Abstract
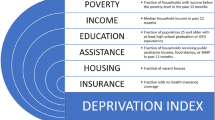
Socioeconomic status (SES) affects a range of health outcomes but has not been extensively explored in the single ventricle population. We investigate the impact of community-level deprivation on morbidity and mortality for infants with single ventricle heart disease in the first year of life. Retrospective cohort analysis of infants enrolled in the National Pediatric Cardiology Improvement Collaborative who underwent staged single ventricle palliation examining mortality and length of stay (LOS) using a community-level deprivation index (DI). 974 patients met inclusion criteria. Overall mortality was 20.5%, with 15.7% of deaths occurring between the first and second palliations. After adjusting for clinical risk factors, the DI was associated with death (log relative hazard \({\chi }_{3}^{2}\) = 8.92, p = 0.030) and death or transplant (log relative hazard \({\chi }_{3}^{2}\) = 8.62, p = 0.035) in a non-linear fashion, impacting those near the mean DI. Deprivation was associated with LOS following the first surgical palliation (S1P) (p = 0.031) and overall hospitalization during the first year of life (p = 0.018). For every 0.1 increase in the DI, LOS following S1P increased by 3.35 days (95% confidence interval 0.31–6.38) and total hospitalized days by 5.08 days (95% CI 0.88–9.27). Community deprivation is associated with mortality and LOS for patients with single ventricle congenital heart disease. While patients near the mean DI had a higher hazard of one year mortality compared to those at the extremes of the DI, LOS and DI were linearly associated, demonstrating the complex nature of SES factors.





Similar content being viewed by others
Data Availability
The de-identified data that support the findings of this study are available upon request from the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) through their standard report request process and with appropriate human subject protections assured.
Code Availability
The R codes for running the statistical analyses are available upon request from corresponding authors.
References
Ghanayem NS, Allen KR, Tabbutt S et al (2012) Interstage mortality after the Norwood procedure: results of the multicenter single ventricle reconstruction trial. J Thorac Cardiovasc Surg 144(4):896–906. https://doi.org/10.1016/j.jtcvs.2012.05.020
Carlo WF, Cnota JF, Dabal RJ et al (2017) Practice trends over time in the care of infants with hypoplastic left heart syndrome: a report from the national pediatric cardiology quality improvement collaborative. Congenit Heart Dis 12(3):315–321. https://doi.org/10.1111/chd.12442
Cross RR, Harahsheh AS, McCarter R et al (2014) Identified mortality risk factors associated with presentation, initial hospitalisation, and interstage period for the Norwood operation in a multi-centre registry: a report from the national pediatric cardiology-quality improvement collaborative. Cardiol Young 24(2):253–262. https://doi.org/10.1017/s1047951113000127
Bucholz EM, Sleeper LA, Newburger JW (2018) Neighborhood socioeconomic status and outcomes following the Norwood procedure: an analysis of the pediatric heart network single ventricle reconstruction trial public data set. J Am Heart Assoc. https://doi.org/10.1161/jaha.117.007065
Peyvandi S, Baer RJ, Moon-Grady AJ et al (2018) Socioeconomic mediators of racial and ethnic disparities in congenital heart disease outcomes: a population based study in California. J Am Heart Assoc 7(20):e010342. https://doi.org/10.1161/JAHA.118.010342
Tweddell JS, Sleeper LA, Ohye RG et al (2012) Intermediate-term mortality and cardiac transplantation in infants with single-ventricle lesions: risk factors and their interaction with shunt type. J Thorac Cardiovasc Surg 144(1):152–159. https://doi.org/10.1016/j.jtcvs.2012.01.016
Taylor LC, Burke B, Donohue JE et al (2016) Risk factors for interstage mortality following the norwood procedure: impact of sociodemographic factors. Pediatr Cardiol 37(1):68–75. https://doi.org/10.1007/s00246-015-1241-2
Kucik JE, Nembhard WN, Donohue P et al (2014) Community socioeconomic disadvantage and the survival of infants with congenital heart defects. Am J Public Health 104(11):e150–e157. https://doi.org/10.2105/AJPH.2014.302099
Chan T, Barrett CS, Tjoeng YL et al (2018) Racial variations in extracorporeal membrane oxygenation use following congenital heart surgery. J Thorac Cardiovasc Surg 156(1):306–315. https://doi.org/10.1016/j.jtcvs.2018.02.103
