Abstract
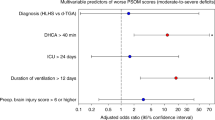
The aim of this study is to describe the clinical characteristics, perioperative course and neuroimaging abnormalities of infants with congenital heart disease (CHD) undergoing heart surgery without deep hypothermic circulatory arrest (DHCA) and identify variables associated with neurological outcome. Infants with CHD undergoing open-heart surgery without DHCA between 2009 and 2017 were identified from a cardiac surgery database. Full-term infants < 10 weeks of age at the time of surgery who had both a pre- and postoperative brain magnetic resonance imaging exam (MRI) were included. Clinical characteristics and perioperative variables were collected from the electronic medical record. Brain Injury Scores (BIS) were assigned to pre- and postoperative brain MRIs. Variables were examined for association with neurological outcome at 12 months of age or greater. Forty-two infants were enrolled in the study, of whom 69% (n = 29) had a neurological assessment ≥ to 12 months of age. Adverse neurological outcome was associated with longer intensive care unit (ICU) stay (P = 0.003), lengthier mechanical ventilation (P = 0.031), modified Blalock-Taussig (MBT) shunt procedure (P = 0.005) and postoperative seizures (P = 0.005). Total BIS scores did not predict outcome but postoperative infarction and/or intraparenchymal hemorrhage (IPH) was associated with worse outcome by multivariable analysis (P = 0.018). Infants with CHD undergoing open-heart surgery without DHCA are at increased risk of worse neurological outcome when their ICU stay is prolonged, mechanical ventilation is extended, MBT shunt is performed or when postoperative seizures are present. Cerebral infarctions and IPH on postoperative MRI are also associated with worse outcome.
Similar content being viewed by others
Data Availability
Data sharing was not included in the IRB approval for this study. Supplemental tables are included to maximize transparency.
Code Availability
Not applicable.
References
van der Linde D, Konings EEM, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJM et al (2011) Birth prevalence of congenital heart disease worldwide. J Am Coll Cardiol 58(21):2241–2247
Bernier P-L, Stefanescu A, Samoukovic G, Tchervenkov CI (2010) The challenge of congenital heart disease worldwide: epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 13(1):26–34
Liu Y, Chen S, Zühlke L, Black GC, Choy M, Li N et al (2019) Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol 48(2):455–463
Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW et al (2012) Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management a scientific statement from the american heart association. Circulation 126(9):1143–1172
Latal B (2016) Neurodevelopmental outcomes of the child with congenital heart disease. Clin Perinatol 43(1):173–185
Boneva RS, Botto LD, Moore CA, Yang Q, Correa A, Erickson JD (2001) Mortality associated with congenital heart defects in the United States: trends and racial disparities, 1979–1997. Circulation 103(19):2376–2381
Holst KA, Said SM, Nelson TJ, Cannon BC, Dearani JA (2017) Current interventional and surgical management of congenital heart disease: specific focus on valvular disease and cardiac arrhythmias. Circ Res 120(6):1027–1044
Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, Dendukuri N, Kaouache M (2014) Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation 130(9):749–756
Mazor Dray E, Marelli AJ (2015) Adult congenital heart disease. Cardiol Clin 33(4):503–512
Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A (2013) Temporal trends in survival among infants with critical congenital heart defects. Pediatrics 131(5):e1502–e1508
Limperopoulos C, Majnemer A, Shevell MI, Rosenblatt B, Rohlicek C, Tchervenkov C (2000) Neurodevelopmental status of newborns and infants with congenital heart defects before and after open heart surgery. J Pediatr 137(5):638–645
Wernovsky G, Shillingford AJ, Gaynor JW (2005) Central nervous system outcomes in children with complex congenital heart disease. Curr Opin Cardiol 20(2):94–99
Limperopoulos C, Majnemer A, Shevell MI, Rosenblatt B, Rohlicek C, Tchervenkov C et al (2001) Functional limitations in young children with congenital heart defects after cardiac surgery. Pediatrics 108(6):1325–1331
Gaynor JW, Wernovsky G, Jarvik GP, Bernbaum J, Gerdes M, Zackai E et al (2007) Patient characteristics are important determinants of neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery. J Thorac Cardiovasc Surg 133(5):1344-1353.e3
Hövels-Gürich HH (2016) Factors influencing neurodevelopment after cardiac surgery during infancy. Front Pediatr 4:137. https://doi.org/10.3389/fped.2016.00137
Naef N, Liamlahi R, Beck I, Bernet V, Dave H, Knirsch W et al (2017) Neurodevelopmental profiles of children with congenital heart disease at school age. J Pediatr 188:75–81
