Abstract
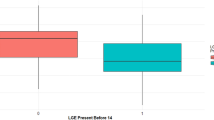
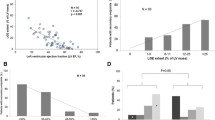
Barth Syndrome (BTHS) is an X-linked mitochondrial cardioskeletal myopathy caused by defects in TAFAZZIN, a gene responsible for cardiolipin remodeling. Altered mitochondrial levels of cardiolipin lead to cardiomyopathy (CM), muscle weakness, exercise intolerance, and mortality. Cardiac risk factors predicting outcome are unknown. Therefore, we conducted a longitudinal observational study to determine risk factors for outcome in BTHS. Subjects with minimum two evaluations (or one followed by death or transplant) were included. Cardiac size, function, and QTc data were measured by echocardiography and electrocardiography at 7 time points from 2002 to 2018. Analysis included baseline, continuous, and categorical variables. Categorical risk factors included prolonged QTc, abnormal right ventricle fractional area change (RV FAC), left ventricle (LV) or RV non-compaction, and restrictive CM phenotype. The association between variables and cardiac death or transplant (CD/TX) was assessed. Median enrollment age was 7 years (range 0.5–22; n = 44). Transplant-free survival (TFS) was 74.4% at 15 years from first evaluation. The cohort demonstrated longitudinal declines in LV size and stroke volume z-scores (end-diastolic volume, p = 0.0002; stroke volume p < 0.0001), worsening RV FAC (p = 0.0405), and global longitudinal strain (GLS) (p = 0.0001) with stable ejection (EF) and shortening (FS) fraction. CD/TX subjects (n = 9) displayed worsening LV dilation (p = 0.0066), EF (p ≤ 0.0001), FS (p = 0.0028), and RV FAC (p = .0032) versus stability in TFS. Having ≥ 2 categorical risk factors predicted CD/TX (p = 0.0073). Over 15 years, 25% of BTHS subjects progressed to CD/TX. Those with progressive LV enlargement, dysfunction, and multiple cardiac risk factors warrant increased surveillance and intense therapy.






Similar content being viewed by others
References
Vreken P, Valianpour F, Nijtmans LG, Grivell LA, Plecko B, Wanders RJ et al (2000) Defective remodeling of cardiolipin and phosphatidylglycerol in Barth syndrome. Biochem Biophys Res Commun 279(2):378–382
Barth PG, Scholte HR, Berden JA, Van der Klei-Van Moorsel JM, Luyt-Houwen IE, Van’t Veer-Korthof ET et al (1983) An X-linked mitochondrial disease affecting cardiac muscle, skeletal muscle and neutrophil leucocytes. J Neurol Sci 62(1–3):327–355
Neustein HB, Lurie PR, Dahms B, Takahashi M (1979) An X-linked recessive cardiomyopathy with abnormal mitochondria. Pediatrics 64(1):24–29
Spencer CT, Bryant RM, Day J, Gonzalez IL, Colan SD, Thompson WR et al (2006) Cardiac and clinical phenotype in Barth syndrome. Pediatrics 118(2):e337–e346
Roberts AE, Nixon C, Steward CG, Gauvreau K, Maisenbacher M, Fletcher M et al (2012) The Barth Syndrome Registry: distinguishing disease characteristics and growth data from a longitudinal study. Am J Med Genet A 158A(11):2726–2732
Rigaud C, Lebre AS, Touraine R, Beaupain B, Ottolenghi C, Chabli A et al (2013) Natural history of Barth syndrome: a national cohort study of 22 patients. Orphanet J Rare Dis 8:70
Clarke SL, Bowron A, Gonzalez IL, Groves SJ, Newbury-Ecob R, Clayton N et al (2013) Barth syndrome. Orphanet J Rare Dis 8:23
Kang SL, Forsey J, Dudley D, Steward CG, Tsai-Goodman B (2016) Clinical characteristics and outcomes of cardiomyopathy in Barth Syndrome: the UK experience. Pediatr Cardiol 37(1):167–176
Spencer CT, Byrne BJ, Bryant RM, Margossian R, Maisenbacher M, Breitenger P et al (2011) Impaired cardiac reserve and severely diminished skeletal muscle O(2) utilization mediate exercise intolerance in Barth syndrome. Am J Physiol Heart Circ Physiol 301(5):H2122–H2129
Bione S, D’Adamo P, Maestrini E, Gedeon AK, Bolhuis PA, Toniolo D (1996) A novel X-linked gene, G45 is responsible for Barth syndrome. Nat Genet 12(4):385–389
Schlame M, Towbin JA, Heerdt PM, Jehle R, DiMauro S, Blanck TJ (2002) Deficiency of tetralinoleoyl-cardiolipin in Barth syndrome. Ann Neurol 51(5):634–637
Xu Y, Phoon CK, Berno B, D’Souza K, Hoedt E, Zhang G et al (2016) Loss of protein association causes cardiolipin degradation in Barth syndrome. Nat Chem Biol 12(8):641–647
Neuwald AF (1997) Barth syndrome may be due to an acyltransferase deficiency. Curr Biol 7(8):R465–R466
