Abstract
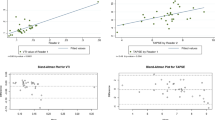
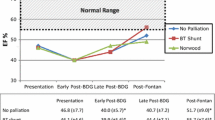
Leftward posterior deviation of the atrial septum primum (LDSP) has been reported in up to 64% of patients with hypoplastic left heart syndrome (HLHS) but there are no published data on its impact on neonatal outcomes. We reviewed the prevalence of LDSP and its correlation with neonatal outcomes in our institution. This was a single-center retrospective study of neonates with HLHS from 2001 to 2019. Echocardiograms were reviewed and the presence or absence of LDSP was noted. To quantify the degree of deviation in patients with LDSP, a new measurement, the deviation index (DI) was calculated using both the subcostal long and short-axis views. Of ninety-four patients with HLHS, fifty-seven (61%) patients were noted to have LDSP. There was no statistically significant difference in gestational age (GA), birth weight (BW), or mortality between patients with and without LDSP. Patients with LDSP had an increased incidence of unplanned reoperation (p < 0.01), post-operative cardiac catheterization (p < 0.05), and post-operative infection (p < 0.05). After correction for GA, BW, HLHS subtype, and type of surgery, LDSP predicted reoperation (OR = 3.6, p < 0.01), catheterization (OR = 2.7, p = 0.05), and infection (OR = 3.4, p < 0.05). Higher degree of deviation predicted reoperation (DI > 0.17), catheterization (DI > 0.07), and infection (DI > 0.12). There was excellent inter-observer reproducibility of the DI (ICCabsolute-agreement = 0.82, ICCconsistency = 0.90). Patients with LDSP have a higher prevalence of post-operative morbidity. The degree of deviation was found to be predictive of post-operative complications. Pre-operative echocardiographic evaluation of LDSP in patients with HLHS may be helpful in risk stratification and counseling.




Similar content being viewed by others
References
Remmell-Dow DR, Bharati S, Davis JT, Lev M, Allen HD (1995) Hypoplasia of the eustachian valve and abnormal orientation of the limbus of the foramen ovale in hypoplastic left heart syndrome. Am Heart J 130(1):148–152. https://doi.org/10.1016/0002-8703(95)90250-3
Chin AJ, Weinberg PM, Barber G (1990) Subcostal two-dimensional echocardiographic identification of anomalous attachment of septum primum in patients with left atrioventricular valve underdevelopment. J Am Coll Cardiol 15(3):678–681. https://doi.org/10.1016/0735-1097(90)90645-6
Weinberg PM (1988) Atrial septal anomlaies differentiate types of hypoplastic left heart syndrome. J Am Coll Cardiol 11:136A
Silvestri LM, Scarabotti A, Marino B (2014) Leftward displacement of septum primum in children with congenital heart disease. Pediatr Cardiol 35(1):185. https://doi.org/10.1007/s00246-013-0803-4
Park MV, Fedderly RT, Frommelt PC et al (2013) Leftward displacement of septum primum in hypoplastic left heart syndrome. Pediatr Cardiol 34(4):942–947. https://doi.org/10.1007/s00246-012-0579-y
Gaynor JW, Mahle WT, Cohen MI et al (2002) Risk factors for mortality after the Norwood procedure. Eur J Cardio-thoracic Surg 22(1):82–89. https://doi.org/10.1016/S1010-7940(02)00198-7
Feinstein J, Benson W, Dubin A et al (2020) Hypoplastic left heart syndrome current considerations and expectations. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2011.09.022
Rossi AF, Sommer RJ, Lotvin A et al (1994) Usefulness of intermittent monitoring of mixed venous oxygen saturation after stage I palliation for hypoplastic left heart syndrome. Am J Cardiol 73(15):1118–1123. https://doi.org/10.1016/0002-9149(94)90293-3