Rivkin MJ, Watson CG, Scoppettuolo LA, Wypij D, Vajapeyam S, Bellinger DC et al (2013) Adolescents with d-transposition of the great arteries repaired in early infancy demonstrate reduced white matter microstructure associated with clinical risk factors. J Thorac Cardiovasc Surg 146(3):543-549.e1
Wernovsky G, Licht D (2016) Neurodevelopmental outcomes in children with congenital heart disease—what can we impact? Pediatr Crit Care Med 17(8):232–242
Morton PD, Ishibashi N, Jonas RA (2017) Neurodevelopmental abnormalities and congenital heart disease: insights into altered brain maturation. Circ Res 120(6):960–977
Kuhn VA, Carpenter JL, Zurakowski D, Reitz JG, Tague L, Donofrio MT et al (2021) Determinants of neurological outcome in neonates with congenital heart disease following heart surgery. Pediatr Res 89:1283–1290. https://doi.org/10.1038/s41390-020-1085-1
Wypij D, Newburger JW, Rappaport LA, duPlessis AJ, Jonas RA, Wernovsky G et al (2003) The effect of duration of deep hypothermic circulatory arrest in infant heart surgery on late neurodevelopment: the boston circulatory arrest trial. J Thorac Cardiovasc Surg 126(5):1397–1403
Andropoulos DB, Hunter JV, Nelson DP, Stayer SA, Stark AR, McKenzie ED et al (2010) Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J Thorac Cardiovasc Surg 139(3):543–556
Heinrichs AKM, Holschen A, Krings T, Messmer BJ, Schnitker R, Minkenberg R et al (2014) Neurologic and psycho-intellectual outcome related to structural brain imaging in adolescents and young adults after neonatal arterial switch operation for transposition of the great arteries. J Thorac Cardiovasc Surg 148(5):2190–2199
Andropoulos DB, Ahmad HB, Haq T, Brady K, Stayer SA, Meador MR et al (2014) The association between brain injury, perioperative anesthetic exposure, and 12-month neurodevelopmental outcomes after neonatal cardiac surgery: a retrospective cohort study. Paediatr Anaesth 24(3):266–274
Murray DM, Boylan GB, Ali I, Ryan CA, Murphy BP, Connolly S (2008) Defining the gap between electrographic seizure burden, clinical expression and staff recognition of neonatal seizures. Arch Dis Child Fetal Neonatal Ed 93(3):F187–F191
Childs AM, Ramenghi LA, Cornette L, Tanner SF, Arthur RJ, Martinez D et al (2001) Cerebral maturation in premature infants: quantitative assessment using MR imaging. AJNR Am J Neuroradiol 22(8):1577–1582
deVeber GA, MacGregor D, Curtis R, Mayank S (2000) Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J Child Neurol 15(5):316–324
Kitchen L, Westmacott R, Friefeld S, MacGregor D, Curtis R, Allen A et al (2012) The pediatric stroke outcome measure: a validation and reliability study. Stroke 43(6):1602–1608
Felling RJ, Rafay MF, Bernard TJ, Carpenter JL, Dlamini N, Hassanein SMA et al (2020) Predicting recovery and outcome after pediatric stroke: results from the international pediatric stroke study. Ann Neurol 87(6):840–852
Beers SR, Wisniewski SR, Garcia-Filion P, Tian Y, Hahner T, Berger RP et al (2012) Validity of a pediatric version of the glasgow outcome scale-extended. J Neurotrauma 29(6):1126–1139
Dent CL, Spaeth JP, Jones BV, Schwartz SM, Glauser TA, Hallinan B et al (2005) Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 130(6):1523–1530
McQuillen PS, Barkovich AJ, Hamrick SEG, Perez M, Ward P, Glidden DV et al (2007) Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke 38(2):736–741
Dimitropoulos A, McQuillen PS, Sethi V, Moosa A, Chau V, Xu D et al (2013) Brain injury and development in newborns with critical congenital heart disease. Neurology 81(3):241–248
Kelly CJ, Arulkumaran S, Tristão Pereira C, Cordero-Grande L, Hughes EJ, Teixeira RPAG et al (2019) Neuroimaging findings in newborns with congenital heart disease prior to surgery: an observational study. Arch Dis Child 104(11):1042–1048
Mahle WT, Tavani F, Zimmerman RA, Nicolson SC, Galli KK, Gaynor JW et al (2002) An MRI study of neurological injury before and after congenital heart surgery. Circulation 106(12 Suppl 1):I109-114
Chen J, Zimmerman RA, Jarvik GP, Nord AS, Clancy RR, Wernovsky G et al (2009) Perioperative stroke in infants undergoing open heart operations for congenital heart disease. Ann Thorac Surg 88(3):823–829
Mebius MJ, Kooi EMW, Bilardo CM, Bos AF (2017) Brain injury and neurodevelopmental outcome in congenital heart disease: a systematic review. Pediatrics 140(1):e20164055
Beca J, Gunn JK, Coleman L, Hope A, Reed PW, Hunt RW et al (2013) New white matter brain injury after infant heart surgery is associated with diagnostic group and the use of circulatory arrest. Circulation 127(9):971–979
Claessens NHP, Algra SO, Ouwehand TL, Jansen NJG, Schappin R, Haas F et al (2018) Perioperative neonatal brain injury is associated with worse school-age neurodevelopment in children with critical congenital heart disease. Dev Med Child Neurol 60(10):1052–1058
