Eur J Clin Nutr 46(7):457–464
Warner DO, Zaccariello MJ, Katusic SK et al (2018) Neuropsychological and behavioral outcomes after exposure of young children to procedures requiring general anesthesia: the mayo anesthesia safety in kids (MASK) study. Anesthesiology 129(1):89–105
Sun LS, Li G, Miller TLK et al (2016) Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA 315(21):2312–2320
Ghandour RM, Sherman LJ, Vladutiu CJ et al (2019) Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr 206:256-267.e253
Castro E, Cotov M, Brovedani P et al (2020) Associations between learning and behavioral difficulties in second-grade children. Children (Basel). 7(9):112
Hukkelberg S, Keles S, Ogden T, Hammerstrøm K (2019) The relation between behavioral problems and social competence: a correlational Meta-analysis. BMC Psychiatry 19(1):354. https://doi.org/10.1186/s12888-019-2343-9
Poton WL, Soares ALG, Gonçalves H (2018) Internalizing and externalizing behavior problems and substance use in adolescence. Cad Saude Publica 34(9):e00205917
Klein RG, Mannuzza S, Olazagasti MA et al (2012) Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry 69(12):1295–1303
Stout KK, Daniels CJ, Aboulhosn JA et al (2019) 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation 139(14):e698–e800
Oates RK, Turnbull JA, Simpson JM et al (1994) Parent and teacher perceptions of child behaviour following cardiac surgery. Acta Paediatr 83(12):1303–1307
Bellinger DC, Newburger JW, Wypij D, Kuban KC, duPlesssis AJ, Rappaport LA (2009) Behaviour at eight years in children with surgically corrected transposition: the boston circulatory arrest trial. Cardiol Young 19(1):86–97
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Campbell SB (1995) Behavior problems in preschool children: a review of recent research. J Child Psychol Psychiatry 36(1):113–149
Dipchand AI (2018) Current state of pediatric cardiac transplantation. Ann Cardiothorac Surg 7(1):31–55
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Freeman S, Sutton A. Identifying publication bias in meta-analyses of continuous outcomes. July 2020. Accessed April 29, 2022. https://training.cochrane.org/resource/identifying-publication-bias-meta-analyses-continuous-outcomes
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805
Ernst MM, Marino BS, Cassedy A et al (2018) Biopsychosocial predictors of quality of life outcomes in pediatric congenital heart disease. Pediatr Cardiol 39(1):79–88
Fredriksen PM, Diseth TH, Thaulow E (2009) Children and adolescents with congenital heart disease: assessment of behavioural and emotional problems. Eur Child Adolesc Psychiatry 18(5):292–300
Gaynor JW, Nord AS, Wernovsky G et al (2009) Apolipoprotein E genotype modifies the risk of behavior problems after infant cardiac surgery. Pediatrics 124(1):241
Goldberg CS, Hu C, Brosig C et al (2019) Behavior and quality of life at 6 years for children with hypoplastic left heart syndrome. Pediatrics 144(5):e20191010
Harrison TM (2013) Autonomic nervous system function, child behavior, and maternal sensitivity in three-year-old children with surgically corrected transposition. Heart Lung 42(6):414–421
Jackson JL, Gerardo GM, Monti JD, Schofield KA, Vannatta K (2018) Executive function and internalizing symptoms in adolescents and young adults with congenital heart disease: the role of coping. J Pediatr Psychol 43(8):906–915
Liu M, Yang L (1992) Neuropsychological and behavioral status of children with congenital heart diseases. Zhonghua Shen Jing Jing Shen Ke Za Zhi. 25(3):160-164.191
Miatton M, De Wolf D, Francois K, Thiery E, Vingerhoets G (2007) Behavior and self-perception in children with a surgically corrected congenital heart disease. J Dev Behav Pediatr 28(4):294–301
Sarrechia I, De Wolf D, Miatton M et al (2015) Neurodevelopment and behavior after transcatheter versus surgical closure of secundum type atrial septal defect. J Pediatr 166(1):31–38
Sarrechia I, Miatton M, De Wolf D et al (2016) Neurocognitive development and behaviour in school-aged children after surgery for univentricular or biventricular congenital heart disease. Eur J Cardiothorac Surg 49(1):167–174