Ikon N, Ryan RO (2017) Barth syndrome: connecting cardiolipin to cardiomyopathy. Lipids 52(2):99–108
Ren M, Phoon CK, Schlame M (2014) Metabolism and function of mitochondrial cardiolipin. Prog Lipid Res 55:1–16
Gonzalvez F, D’Aurelio M, Boutant M, Moustapha A, Puech JP, Landes T et al (2013) Barth syndrome: cellular compensation of mitochondrial dysfunction and apoptosis inhibition due to changes in cardiolipin remodeling linked to tafazzin (TAZ) gene mutation. Biochim Biophys Acta 1832(8):1194–1206
Claypool SM, Koehler CM (2012) The complexity of cardiolipin in health and disease. Trends Biochem Sci 37(1):32–41
Pfeiffer K, Gohil V, Stuart RA, Hunte C, Brandt U, Greenberg ML et al (2003) Cardiolipin stabilizes respiratory chain supercomplexes. J Biol Chem 278(52):52873–52880
Zhang M, Mileykovskaya E, Dowhan W (2002) Gluing the respiratory chain together. Cardiolipin is required for supercomplex formation in the inner mitochondrial membrane. J Biol Chem 277(46):43553–43556
Barth PG, Van den Bogert C, Bolhuis PA, Scholte HR, van Gennip AH, Schutgens RB et al (1996) X-linked cardioskeletal myopathy and neutropenia (Barth syndrome): respiratory-chain abnormalities in cultured fibroblasts. J Inherit Metab Dis 19(2):157–160
Dudek J, Cheng IF, Balleininger M, Vaz FM, Streckfuss-Bomeke K, Hubscher D et al (2013) Cardiolipin deficiency affects respiratory chain function and organization in an induced pluripotent stem cell model of Barth syndrome. Stem Cell Res 11(2):806–819
Xu Y, Sutachan JJ, Plesken H, Kelley RI, Schlame M (2005) Characterization of lymphoblast mitochondria from patients with Barth syndrome. Lab Invest 85(6):823–830
Bashir A, Bohnert KL, Reeds DN, Peterson LR, Bittel AJ, de Las Fuentes L et al (2017) Impaired cardiac and skeletal muscle bioenergetics in children, adolescents, and young adults with Barth syndrome. Physiol Rep 5(3):e13130
Paradies G, Paradies V, Ruggiero FM, Petrosillo G (2019) Role of cardiolipin in mitochondrial function and dynamics in health and disease: molecular and pharmacological aspects. Cells 8(7):728
Bowron A, Honeychurch J, Williams M, Tsai-Goodman B, Clayton N, Jones L et al (2015) Barth syndrome without tetralinoleoyl cardiolipin deficiency: a possible ameliorated phenotype. J Inherit Metab Dis 38(2):279–286
Miller PC, Ren M, Schlame M, Toth MJ, Phoon CKL (2020) A Bayesian analysis to determine the prevalence of barth syndrome in the pediatric population. J Pediatr 217:139–144
Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S et al (2006) Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA 296(15):1867–1876
Nugent AW, Daubeney PE, Chondros P, Carlin JB, Cheung M, Wilkinson LC et al (2003) The epidemiology of childhood cardiomyopathy in Australia. N Engl J Med 348(17):1639–1646
Hirono K, Hata Y, Nakazawa M, Momoi N, Tsuji T, Matsuoka T et al (2018) Clinical and echocardiographic impact of Tafazzin variants on dilated cardiomyopathy phenotype in left ventricular non-compaction patients in early infancy. Circ J 82(10):2609–2618
Wang J, Guo Y, Huang M, Zhang Z, Zhu J, Liu T et al (2017) Identification of TAZ mutations in pediatric patients with cardiomyopathy by targeted next-generation sequencing in a Chinese cohort. Orphanet J Rare Dis 12(1):26
Spencer CT, Byrne BJ, Gewitz MH, Wechsler SB, Kao AC, Gerstenfeld EP et al (2005) Ventricular arrhythmia in the X-linked cardiomyopathy Barth syndrome. Pediatr Cardiol 26(5):632–637
Sluysmans TCS (2009) Structural measurements and adjustment for growth. In: Lai WWCM, Geva T, Mertens L (eds) Echocardiography in pediatric and congenital heart disease. Sussex, Wiley-Blackwell
Colan SD (2016) Normal echocardiographic values for cardiovascular structures. In: Echocardiography in pediatric and congenital heart disease, pp 883–901
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ et al (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function–a study in normals and dilated cardiomyopathy. J Cardiol 26(6):357–366
Eidem BW, McMahon CJ, Cohen RR, Wu J, Finkelshteyn I, Kovalchin JP et al (2004) Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr 17(3):212–221
Cantinotti M, Giordano R, Scalese M, Murzi B, Assanta N, Spadoni I et al (2016) Nomograms for mitral inflow Doppler and tissue Doppler velocities in Caucasian children. J Cardiol 68(4):288–299