Karl TR, Hall S, Ford G, Kelly EA, Brizard CPR, Mee RBB et al (2004) Arterial switch with full-flow cardiopulmonary bypass and limited circulatory arrest: neurodevelopmental outcome. J Thorac Cardiovasc Surg 127(1):213–222
Liamlahi R, Von Rhein M, Bührer S, Valsangiacomo Buechel ER, Knirsch W, Landolt MA et al (2014) Motor dysfunction and behavioural problems frequently coexist with congenital heart disease in school-age children. Acta Paediatr Int J Paediatr 103(7):752–758
Mussatto KA, Hoffmann RG, Hoffman GM, Tweddell JS, Bear L, Cao Y et al (2014) Risk and prevalence of developmental delay in young children with congenital heart disease. Pediatrics 133(3):e570–e577. https://doi.org/10.1542/peds.2013-2309
Sananes R, Manlhiot C, Kelly E, Hornberger LK, Williams WG, MacGregor D et al (2012) Neurodevelopmental outcomes after open heart operations before 3 months of age. Ann Thorac Surg 93(5):1577–1583
Bellinger DC, Wypij D, Kuban KCK, Rappaport LA, Hickey PR, Wernovsky G et al (1999) Developmental and neurological status of children at 4 years of age after heart surgery with hypothermic circulatory arrest or low-flow cardiopulmonary bypass. Circulation 100(5):526–532
Latal B, Helfricht S, Fischer JE, Bauersfeld U, Landolt MA (2009) Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: a systematic review. BMC Pediatr 9(1):6
Shillingford AJ, Glanzman MM, Ittenbach RF, Clancy RR, Gaynor JW, Wernovsky G (2008) Inattention, hyperactivity, and school performance in a population of school-age children with complex congenital heart disease. Pediatrics 121(4):e759–e767
Naim MY, Gaynor JW, Chen J, Nicolson SC, Fuller S, Spray TL et al (2015) Subclinical seizures identified by postoperative electroencephalographic monitoring are common after neonatal cardiac surgery. J Thorac Cardiovasc Surg 150(1):169–180
Clancy RR, McGaurn SA, Wernovsky G, Gaynor JW, Spray TL, Norwood WI et al (2003) Risk of seizures in survivors of newborn heart surgery using deep hypothermic circulatory arrest. Pediatrics 111(3):592–601
Clancy RR, Sharif U, Ichord R, Spray TL, Nicolson S, Tabbutt S et al (2005) Electrographic neonatal seizures after infant heart surgery. Epilepsia 46(1):84–90
Rappaport LA, Wypij D, Bellinger DC, Helmers SL, Holmes GL, Barnes PD et al (1998) Relation of seizures after cardiac surgery in early infancy to neurodevelopmental outcome. Circulation 97(8):773–779
Gorla S, Stumpf E, Sandhu SK (2018) The role of interventional cardiology in the management of thrombotic conditions in the pediatric population. In: Cardiovascular thrombus [Internet], Elsevier, Amsterdam. p 565–575. https://linkinghub.elsevier.com/retrieve/pii/B9780128126158000405. Accessed 2 Jun 2021
Gedicke M, Morgan G, Parry A, Martin R, Tulloh R (2010) Risk factors for acute shunt blockage in children after modified blalock-taussig shunt operations. Heart Vessels 25(5):405–409
Petrucci O, O’Brien SM, Jacobs ML, Jacobs JP, Manning PB, Eghtesady P (2011) Risk factors for mortality and morbidity after the neonatal blalock-taussig shunt procedure. Ann Thorac Surg 92(2):642–652
Garabedian CP, Joyce JJ, Ross-Ascuitto NT, Ascuitto RJ (1998) Innominate artery steal syndrome after stage I palliation for hypoplastic left heart syndrome. Pediatr Cardiol 19(6):458–462
Newburger J, Wypij D, Bellinger D, Du Plessis A, Kuban K, Rappaport L et al (2003) Length of stay after infant heart surgery is related to cognitive outcome at age 8 years. J Pediatr 143(1):67–73
Tabbutt S, Ghanayem N, Ravishankar C, Sleeper LA, Cooper DS, Frank DU et al (2012) Risk factors for hospital morbidity and mortality after the Norwood procedure: a report from the pediatric heart network single ventricle reconstruction trial. J Thorac Cardiovasc Surg 144(4):882–895
Funding
Internal funding.
Author information
Authors and Affiliations
Contributions
AK, CY, MTD, JGR, JLC: Substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article; final approval of the version to be published. DZ: Substantial contributions to conception and design, analysis and interpretation of data; drafting the article; final approval of the version to be published. LT: Substantial contributions to acquisition of data and final approval of the version to be published. RA-F: Substantial contributions to conception and design and final approval of the version to be published. JM, CL: Substantial contributions to acquisition of data, and analysis and interpretation of data; final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical Approval
Not applicable.
Consent to Participate
Waiver of consent was granted by the IRB.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kosiorek, A., Donofrio, M.T., Zurakowski, D. et al. Predictors of Neurological Outcome Following Infant Cardiac Surgery Without Deep Hypothermic Circulatory Arrest. Pediatr Cardiol 43, 62–73 (2022). https://doi.org/10.1007/s00246-021-02693-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02693-z