Anderson JB, Beekman RH 3rd, Kugler JD et al (2015) Improvement in interstage survival in a national pediatric cardiology learning network. Circ Cardiovasc Qual Outcomes 8(4):428–436. https://doi.org/10.1161/circoutcomes.115.001956
Brokamp C, Wolfe C, Lingren T et al (2017) Decentralized and reproducible geocoding and characterization of community and environmental exposures for multisite studies. J Am Med Inform Assoc 25(3):309–314. https://doi.org/10.1093/jamia/ocx128
Therneau T (2020) A package for survival analysis in R 2020. https://CRAN.R-project.org/package=survival. Accessed 12 Aug 2020
Bates D, Maechler M, Boker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Soft 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
Team RC (2020) R: a language and environment for statistical computing 4.0.0. Vienna. R Foundation for Statistical Computing, Austria
Kaplinski M, Ittenbach RF, Hunt ML et al (2020) Decreasing interstage mortality after the Norwood procedure: a 30 year experience. J Am Heart Assoc 9(19):e016889. https://doi.org/10.1161/JAHA.120.016889
Anderson BR, Fieldston ES, Newburger JW et al (2018) Disparities in outcomes and resource use after hospitalization for cardiac surgery by neighborhood income. Pediatrics 141(3):e20172432. https://doi.org/10.1542/peds.2017-2432
Dean PN, Hillman DG, McHugh KE et al (2011) Inpatient costs and charges for surgical treatment of hypoplastic left heart syndrome. Pediatrics 128(5):e1181–e1186. https://doi.org/10.1542/peds.2010-3742
White-Williams C, Rossi LP, Bittner VA et al (2020) Addressing social determinants of health in the care of patients with heart failure: a scientific statement from the American heart association. Circulation 141(22):e841–e863. https://doi.org/10.1161/cir.0000000000000767
Davey B, Sinha R, Lee JH et al (2021) Social determinants of health and outcomes for children and adults with congenital heart disease: a systematic review. Pediatr Res 89(2):275–294. https://doi.org/10.1038/s41390-020-01196-6
Butler DC, Petterson S, Phillips RL et al (2013) Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 48(2 Pt 1):539–559. https://doi.org/10.1111/j.1475-6773.2012.01449.x
Diez Roux AV, Merkin SS, Arnett D et al (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345(2):99–106. https://doi.org/10.1056/nejm200107123450205
Noelke CMN, Baek M, Huntington N et al (2021) Child Opportunity Index 2.0 Technical Documentation2020. Available from: https://www.diversitydatakids.org/sites/default/files/2020-02/ddk_coi2.0_technical_documentation_20200212.pdf
Auger KA, Kahn RS, Simmons JM et al (2017) Using address information to identify hardships reported by families of children hospitalized with asthma. Acad Pediatr 17(1):79–87. https://doi.org/10.1016/j.acap.2016.07.003
Funding
Current funding sources for National Pediatric Cardiology Quality Improvement Collaborative include (1) participation fees from enrolled centers; (2) a grant from the Children’s Heart Association of Cincinnati; (3) a federal grant to the pediatric Center for Education and Research in Therapeutics at Cincinnati Children’s Hospital Medical Center, funded by the federal Agency for Healthcare, Research and Quality [#U19HS021114 AHRQ]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SL, KS, HZ, and NO. The first draft of the manuscript was written by SL and KS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This research study was conducted retrospectively from data obtained from infants enrolled in the National Pediatric Cardiology Quality Improvement Collaborative and was in accordance with the ethical standards of our institution and with the 1964 Helsinki declaration and its later amendments of comparable ethical standards. The protocol was reviewed and approved by the IRB of Cincinnati Children’s Hospital Medical Center using an expedited review in accordance with 45 CFR 46.11(b)(1).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sarah R. de Loizaga and Kristin Schneider are considered as the co First authors.
Rights and permissions
About this article
Cite this article
de Loizaga, S.R., Schneider, K., Beck, A.F. et al. Socioeconomic Impact on Outcomes During the First Year of Life of Patients with Single Ventricle Heart Disease: An Analysis of the National Pediatric Cardiology Quality Improvement Collaborative Registry. Pediatr Cardiol 43, 605–615 (2022). https://doi.org/10.1007/s00246-021-02763-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02763-2