Tweddell JS, Hoffman GM, Mussatto KA et al (2002) Hypoplastic left heart syndrome: lessons learned from 115 consecutive patients. Circulation 106:82–89. https://doi.org/10.1161/01.cir.0000032878.55215.bd
Hoffman GM, Tweddell JS, Ghanayem NS et al (2004) Alteration of the critical arteriovenous oxygen saturation relationship by sustained afterload reduction after the Norwood procedure. J Thorac Cardiovasc Surg 127(3):738–745. https://doi.org/10.1016/S0022-5223(03)01315-1
Stasik CN, Goldberg CS, Bove EL, Devaney EJ, Ohye RG (2006) Current outcomes and risk factors for the Norwood procedure. J Thorac Cardiovasc Surg 131(2):412–417. https://doi.org/10.1016/j.jtcvs.2005.09.030
Srinivasan C, Sachdeva R, Morrow WR et al (2009) Standardized management improves outcomes after the Norwood procedure. Congenit Heart Dis 4(5):329–337. https://doi.org/10.1111/j.1747-0803.2009.00323.x
Lopez L, Colan SD, Frommelt PC et al (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram : a report from the pediatric measurements writing group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23(5):465–495. https://doi.org/10.1016/j.echo.2010.03.019
Cole SR, Herna MA (2008) Practice of epidemiology constructing inverse probability weights for marginal structural models. Am J Epidemiol 168(6):656–664
Chen T (2016) XGBoost : A Scalable Tree Boosting System. Doi: https://doi.org/10.1145/2939672.2939785
Jacobs JP, Mayer JE, Mavroudis C et al (2016) The society of thoracic surgeons congenital heart surgery database : 2016 update on outcomes and quality. Ann Thorac Surg 101(3):850–862. https://doi.org/10.1016/j.athoracsur.2016.01.057
Fruitman DS, Medicine F, Scotia N (2000) Hypoplastic left heart syndrome : prognosis and management options. Paediatr Child Health 5(4):219–225
Sano S, Huang S, Kasahara S, Yoshizumi K (2009) Risk factors for mortality after the Norwood procedure using right ventricle to pulmonary. ATS 87(1):178–186. https://doi.org/10.1016/j.athoracsur.2008.08.027
Hehir DA, Dominguez TE, Ballweg JA et al (2008) Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2007.12.012
Kaplinski M, Ittenbach RF, Hunt ML et al (2020) Decreasing interstage mortality after the Norwood procedure: a 30-year experience. J Am Heart Assoc. https://doi.org/10.1161/JAHA.120.016889
Hamzah M, Othman HF, Elsamny E, Agarwal H, Aly H (2020) Clinical outcomes and risk factors for in - hospital mortality in neonates with hypoplastic left heart syndrome. Pediatr Cardiol. https://doi.org/10.1007/s00246-020-02312-3
Cohen MS, Weinberg P, Coon PD, Gaynor JW, Rychik J (2001) Deviation of atrial septum primum in association with normal left atrioventricular valve size. J Am Soc Echocardiogr 14(7):732–737. https://doi.org/10.1067/mje.2001.111875
Maeda K, Yamaki S, Kado H, Asou T (2004) Hypoplasia of the small pulmonary arteries in hypoplastic left heart syndrome with restrictive atrial septal defect. Circulation 110:139–146
Taketazu M, Barrea C, Smallhorn JF, Wilson GJ, Hornberger LK (2004) Intrauterine pulmonary venous flow and restrictive foramen ovale in fetal hypoplastic left heart syndrome. J Am College Cardiol. https://doi.org/10.1016/j.jacc.2004.01.033
Vlahos A, Lock J, der McElhinney DV (2004) Hypoplastic left heart syndrome with intact or highly restrictive atrial septum outcome after neonatal transcatheter atrial septostomy. Circulation 109:2326–2330
Acknowledgements
None.
Funding
The authors received no funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gill, K., Lopez, L., Taylor, T. et al. Leftward and Posterior Deviation of the Septum Primum Predicts Morbidity in Patients with Hypoplastic Left Heart Syndrome. Pediatr Cardiol 43, 1365–1372 (2022). https://doi.org/10.1007/s00246-022-02860-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02860-w