Abstract
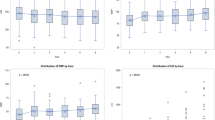
The use of vasopressin has been increased in recent years in children after congenital heart surgery. However, there is limited information regarding its effects on cardiac output, systemic oxygen delivery, and myocardial energetics. The purpose of this study is to characterize the effects of vasopressin infusions on hemodynamics and systemic oxygen delivery in children with congenital heart disease. A retrospective, single-center study of patients with congenital heart disease who received vasopressin infusions in a pediatric cardiac intensive care unit between January 2019 and May 2020. The measured values collected for study were systolic and diastolic blood pressure, heart rate, arterial oxygen saturation as determined by pulse oximetry, arterial pH, arterial partial pressure of oxygen, arterial partial pressure of carbon dioxide, serum lactate, serum sodium, and renal and cerebral oximetry based on near-infrared spectroscopy. The calculated values for this study were the difference between arterial and NIRS oximetry, the reno-cerebral near-infrared spectroscopy gradient and the vasoinotrope score. A Wilcoxon signed-rank test was utilized to compare values of paired continuous variables before and after initiation of the vasopressin infusion. Correlations were assessed using Spearman correlation analyses and stepwise regressions were completed. A total of 26 vasopressin infusions among 20 unique patients were included in the final analyses. Of these 26 vasopressin infusions, 18 were in patients with biventricular circulation and 8 were in patients with functionally univentricular circulation. The median vasopressin infusion dose at initiation was 0.4 (0.1–1) milliunits/kg/min. For the entire cohort 2 h after the initiation of vasopressin, systolic blood pressure increased to 8.4 mmHg, p < 0.01, but no significant correlation was found to markers of systemic oxygen delivery. Similar results were obtained when only those with biventricular circulation were considered. Those with functionally univentricular circulation were not found to have any statistically significant rise in blood pressure. Vasopressin infusions appear to statistically significantly increase systolic blood pressure in children with congenital heart disease who have a biventricular but not functionally univentricular circulation. Even when an increase in systolic blood pressure is present, systemic oxygen delivery did not improve.
Similar content being viewed by others
Data Availability
All data and materials, as well as software application, support our published claims and comply with field standards.
References
Loomba RS, Flores S (2019) Use of vasoactive agents in postoperative pediatric cardiac patients: insights from a national database. Congenit Heart Dis 14(6):1176–1184
Farias JS et al (2021) Effects of vasopressin infusion after pediatric cardiac surgery: a meta-analysis. Pediatr Cardiol 42(2):225–233
Wernovsky G et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92(8):2226–2235
Li J et al (2006) Adverse effects of dopamine on systemic hemodynamic status and oxygen transport in neonates after the Norwood procedure. J Am Coll Cardiol 48(9):1859–1864
Dhillon S et al (2015) Clinical hemodynamic parameters do not accurately reflect systemic oxygen transport in neonates after the Norwood procedure. Congenit Heart Dis 10(3):234–239
Zhang G et al (2011) Aortic atresia is associated with an inferior systemic, cerebral, and splanchnic oxygen-transport status in neonates after the Norwood procedure. Eur J Cardiothorac Surg 39(3):e13-21
Tweddell JS et al (2000) Patients at risk for low systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 69(6):1893–1899
Tweddell JS et al (1999) Phenoxybenzamine improves systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 67(1):161–167; discussion 167–168
Naito Y et al (2010) Factors affecting systemic oxygen delivery after Norwood procedure with Sano modification. Ann Thorac Surg 89(1):168–173
Yamamoto M et al (2021) The relationships of cerebral and somatic oxygen saturation with physiological parameters in pediatric cardiac surgery with cardiopulmonary bypass: analysis using the random-effects model. Pediatr Cardiol 42(2):370–378
Li J et al (2007) Profiles of hemodynamics and oxygen transport derived by using continuous measured oxygen consumption after the Norwood procedure. J Thorac Cardiovasc Surg 133(2):441–448
Wardle SP, Yoxall CW, Weindling AM (2000) Determinants of cerebral fractional oxygen extraction using near infrared spectroscopy in preterm neonates. J Cereb Blood Flow Metab 20(2):272–279
Goonasekera CDA, Carcillo JA, Deep A (2018) Oxygen delivery and oxygen consumption in pediatric fluid refractory septic shock during the first 42 h of therapy and their relationship to 28-day outcome. Front Pediatr 6:314
Ranucci M et al (2010) Central venous oxygen saturation and blood lactate levels during cardiopulmonary bypass are associated with outcome after pediatric cardiac surgery. Crit Care 14(4):R149
Houwink AP et al (2016) The association between lactate, mean arterial pressure, central venous oxygen saturation and peripheral temperature and mortality in severe sepsis: a retrospective cohort analysis. Crit Care 20:56
Irschik S et al (2020) Direct postoperative protein S100B and NIRS monitoring in infants after pediatric cardiac surgery enrich early mortality assessment at the PICU. Heart Lung 49(6):731–736
Duke TD, Butt W, South M (1997) Predictors of mortality and multiple organ failure in children with sepsis. Intensive Care Med 23(6):684–692
Agrawal A et al (2012) Intravenous arginine vasopressin infusion in refractory vasodilatory shock: a clinical study. Indian J Pediatr 79(4):488–493
Burton GL et al (2011) The use of arginine vasopressin in neonates following the Norwood procedure. Cardiol Young 21(5):536–544
Lu Z et al (2018) Vasopressin in vasodilatory shock for both left and right heart anomalous pediatric patients after cardiac surgery. Shock 50(2):173–177
Mastropietro CW et al (2008) Arginine vasopressin to manage hypoxemic infants after stage I palliation of single ventricle lesions. Pediatr Crit Care Med 9(5):506–510
Rosenzweig EB et al (1999) Intravenous arginine-vasopressin in children with vasodilatory shock after cardiac surgery. Circulation 100(19 Suppl):II182–II186
Iliopoulos I et al (2017) Arginine-vasopressin therapy in hypotensive neonates and infants after cardiac surgery: response is unrelated to baseline ventricular function. Cardiol Young 27(6):1031–1040
Alten JA et al (2012) Early initiation of arginine vasopressin infusion in neonates after complex cardiac surgery. Pediatr Crit Care Med 13(3):300–304
Bigelow AM et al (2019) Safety and efficacy of vasopressin after fontan completion: a randomized pilot study. Ann Thorac Surg 108(6):1865–1874
Davalos MC et al (2013) Hyponatremia during arginine vasopressin therapy in children following cardiac surgery. Pediatr Crit Care Med 14(3):290–297
Kumar TK et al (2016) Vasopressin after the fontan operation. World J Pediatr Congenit Heart Surg 7(1):43–48
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RSL, SF, and RAB contributed to the study conception and design. Material preparation, data collection, and analysis were performed by CC, KS, MV, and FS. The first draft of the manuscript was written by RSL and SF. RAB commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The Study have been approved by the appropriate institutional ethics committee and have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Loomba, R.S., Culichia, C., Schulz, K. et al. Acute Effects of Vasopressin Arginine Infusion in Children with Congenital Heart Disease: Higher Blood Pressure Does Not Equal Improved Systemic Oxygen Delivery. Pediatr Cardiol 42, 1792–1798 (2021). https://doi.org/10.1007/s00246-021-02667-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02667-1