Abstract
Although De Vega annuloplasty is an important option for pediatric patients with functional tricuspid regurgitation (TR), little is known about its long-term results, including the future of the plicated annulus. We retrospectively reviewed our experience with pediatric patients who underwent the De Vega annuloplasty between 2005 and 2020. Tricuspid valve assessments were performed by transthoracic echocardiography. The targeted diameter of annular plication was 80 to 90% of normal tricuspid diameter, according to the patient's condition. The study included 55 patients (41 with biventricular physiology (group B), 14 with univentricular physiology (group U)) with a median follow-up of 5.0 years. Median age at operation was 5.0 years. There was one late death due to severe mitral regurgitation. Tricuspid valve reoperation was required in five patients and the 10-year freedom from reoperation was 91.9% for the entire cohort. The 10-year freedom from the composite adverse outcome of death, reoperation, and significant TR was 79.2% in group B versus 56.6% in group U (p = 0.034). TR grade significantly decreased after surgery (p < 0.001), without significant aggravation during the postoperative follow-up. No patients presented tricuspid stenosis. Mean Z-scores of annular diameter immediately after operation and at the latest follow-up were − 0.65 ± 0.56 versus − 0.47 ± 0.65 (p = 0.57). De Vega annuloplasty is a safe, efficient, and durable procedure for functional TR in pediatric patients including those with univentricular physiology, allowing adequate growth of the plicated annulus without the progression of tricuspid stenosis.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code Availability
Not applicable.
References
De Vega NG (1972) La anuloplastia selectiva, regulable y permanente. Una tècnica original para el tratamiento de la insuficiencia tricuspide. Rev Esp Cardiol 25:555–556
Kanter KR, Doelling NR, Fyfe DA et al (2001) De Vega Tricuspid annuloplasty for tricuspid regurgitation in children. Ann Thorac Surg 72:1344–1348
Kanter KR, Forbess JM, Fyfe DA et al (2004) De Vega tricuspid annuloplasty for systemic tricuspid regurgitation in children with univentricular physiology. J Heart Valve Dis 13:86–90
Baumgartner H, Hung J, Bermejo J et al (2009) Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr 22:1–23
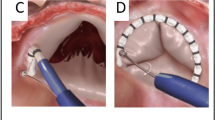
Antunes MJ (2003) De Vega annuloplasty of the tricuspid valve. Oper Tech Thorac Cardiovasc Surg 8:169–176
Calafiore AM, Mauro MD (2011) Tricuspid valve repair-indications and techniques: suture annuloplasty and band annuloplasty. Oper Tech Thorac Cardiovasc Surg 16:86–96. https://doi.org/10.1053/j.optechstcvs.2011.06.002
Parolari A, Barili F, Pilozzi A, Pacini D (2014) Ring or suture annuloplasty for tricuspid regurgitation? A meta-analysis review. Ann Thorac Surg 98:2255–2263. https://doi.org/10.1016/j.athoracsur.2014.06.100
McCarthy PM, Bhudia SK, Rajeswaran J et al (2004) Tricuspid valve repair: durability and risk factors for failure. J Thorac Cardiovasc Surg 127:674–685. https://doi.org/10.1016/j.jtcvs.2003.11.019
Nishimura RA, Otto CM, Bonow RO et al (2014) 2014 AHA/ACC Guideline for the management of patients with valvular heart disease. J Am Col Cardiol 63:e57-185. https://doi.org/10.1161/cir.0000000000000031
Dreyfus GD, Corbi PJ, Chan KMJ, Bahrami T (2005) Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg 79:127–132. https://doi.org/10.1016/j.athoracsur.2004.06.057
Honjo O, Atlin CR, Mertens L et al (2011) Atrioventricular valve repair in patients with functional single-ventricle physiology: impact of ventricular and valve function and morphology on survival and reintervention. J Thorac Cardiovasc Surg 142:326–335. https://doi.org/10.1016/j.jtcvs.2010.11.060
Stamm C, Anderson RH, Ho SY (1997) The morphologically tricuspid valve in hypoplastic left heart syndrome. Eur J Cardiothorac Surg 12:587–592. https://doi.org/10.1016/S1010-7940(97)00184-X
Ono M, Cleuziou J, von Ohain JP et al (2018) Atrioventricular valve regurgitation in patients undergoing total cavopulmonary connection: impact of valve morphology and underlying mechanisms on survival and reintervention. J Thorac Cardiovasc Surg 155:701–709. https://doi.org/10.1016/j.jtcvs.2017.08.122
De Vega NG (2013) Yesterday’s future: the gap between where we are now and where we were supposed to be. Eur J Cardiothorac Surg 43:66. https://doi.org/10.1093/ejcts/ezs305
Tsang VT, Jansen HA (2014) The “Systemic” tricuspid valeve in hypoplastic left heart syndrome. In: Giamberti A, Chessa M (eds) The tricspid valve in congenital heart disease. Springer, Milan
Acknowledgements
The authors are grateful to N. Fujiwara for his constructive suggestions on statistical analysis.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
YY conceived and designed the study, analyzed the data, wrote the manuscript, and revised it. KN, FM, and SI collected and analyzed the data and helped in revision of manuscript. KH helped in the final drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical Approval
This study was conducted with the approval of the institutional review board of Saitama Children's Medical Center (#2020-05-004, January 14, 2021).
Disclosure
All authors have nothing to disclose.
Informed Consent
A written informed consent was obtained from one or both parents of all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamamoto, Y., Nomura, K., Murayama, F. et al. De Vega Tricuspid Annuloplasty for Pediatric Patients: Growth Potential of the Plicated Annulus. Pediatr Cardiol 42, 1854–1861 (2021). https://doi.org/10.1007/s00246-021-02679-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02679-x