Abstract
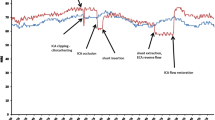
Pediatric cardiac interventions via percutaneous common carotid artery (CCA) access have been shown to be safe and effective. However, the impact of placement of a sheath in the carotid artery for interventions on cerebral perfusion is unknown. In this study we used cerebral near-infrared spectroscopy (NIRS) to analyze the effects of percutaneous CCA access for cardiac interventions on cerebral perfusion. This study is a retrospective chart review carried out at a tertiary care center on all pediatric patients who underwent percutaneous cardiac catheterization via carotid artery access from January 2010 to January 2020. All patients who had ipsilateral NIRS recorded on the side of carotid artery access were included. Patients with only partial or no ipsilateral NIRS data were excluded. The primary outcome measure was the change in NIRS upon CCA access; the mean NIRS for 15 min before obtaining access was compared to the mean NIRS during the procedure and to the mean NIRS 15 min after removal of the CCA sheath. We hypothesized that there would be a significant drop in NIRS values on the side of CCA access. There were 48 catheterizations in the study period where percutaneous CCA was accessed. Of those, 21 catheterizations had complete data and were included in the study. 13 (62%) were of males. The median age was 23 days (IQR 7–79). The indications for CCA access were patent ductus arteriosus stent implantation (n = 13; 62%), aortic valvuloplasty (n = 5; 24%), balloon angioplasty of coarctation of aorta (n = 2; 10%), and renal artery angioplasty (n = 1; 4%). In 16 patients (72%), the left common carotid artery was accessed. The median weight of the patients was 3.3 kg (IQR 2.8–2.9). The most common sheath size used was 4F, in 16 patients (72%). The mean NIRS prior to the procedure was 67 ± 15%, during the procedure was 68 ± 20%, and after removal of sheath was 68 ± 21%. Paired t test of cerebral NIRS before, during, and after the procedure showed no significant change with CCA access (P = 0.08). No patient in the series had a documented neurologic deficit following the procedure. Percutaneous CCA access was not associated with a decrease in NIRS on the side of the access during the procedure, suggesting there was no significant acute change in cerebral perfusion with CCA access.


Similar content being viewed by others
References
Justino H, Petit C (2016) Percutaneous common carotid artery access for pediatric interventional cardiac catheterization. Circ: Cardiovasc Interv 9(4):e003003
Azzolina G, Eufrate SA, Allella A (1973) New approach to catheterization of the heart in infants and children. Br Heart J 35(6):643–646
Choudhry S, Balzer D, Murphy J, Nicolas R, Shahanavaz S (2016) Percutaneous carotid artery access in infants < 3 months of age. Catheter Cardiovasc Interv 87(4):757–761
Ligon et al. (2018) Angiographic follow-up of infants and children undergoing percutaneous carotid artery interventions. Catheter Cardiovasc Interv 91(7):1301–1306
Ejike JC, Schenkman KA, Seidel K, Ramamoorthy C, Roberts JS (2006) Cerebral oxygenation in neonatal and pediatric patients during veno-arterial extracorporeal life support. Pediatr Crit Care Med 7(2):154–158
Cabrera AG, Kibler KK, Blaine Easley R, Goldsworthy M, Shekerdemian LS, Andropoulos DB et al (2018) Elevated arterial blood pressure after superior cavo-pulmonary anastomosis is associated with elevated pulmonary artery pressure and cerebrovascular dysautoregulation. Pediatr Res 84(3):356–361
Desmond FA, Namachivayam S (2016) Does near-infrared spectroscopy play a role in paediatric intensive care? BJA Educ 16(8):281–285
Andropoulos DB, Stayer SA, McKenzie ED, Fraser CD (2003) Novel cerebral physiologic monitoring to guide low-flow cerebral perfusion during neonatal aortic arch reconstruction. J Thorac Cardiovasc Surg 125(3):491–499
Kussman BD, Wypij D, Laussen PC, Soul JS, Bellinger DC, Dinardo JA et al (2010) Relationship of intraoperative cerebral oxygen saturation to neurodevelopmental outcome and brain MRI at one year of age in infants undergoing biventricular repair. Circulation 122(3):245–254
Kurth CD, Levy WJ, McCann J (2016) Near-infrared spectroscopy cerebral oxygen saturation thresholds for hypoxia–ischemia in piglets. J Cereb Blood Flow Metab 22(3):335–341
Dent CL, Spaeth JP, Jones BV, Schwartz SM, Glauser TA, Hallinan B et al (2006) Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 131(1):190–197
Ligon RA, Ooi YK, Kim DW, Vincent RN, Petit CJ (2017) Intervention on surgical systemic-to-pulmonary artery shunts: carotid versus femoral access. JACC: Cardiovasc Interv 10(17):1738–1744
Kurth CD, McCann JC, Wu J, Miles L, Loepke AW (2009) Cerebral oxygen saturation-time threshold for hypoxic-ischemic injury in piglets. Anesth Analg 108(4):1268–1277
Hagino I, Anttila V, Zurakowski D, Duebener LF, Lidov HGW, Jonas RA (2005) Tissue oxygenation index is a useful monitor of histologic and neurologic outcome after cardiopulmonary bypass in piglets. J Thorac Cardiovasc Surg 130(2):384–392
Dent CL, Spaeth JP, Jones BV, Schwartz SM, Glauser TA, Hallinan B et al (2005) Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 130(6):1523–1530
Borghi A, Borghi A, Agnoletti G, Agnoletti G, Poggiani C, Poggiani C (2001) Surgical cutdown of the right carotid artery for aortic balloon valvuloplasty in infancy: midterm follow-up. Pediatr Cardiol 22(3):194–197
Davenport JJ, Lam L, Whalen-Glass R, Nykanen DG, Burke RP, Hannan R et al (2008) The successful use of alternative routes of vascular access for performing pediatric interventional cardiac catheterization. Catheter Cardiovasc Interv 72(3):392–398
Buesing KA, Kilian AK, Schaible T, Loff S, Sumargo S, Neff KW (2007) Extracorporeal membrane oxygenation in infants with congenital diaphragmatic hernia: follow-up MRI evaluating carotid artery reocclusion and neurologic outcome. Am J Roentgenol 188(6):1636–1642
Henzler C, Zöllner FG, Weis M, Zimmer F, Schoenberg SO, Zahn K et al (2017) Cerebral perfusion after repair of congenital diaphragmatic hernia with common carotid artery occlusion after ECMO therapy. In Vivo 31(4):557–564
Funding
No financial disclosures.
Author information
Authors and Affiliations
Contributions
SL collected the data and wrote the manuscript. AMQ, HJ, and EM contributed significantly on conceptualization and writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lahiri, S., Qureshi, A.M., Justino, H. et al. Percutaneous Common Carotid Artery Access for Cardiac Interventions in Infants Does Not Acutely Change Cerebral Perfusion. Pediatr Cardiol 43, 104–109 (2022). https://doi.org/10.1007/s00246-021-02697-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02697-9