Sarrechia I, Miatton M, Francois K et al (2015) Neurodevelopmental outcome after surgery for acyanotic congenital heart disease. Res Dev Disabil 45–46:58–68
Simons JS, Glidden R, Sheslow D, Pizarro C (2010) Intermediate neurodevelopmental outcome after repair of ventricular septal defect. Ann Thorac Surg 90(5):1586–1591
Spijkerboer AW, Utens EMWJ, Bogers AJJC, Verhulst FC, Helbing WA (2008) Long-term intellectual functioning and school-related behavioural outcomes in children and adolescents after invasive treatment for congenital heart disease. Br J Dev Psychol 26(4):457–470
Sterken C, Lemiere J, Van den Berghe G, Mesotten D (2016) Neurocognitive development after pediatric heart surgery. Pediatrics. https://doi.org/10.1542/peds.2015-4675
Utens EM, Verhulst FC, Duivenvoorden HJ, Meijboom FJ, Erdman RA, Hess J (1998) Prediction of behavioural and emotional problems in children and adolescents with operated congenital heart disease. Eur Heart J 19(5):801–807
Wright M, Nolan T (1994) Impact of cyanotic heart disease on school performance. Arch Dis Child 71(1):64–70
Chang LY, Wang CC, Weng WC, Chiu SN, Chang HY (2021) Age differences in the mediating effects of parenting stress on the relationship between cyanotic congenital heart disease and externalizing problems in children and adolescents. J Cardiovasc Nurs 36(3):293–303
Brosig CL, Bear L, Allen S et al (2017) Preschool neurodevelopmental outcomes in children with congenital heart disease. J Pediatr 183:80-86.e81
Karl TR, Hall S, Ford G et al (2004) Arterial switch with full-flow cardiopulmonary bypass and limited circulatory arrest: neurodevelopmental outcome. J Thorac Cardiovasc Surg 127(1):213–222
McCusker CG, Armstrong MP, Mullen M, Doherty NN, Casey FA (2013) A sibling-controlled, prospective study of outcomes at home and school in children with severe congenital heart disease. Cardiol Young 23(4):507–516
McCusker CG, Doherty NN, Molloy B et al (2007) Determinants of neuropsychological and behavioural outcomes in early childhood survivors of congenital heart disease. Arch Dis Child 92(2):137–141
Quartermain MD, Ittenbach RF, Flynn TB et al (2010) Neuropsychological status in children after repair of acyanotic congenital heart disease. Pediatrics 126(2):e351-359
Schaefer C, von Rhein M, Knirsch W et al (2013) Neurodevelopmental outcome, psychological adjustment, and quality of life in adolescents with congenital heart disease. Dev Med Child Neurol 55(12):1143–1149
Gothelf D, Gruber R, Presburger G et al (2003) Methylphenidate treatment for attention-deficit/hyperactivity disorder in children and adolescents with velocardiofacial syndrome: an open-label study. J Clin Psychiatry 64(10):1163–1169
Mahle WT, Clancy RR, Moss EM et al (2000) Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with hypoplastic left heart syndrome. Pediatrics 105:1082–1089
Kirshbom PM, Flynn TB, Clancy RR et al (2005) Late neurodevelopmental outcomes after repair of total anomalous pulmonary venous connections. J Thorac Cardiovasc Surg 129:1091–1096
Acknowledgements
None
Funding
We received no funding for this work, nor do any of the authors have any funding to disclose that may have had an influence on this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests financial or otherwise to declare that are directly or indirectly related to the work in this manuscript.
Ethical approval
All ethical standards as outlined by the journal and the home institution of the authors were followed to the best of our abilities. This work did not require approval by the IRB as it involved no human subjects or data and utilized previously published, publicly available data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Finkel, G.G., Sun, L.S. & Jackson, W.M. Children with Congenital Heart Disease Show Increased Behavioral Problems Compared to Healthy Peers: A Systematic Review and Meta-Analysis. Pediatr Cardiol 44, 116–123 (2023). https://doi.org/10.1007/s00246-022-02940-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02940-x