Cantinotti M, Lopez L (2013) Nomograms for blood flow and tissue Doppler velocities to evaluate diastolic function in children: a critical review. J Am Soc Echocardiogr 26(2):126–141
Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D et al (2015) Echocardiographic reference ranges for normal cardiac Doppler data: results from the NORRE Study. Eur Heart J Cardiovasc Imaging 16(9):1031–1041
Jenni R, Oechslin E, Schneider J, Attenhofer Jost C, Kaufmann PA (2001) Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart 86(6):666–671
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG et al (2009) 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 119(14):e391-479
Mazar I, Stokes J, Ollis S, Love E, Espensen A, Barth PG et al (2019) Understanding the life experience of Barth syndrome from the perspective of adults: a qualitative one-on-one interview study. Orphanet J Rare Dis 14(1):243
Towbin JA, Lorts A, Jefferies JL (2015) Left ventricular non-compaction cardiomyopathy. The Lancet 386(9995):813–825
Martinez HR, Miller E, Mead R, Osher J, Almasri M, Parent JJ (2020) Biventricular noncompaction cardiomyopathy with severe dilated phenotype in a family with a novel MYH7 gene variant. Prog Pediatr Cardiol 59:101205
Stampfli SF, Gotschy A, Kiarostami P, Ozkartal T, Gruner C, Niemann M et al (2020) Right ventricular involvement in left ventricular non-compaction cardiomyopathy. Cardiol J. https://doi.org/10.5603/CJ.a2020.0095
Nucifora G, Aquaro GD, Masci PG, Pingitore A, Lombardi M (2014) Magnetic resonance assessment of prevalence and correlates of right ventricular abnormalities in isolated left ventricular noncompaction. Am J Cardiol 113(1):142–146
Pignatelli RH, McMahon CJ, Dreyer WJ, Denfield SW, Price J, Belmont JW et al (2003) Clinical characterization of left ventricular noncompaction in children: a relatively common form of cardiomyopathy. Circulation 108(21):2672–2678
Jefferies JL, Wilkinson JD, Sleeper LA, Colan SD, Lu M, Pahl E et al (2015) cardiomyopathy phenotypes and outcomes for children with left ventricular myocardial noncompaction: results from the Pediatric Cardiomyopathy Registry. J Card Fail 21(11):877–884
Hanke SP, Gardner AB, Lombardi JP, Manning PB, Nelson DP, Towbin JA et al (2012) Left ventricular noncompaction cardiomyopathy in Barth syndrome: an example of an undulating cardiac phenotype necessitating mechanical circulatory support as a bridge to transplantation. Pediatr Cardiol 33(8):1430–1434
Webber SA, Lipshultz SE, Sleeper LA, Lu M, Wilkinson JD, Addonizio LJ et al (2012) Outcomes of restrictive cardiomyopathy in childhood and the influence of phenotype: a report from the Pediatric Cardiomyopathy Registry. Circulation 126(10):1237–1244
Lee TM, Hsu DT, Kantor P, Towbin JA, Ware SM, Colan SD et al (2017) Pediatric cardiomyopathies. Circ Res 121(7):855–873
Daubeney PE, Nugent AW, Chondros P, Carlin JB, Colan SD, Cheung M et al (2006) Clinical features and outcomes of childhood dilated cardiomyopathy: results from a national population-based study. Circulation 114(24):2671–2678
Acknowledgements
The authors thank the Barth Syndrome Foundation and the health care providers, research staff, patients, and caregivers who participated in this longitudinal observational study. Writing and editing assistance, including incorporating author feedback and manuscript submission, was provided by James A. Shiffer, RPh (Write On Time Medical Communications, LLC) and Gene Kelly (Stealth Biotherapeutics). This support was funded by Stealth Biotherapeutics.
Funding
This study received no grant funding. The Barth Syndrome Foundation funded the Barth Syndrome Registry from which retrospective data were obtained.
Author information
Authors and Affiliations
Contributions
All authors of this study participated in study design. All authors had access to the data, participated in the development and critical review of the manuscript, approved submission of the manuscript for publication, and are accountable for the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chowdhury, S., Jackson, L., Byrne, B.J. et al. Longitudinal Observational Study of Cardiac Outcome Risk Factor Prediction in Children, Adolescents, and Adults with Barth Syndrome. Pediatr Cardiol 43, 1251–1263 (2022). https://doi.org/10.1007/s00246-022-02846-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02846-8