Abstract
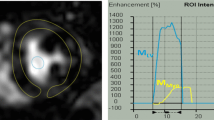
Coronary angiography remains the standard for diagnosis of cardiac transplant vasculopathy (CAV), but it is invasive. Non-invasively derived left ventricle (LV) global myocardial work (GMW) indices have not been evaluated. We aimed to assess for correlations between LV GMW and the presence of CAV in a pediatric population. 24 heart transplant patients and 24 normal controls were prospectively enrolled. Patients were age-matched into groups with: orthotopic heart transplant and CAV (OHT-CAV; 6 patients, 33% male, mean age 13.5 years [SD 4.2]), orthotopic heart transplant without CAV (OHT; 18 patients, 67% male, mean age 11.1 years [SD 4.8]), and normal healthy controls (42% male, mean age 12.8 years [SD 5.0]). Transplant patients underwent cardiac catheterization with coronary angiography within 3 months of echocardiogram. Post-processing of echocardiograms with speckle-tracking echocardiography and derivation of GMW indices was performed. OHT-CAV patients had decreased global work efficiency (GWE) compared to OHT (mean difference = 7.01 [1.76, 12.25], adjusted p < 0.01). LV global longitudinal strain (GLS) and LV ejection fraction were not different between groups. Both global work index and GWE were decreased in OHT-CAV and OHT when compared to normal controls (OHT-CAV 1311.23 mmHg% vs OHT 1426.22 mmHg% vs controls 1802.81 mmHg%, adjusted p < 0.01; OHT-CAV 83.87% vs. OHT 90.87% vs. controls 95.41%, adjusted p < 0.01). GWE correlated negatively with the presence of CAV (r = − 0.44 [− 0.72, − 0.05]). This pilot study demonstrates decreased GWE correlates with pediatric CAV. This supports the need for further investigation of this promising diagnostic tool.



Similar content being viewed by others
References
Mehra MR, Crespo-Leiro MG, Dipchand A et al (2010) International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy-2010. J Heart Lung Transplant 29(7):717–727
Rossano JW, Dipchand AI, Edwards LB et al (2016) The registry of the international society for heart and lung transplantation: nineteenth pediatric heart transplantation report-2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant 35(10):1185–1195
Miller CA, Chowdhary S, Ray SG et al (2011) Role of noninvasive imaging in the diagnosis of cardiac allograft vasculopathy. Circ Cardiovasc Imaging 4(5):583–593
Konstam MA, Abboud FM (2017) Ejection fraction: misunderstood and overrated (changing the paradigm in categorizing heart failure). Circulation 135(8):717–719
Russell K, Eriksen M, Aaberge L et al (2012) A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J 33(6):724–733
Hubert A, Le Rolle V, Leclercq C et al (2018) Estimation of myocardial work from pressure-strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging 19(12):1372–1379
Galli E, Vitel E, Schnell F et al (2019) Myocardial constructive work is impaired in hypertrophic cardiomyopathy and predicts left ventricular fibrosis. Echocardiography 36(1):74–82
Chan J, Edwards NFA, Khandheria BK et al (2019) A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 20(1):31–39
Edwards NFA, Scalia GM, Shiino K et al (2019) global myocardial work is superior to global longitudinal strain to predict significant coronary artery disease in patients with normal left ventricular function and wall motion. J Am Soc Echocardiogr 32(8):947–957
Tretter JT, Pradhan S, Truong VT, Mullikin A, Mazur W, Hill GD, Redington AN, Taylor MD (2021) Non‐invasive left ventricular myocardial work indices in healthy adolescents at rest. Int J Cardiovasc Imaging 37(8):2429–2438
Pham TTM, Truong VT, Vu PN, Tran TX, Nguyen NNH, Nguyen LPT, Tu HNT, Palmer C, Tretter JT, Levy P, Mazur W, Pham VN (2021) echocardiographic reference ranges of non-invasive myocardial work indices in children. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02695-x (PMID: 34331081)
Lopez L, Colan SD, Frommelt PC, et al. (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr. 23(5):465–495; quiz 576–467.
Team RC. R: a language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org. Published 2019. Accessed.
Harrell Frank E, Zhouwen L. Analysis of observer variability. https://biostat.app.vumc.org/wiki/Main/AnalysisOfObserverVariability
Harrell FE, Slaughter JC. Biostatistics for Biomedical Research Course Notes. http://hbiostat.org/bbr/
Efron B, Tibshirani RJ. An introduction to the bootstrap. CRC press. 1994.
Costanzo MR, Dipchand A, Starling R et al (2010) The international society of heart and lung transplantation guidelines for the care of heart transplant recipients. J Heart Lung Transpl 29(8):914–956
Kindel SJ, Hsu HH, Hussain T, Johnson JN, McMahon CJ, Kutty S (2017) Multimodality noninvasive imaging in the monitoring of pediatric heart transplantation. J Am Soc Echocardiogr 30(9):859–870
Nandi DCC, Schumacher KR, Fenton M, Singh RK, Lin KY, Conway J, Cantor RS, Koehl DA, Lamour JM, Kirklin JK, Elfriede P (2020) Surveillance for cardiac allograft vasculopathy: practice variations among 50 pediatric heart transplant centers. J Heart Lung Transplant 39(11):1260–1269
Soslow JH, Samyn MM (2019) Multi-modal imaging of the pediatric heart transplant recipient. Transl Pediatr 8(4):322–338
Auerbach SR, Fenton MJ, Grutter G, et al. The complication rate of intravascular ultrasound (IVUS) in a multicenter pediatric heart transplant population: A study of the international pediatric IVUS consortium. Clin Transplant. 2020:e13981.
Kindel SJ, Hsu HH, Hussain T, Johnson JN, McMahon CJ, Kutty S (2017) Multimodality Noninvasive Imaging in the Monitoring of Pediatric Heart Transplantation. J Am Soc Echocardiogr 30:859–870
Zoeller BB, Miyamoto SD, Younoszai AK, Landeck BF 2nd (2016) Longitudinal strain and strain rate abnormalities precede invasive diagnosis of transplant coronary artery vasculopathy in pediatric cardiac transplant patients. Pediatr Cardiol 37(4):656–662
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest to disclose, no research involving human participants or animals. Informed verbal consent was obtained from the patient or guardian prior to performing the echocardiogram.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pradhan, S., Mullikin, A., Zang, H. et al. Decreased Global Myocardial Work Efficiency Correlates with Coronary Vasculopathy in Pediatric Heart Transplant Patients. Pediatr Cardiol 43, 515–524 (2022). https://doi.org/10.1007/s00246-021-02748-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02748-1